Abstract
Purpose
The aim of this study was to describe radiological imaging findings of a complicated sinusitis, which should raise the suspicion of rhino-orbital-cerebral mucormycosis as being the underlying cause.
Methods
In this retrospective analysis, we describe the cases and imaging findings of 8 patients with proven mucormycosis. These patients presented mostly with new facial or orbital swelling and were referred for imaging to our institution. Magnetic resonance imaging and computed tomography images were classified as abnormal or normal with respect to orbital, paranasal and cerebral signal results. Special emphasis was placed on the distribution of the signal abnormalities regarding involvement of the skull base and the cavernous sinus.
Results
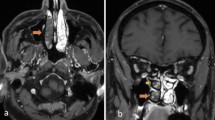
Out of a pool of 43 patients with colonization or proven Mucorales infection at different sites of the body, we identified 8 patients with infiltration of the midface and skull base. Unexpectedly seven out of the eight patients with abnormal findings of the paranasal sinuses and the adjacent tissues showed no bony sinus wall destruction. Of the eight patients seven showed inflammatory changes involving the infratemporal fossa and facial/periorbital tissues, three of the eight patients suffered from fungal invasion of the cavernous sinus and the carotid artery and one of the eight patients had a local infection of the hard palate only.
Conclusion
Imaging findings of inflammatory tissue infiltration adjacent to the paranasal sinuses with possible extension into the pterygopalatine fossa, infratemporal fossa and orbit or the cavernous sinus should raise the suspicion of a mucormycosis, especially in immunocompromised patients.




Similar content being viewed by others
References
Castón-Osorio JJ, Rivero A, Torre-Cisneros J. Epidemiology of invasive fungal infection. Int J Antimicrob Agents. 2008;32(Suppl 2):S103–9.
Long B, Koyfman A. Mucormycosis: what emergency physicians need to know? Am J Emerg Med. 2015;33(12):1823–5.
Walsh TJ, Skiada A, Cornely OA, Roilides E, Ibrahim A, Zaoutis T, Groll A, Lortholary O, Kontoyiannis DP, Petrikkos G. Development of new strategies for early diagnosis of mucormycosis from bench to bedside. Mycoses. 2014;57(Suppl 3):2–7.
Riley TT, Muzny CA, Swiatlo E, Legendre DP. Breaking the mold: a review of mucormycosis and current pharmacological treatment options. Ann Pharmacother. 2016;50(9):747–57.
Safder S, Carpenter JS, Roberts TD, Bailey N. The “black turbinate” sign: an early MR imaging finding of nasal mucormycosis. AJNR Am J Neuroradiol. 2010;31(4):771–4.
Vironneau P, Kania R, Morizot G, Elie C, Garcia-Hermoso D, Herman P, Lortholary O, Lanternier F. French Mycosis Study Group. Local control of rhino-orbito-cerebral mucormycosis dramatically impacts survival. Clin Microbiol Infect. 2014;20(5):336–9.
Kursun E, Turunc T, Demiroglu YZ, Alışkan HE, Arslan AH. Evaluation of 28 cases of mucormycosis. Mycoses. 2015;58(2):82–7.
Son JH, Lim HB, Lee SH, Yang JW, Lee SB. Early differential diagnosis of rhino-orbito-cerebral mucormycosis and bacterial orbital cellulitis: based on computed tomography findings. PLoS One. 2016;11(8):e0160897.
Mostafa BE, el Fiki L, Sallam FA. Complicated fungal sinusitis. Clinical and therapeutic aspects. Rev Laryngol Otol Rhinol (Bord). 2001;122(1):37–42.
Riechelmann H. Fungal sinusitis. Laryngorhinootologie. 2011;90(6):82–4.
Cunnane MB, Curtin HD. Imaging of orbital disorders. Handb Clin Neurol. 2016;135:659–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P. Raab, L. Sedlacek, S. Buchholz, S. Stolle and H. Lanfermann declare that they have no competing interests.
Ethical standards
All procedures described in this manuscript were carried out in accordance with national law and the Helsinki Declaration from 1964 (in its present revised form). This retrospective analysis was approved by the local ethics committee and the patients consented to the scientific anonymized use of their medical data.
Rights and permissions
About this article
Cite this article
Raab, P., Sedlacek, L., Buchholz, S. et al. Imaging Patterns of Rhino-Orbital-Cerebral Mucormycosis in Immunocompromised Patients. Clin Neuroradiol 27, 469–475 (2017). https://doi.org/10.1007/s00062-017-0629-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-017-0629-1