Abstract
Objective
The aim of this study was to investigate the value of initial serum N-terminal pro-brain natriuretic peptide (NT-proBNP) concentrations in ST-segment elevation myocardial infarction (STEMI) patients for predicting ST-segment resolution (STR) after primary percutaneous coronary intervention (pPCI).
Patients and methods
Consecutive STEMI patients (n = 218) who underwent pPCI were assigned to an STR group (≥ 50 % resolution) or a non-STR group (< 50 % resolution). All patients were followed up for 12 months, and major adverse cardiac events were recorded. Data related to the pPCI procedure, biochemical parameters, and cardiac markers were compared between the two groups. Predictive factors of non-STR were also identified.
Results
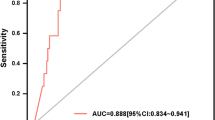
STR at 180 min after pPCI occurred in 202 patients (92.7 %). Compared to the STR group, patients in the non-STR group had a significantly lower left ventricular ejection fraction, a larger left ventricular end-diastolic dimension, and significantly higher serum concentrations of glycosylated hemoglobin and NT-proBNP. Multivariate logistic regression analysis indicated that a high serum NT-proBNP level in STEMI patients on hospital admission was the only independent predictive factor of non-STR after pPCI. An NT-proBNP concentration of ≥ 2,563.6 pg/ml had a sensitivity of 81.2 % and a specificity of 65.8 %.
Conclusions
Serum NT-proBNP concentrations in STEMI patients on hospital admission were useful in predicting non-STR after pPCI.
Zusammenfassung
Ziel
Ziel war die Untersuchung der prognostischen Aussagekraft der Konzentration des initialen n-terminalen „pro-brain natriuretic peptide“ (NT-proBNP) im Serum bei Patienten mit ST-Strecken-Hebungs-Infarkt (STEMI) hinsichtlich der Rückbildung der ST-Stecken-Hebung (STR) nach primärer perkutaner Koronarintervention (pPCI).
Patienten und Methoden
Aufeinanderfolgende STEMI-Patienten (n = 218), bei denen eine pPCI erfolgte, wurden der STR-Gruppe (≥ 50 % Rückbildung) oder der Nicht-STR-Gruppe (< 50 % Rückbildung) zugeteilt. Alle Patienten wurden 12 Monate lang nachbeobachtet, dabei wurden wesentliche unerwünschte kardiale Ereignisse dokumentiert. Es wurden Daten der pPCI, biochemische Parameter und kardiale Marker zwischen den beiden Gruppen verglichen. Prädiktive Faktoren für Nicht-STR wurden ebenfalls erfasst.
Ergebnisse
Eine STR trat bei 202 Patienten (92,7 %) 180 min nach pPCI auf. Im Vergleich zur STR-Gruppe wiesen die Patienten in der Nicht-STR-Gruppe eine signifikant niedrigere linksventrikuläre Ejektionsfraktion (LVEF), einen größeren linksventrikulären enddiastolischen Durchmesser (LVEDD) und signifikant höhere Serumkonzentrationen sowohl von glykosyliertem Hämoglobin (HBA1C) als auch von NT-proBNP auf. Die multivariate logistische Regressionsanalyse ergab, dass ein hoher Serum-NT–proBNP-Spiegel bei STEMI-Patienten bei Aufnahme ins Krankenhaus den einzigen unabhängigen prädiktiven Faktor für eine Nicht-STR nach pPCI darstellte. Eine NT-proBNP-Konzentration ≥ 2563,6 pg/ml wies eine Sensitivität von 81,2 % und eine Spezifität von 65,8 % auf.
Schlussfolgerung
Die Serum-NT-proBNP-Konzentrationen von STEMI-Patienten bei stationärer Aufnahme besaßen prädiktive Aussagekraft für eine Nicht-STR nach pPCI.


Similar content being viewed by others
References
Keeley EC, Hillis LD (2007) Primary PCI for myocardial infarction with ST-segment elevation. N Engl J Med 356:47–54
Wong DT, Puri R, Richardson JD, Worthley MI, Worthley SG (2013) Myocardial ‘no-reflow’–diagnosis, pathophysiology and treatment. Int J Cardiol 167:1798–1806
Santoro GM, Valenti R, Buonamici P et al (1998) Relation between ST-segment changes and myocardial perfusion evaluated by myocardial contrast echocardiography in patients with acute myocardial infarction treated with direct angioplasty. Am J Cardiol 82:932–937
de Lemos JA, Antman EM, Giugliano RP et al (2000) ST-segment resolution and infarct-related artery patency and flow after thrombolytic therapy. Thrombolysis in Myocardial Infarction (TIMI) 14 investigators. Am J Cardiol 85:299–304
de Lemos JA, Braunwald E (2001) ST segment resolution as a tool for assessing the efficacy of reperfusion therapy. J Am Coll Cardiol 38:1283–1294
Balian V, Galli M, Repetto S et al (2005) Intracoronary ST segment evolution during primary coronary stenting predicts infarct zone recovery. Catheter Cardiovasc Interv 64:53–60
Shuja ur R, Sheikh S, Nazeer M (2008) ST segment resolution post MI–a predictor of better outcomes. J Pak Med Assoc 58:283–286
Matetzky S, Novikov M, Gruberg L et al (1999) The significance of persistent ST elevation versus early resolution of ST segment elevation after primary PTCA. J Am Coll Cardiol 34:1932–1938
Nicolau JC, Maia LN, Vitola J et al (2003) ST-segment resolution and late (6-month) left ventricular remodeling after acute myocardial infarction. Am J Cardiol 91:451–453
Araszkiewicz A, Lesiak M, Grajek S, Mularek-Kubzdela T, Popiel M, Cieslinski A (2005) [Value of ST-segment elevation resolution after primary coronary angioplasty in predicting early and late left ventricular function in patients with anterior acute myocardial infarction]. Pol Merkur Lekarski 19:16–19
de Lemos JA, Antman EM, Giugliano RP et al (2000) Comparison of a 60- versus 90-minute determination of ST-segment resolution after thrombolytic therapy for acute myocardial infarction. In TIME-II Investigators. Intravenous nPA for Treatment of Infarcting Myocardium Early-II. Am J Cardiol 86:1235–1237, a1235
Matetzky S, Freimark D, Chouraqui P et al (1998) The distinction between coronary and myocardial reperfusion after thrombolytic therapy by clinical markers of reperfusion. J Am Coll Cardiol 32:1326–1330
Bainey KR, Senaratne MP (2005) Is the outcomes of early ST-segment resolution after thrombolytic therapy in acute myocardial infarction always favorable? J Electrocardiol 38:354–360
Scirica BM, Sabatine MS, Morrow DA et al (2006) The role of clopidogrel in early and sustained arterial patency after fibrinolysis for ST-segment elevation myocardial infarction: the ECG CLARITY-TIMI 28 Study. J Am Coll Cardiol 48:37–42
Lorgis L, Zeller M, Dentan G et al (2008) Prognostic value of ST-segment resolution after rescue percutaneous coronary intervention. Data from the RICO survey. Catheter Cardiovasc Interv 71:607–612
Schroder K, Wegscheider K, Zeymer U, Tebbe U, Schroder R (2001) Extent of ST-segment deviation in a single electrocardiogram lead 90 min after thrombolysis as a predictor of medium-term mortality in acute myocardial infarction. Lancet 358:1479–1486
Zeymer U, Schroder K, Wegscheider K, Senges J, Neuhaus KL, Schroder R (2005) ST resolution in a single electrocardiographic lead: a simple and accurate predictor of cardiac mortality in patients with fibrinolytic therapy for acute ST-elevation myocardial infarction. Am Heart J 149:91–97
Mayr A, Mair J, Schocke M et al (2011) Predictive value of NT-pro BNP after acute myocardial infarction: relation with acute and chronic infarct size and myocardial function. Int J Cardiol 147:118–123
Khan SQ, Dhillon O, Kelly D et al (2008) Plasma N-terminal B-Type natriuretic peptide as an indicator of long-term survival after acute myocardial infarction: comparison with plasma midregional pro-atrial natriuretic peptide: the LAMP (Leicester Acute Myocardial Infarction Peptide) study. J Am Coll Cardiol 51:1857–1864
McCullough PA, Sandberg KR (2003) Sorting out the evidence on natriuretic peptides. Rev Cardiovasc Med 4(Suppl 4):S 13–S 19
Levine GN, Bates ER, Blankenship JC et al (2011) 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 124:2574–2609
Wijns W, Kolh P, Danchin N et al (2010) Guidelines on myocardial revascularization. Eur Heart J 31:2501–2555
Syed MA, Borzak S, Asfour A et al (2004) Single lead ST-segment recovery: a simple, reliable measure of successful fibrinolysis after acute myocardial infarction. Am Heart J 147:275–280
Ariyarajah V, Apiyasawat S, Spodick DH (2009) Formulaic quantification of echocardiographic left atrial volume. J Electrocardiol 42:258–264
Halkin A, Singh M, Nikolsky E et al (2005) Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: the CADILLAC risk score. J Am Coll Cardiol 45:1397–1405
Grabowski M, Filipiak KJ, Karpinski G et al (2004) Serum B-type natriuretic peptide levels on admission predict not only short-term death but also angiographic success of procedure in patients with acute ST-elevation myocardial infarction treated with primary angioplasty. Am Heart J 148:655–662
Jeong YH, Kim WJ, Park DW et al (2010) Serum B-type natriuretic peptide on admission can predict the ‘no-reflow’ phenomenon after primary drug-eluting stent implantation for ST-segment elevation myocardial infarction. Int J Cardiol 141:175–181
Vanderheyden M, Goethals M, Verstreken S et al (2004) Wall stress modulates brain natriuretic peptide production in pressure overload cardiomyopathy. J Am Coll Cardiol 44:2349–2354
Stone GW, Webb J, Cox DA et al (2005) Distal microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction: a randomized controlled trial. JAMA 293:1063–1072
Satoh S, Inoue H, Omura S et al (2013) Comparison of the reperfusion efficacy of thrombus aspiration with and without distal protection during primary percutaneous coronary intervention in patients with acute ST-segment elevation myocardial infarction. Am J Cardiol 112:1725–1729
de Lemos JA, Antman EM, Gibson CM et al (2000) Abciximab improves both epicardial flow and myocardial reperfusion in ST-elevation myocardial infarction. Observations from the TIMI 14 trial. Circulation 101:239–243
Claeys MJ, Bosmans J, De Ceuninck M et al (2004) Effect of intracoronary adenosine infusion during coronary intervention on myocardial reperfusion injury in patients with acute myocardial infarction. Am J Cardiol 94:9–13
Ishibashi F, Saito T, Hokimoto S, Noda K, Moriyama Y, Oshima S (2001) Combined revascularization strategy for acute myocardial infarction in patients with intracoronary thrombus: preceding intracoronary thrombolysis and subsequent mechanical angioplasty. Jpn Circ J 65:251–256
Purcell IF, Newall N, Farrer M (1997) Change in ST segment elevation 60 minutes after thrombolytic initiation predicts clinical outcome as accurately as later electrocardiographic changes. Heart 78:465–471
Anderson RD, White HD, Ohman EM et al (2002) Predicting outcome after thrombolysis in acute myocardial infarction according to ST-segment resolution at 90 min: a substudy of the GUSTO-III trial. Global use of strategies to open occluded coronary arteries. Am Heart J 144:81–88
Acknowledgments
We would like to thank all the staff and participants for their contributions to this study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
B. Peng, H. Xia, A. Ni, G. Wu, and X. Jiang state that there are no conflicts of interest.
Additional information
B. Peng and H. Xia contributed equally to this work.
Rights and permissions
About this article
Cite this article
Peng, B., Xia, H., Ni, A. et al. Serum NT-proBNP on admission can predict ST-segment resolution in patients with acute myocardial infarction after primary percutaneous coronary intervention. Herz 40, 898–905 (2015). https://doi.org/10.1007/s00059-015-4309-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-015-4309-0
Keywords
- Acute myocardial infarction
- Myocardial reperfusion
- ST-segment resolution
- Primary percutaneous coronary intervention
- N-terminal pro-brain natriuretic peptide