Abstract
Objectives
The purpose of this work was to evaluate the influence of insertion depth on the stability of orthodontic mini-implants. Sensitivity of three different methods to measure implant stability based on differences in insertion depth were determined.
Methods
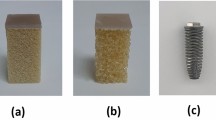
A total of 82 mini-implants (2 × 9 mm) were inserted into pelvic bone of Swabian Hall pigs. Each implant was inserted stepwise to depths of 4, 5, 6, 7, and 8 mm. At each of these depths, three different methods were used to measure implant stability, including maximum insertion torque (MIT), resonance frequency analysis (RFA), and Periotest®. Differences between the recorded values were statistically analyzed and the methods tested for correlations.
Results
Almost linear changes from each insertion depth were measured with the values of RFA [implant stability quotient (ISQ) values range from 1–100], which increased from 6.95 ± 2.85 ISQ at 4 mm to 34.63 ± 5.51 ISQ at 8 mm, and with those of Periotest® [periotest values (PTV) range from −8 to 50], which decreased from 13.24 ± 4.03 PTV to −2.89 ± 1.87 PTV. Both methods were found to record highly significant (p < 0.0001) changes for each additional millimeter of insertion depth. The MIT increased significantly (p < 0.0001) from 153.67 ± 69.32 Nmm to 261 ± 103.73 Nmm between 4 and 5 mm of insertion depth but no further significant changes were observed as the implants were driven deeper. The RFA and Periotest® values were highly correlated (r = −0.907).
Conclusions
Mini-implant stability varies significantly with insertion depth. The RFA and the Periotest® yielded a linear relationship between stability and insertion depth. MIT does not appear to be an adequate method to determine implant stability based on insertion depth.
Zusammenfassung
Zielsetzung
Ziel der Arbeit war es, den Einfluss der Insertionstiefe auf die Stabilität orthodontischer Mini-Implantate zu untersuchen und die Sensitivität verschiedener Stabilitätsmessmethoden in Hinblick auf den Parameter Insertionstiefe zu ermitteln.
Methoden
Insgesamt 82 Mini-Implantate (2 × 9 mm) wurden in den Beckenknochen vom Landschwein inseriert. Bei Insertionstiefen (ID) von 4, 5, 6, 7 und 8 mm wurden jeweils das maximale Eindrehmoment (MIT) gemessen sowie der Periotest® und die Resonanzfrequenzanalyse (RFA) durchgeführt. Die Ergebnisse für die verschiedenen ID wurden statistisch auf signifikante Unterschiede untersucht und die Messmethoden hinsichtlich ihrer Korrelation zueinander überprüft.
Ergebnisse
Die Werte für RFA stiegen mit zunehmender ID nahezu linear an [6,95 ± 2,85 ISQ (“implant stability quotient”) bei ID 4 mm auf 34,63 ± 5,51 ISQ bei ID 8 mm) und fielen für den Periotest® fast linear ab [13,24 ± 4,03 PTV (“periotest values”) auf −2,89 ± 1,87 PTV]. Die Änderungen waren für RFA und Periotest® bei jedem Millimeterschritt der Insertion hoch signifikant (p < 0,0001). Die MIT-Werte stiegen von 4 auf 5 mm ID an (153,67 ± 69,32 auf 261 ± 103,73 Nmm, p < 0,0001) und änderten sich von da an nicht mehr signifikant. RFA und Periotest® zeigten eine hohe Korrelation (r = −0,907).
Schlussfolgerung
Die ID hat einen signifikanten Einfluss auf die Stabilität der Mini-Implantate; der Zusammenhang scheint linearer Natur zu sein. Im Gegensatz zum MIT sind die RFA und der Periotest® dazu geeignet, die Stabilität in Bezug auf den Parameter der Insertionstiefe zu ermitteln.



Similar content being viewed by others
References
Brägger U, Hugel-Pisoni C, Burgin W et al (1996) Correlations between radiographic, clinical and mobility parameters after loading of oral implants with fixed partial dentures. A 2-year longitudinal study. Clin Oral Implants Res 7(3):230–239
Buchter A, Kleinheinz J, Wiesmann HP et al (2004) Peri-implant bone formation around cylindrical and conical implant systems. Mund Kiefer Gesichtschir 8(5):282–288
Buchter A, Kleinheinz J, Wiesmann HP et al (2005) Interface reaction at dental implants inserted in condensed bone. Clin Oral Implants Res 16(5):509–517
Buchter A, Kleinheinz J, Wiesmann HP et al (2005) Biological and biomechanical evaluation of bone remodelling and implant stability after using an osteotome technique. Clin Oral Implants Res 16(1):1–8
Buchter A, Wiechmann D, Koerdt S et al (2005) Load-related implant reaction of mini-implants used for orthodontic anchorage. Clin Oral Implants Res 16(4):473–479
Buchter A, Wiechmann D, Gaertner C et al (2006) Load-related bone modelling at the interface of orthodontic micro-implants. Clin Oral Implants Res 17(6):714–722
Chatzigianni A, Keilig L, Reimann S et al (2011) Effect of mini-implant length and diameter on primary stability under loading with two force levels. Eur J Orthod 33(4):381–387
Grandi T, Guazzi P, Samarani R et al (2013) Clinical outcome and bone healing of implants placed with high insertion torque: 12-month results from a multicenter controlled cohort study. Int J Oral Maxillofac Surg 42(4):516–520
Javed F, Almas K, Crespi R et al (2011) Implant surface morphology and primary stability: is there a connection? Implant Dent 20(1):40–46
Lachmann S, Jager B, Axmann D et al (2006) Resonance frequency analysis and damping capacity assessment. Part I: an in vitro study on measurement reliability and a method of comparison in the determination of primary dental implant stability. Clin Oral Implants Res 17(1):75–79
Lachmann S, Laval JY, Jager B et al (2006) Resonance frequency analysis and damping capacity assessment. Part 2: peri-implant bone loss follow-up. An in vitro study with the Periotest and Osstell instruments. Clin Oral Implants Res 17(1):80–84
Lukas D, Schulte W (1990) Periotest–a dynamic procedure for the diagnosis of the human periodontium. Clin Phys Physiol Meas 11(1):65–75
Meredith N, Alleyne D, Cawley P (1996) Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res 7(3):261–267
Nienkemper M, Wilmes B, Panayotidis A et al (2012) Measurement of mini-implant stability using resonance frequency analysis. Angle Orthod 83(2):230–238
Nienkemper M, Pauls A, Ludwig B et al (2013) Stability of paramedian inserted palatal mini-implants at the initial healing period: a controlled clinical study. Clin Oral Implants Res. 26(8):870–875
Nienkemper M, Wilmes B, Pauls A et al (2013) Mini-implant stability at the initial healing period. Angle Orthod. Epub ahead of print
Nienkemper M, Wilmes B, Pauls A et al (2013) Impact of mini-implant length on stability at the initial healing period: a controlled clinical study. Head Face Med 20(9):30
Noguerol B, Munoz R, Mesa F et al (2006) Early implant failure. Prognostic capacity of Periotest: retrospective study of a large sample. Clin Oral Implants Res 17(4):459–464
Pan CY, Chou ST, Tseng YC et al (2012) Influence of different implant materials on the primary stability of orthodontic mini-implants. Kaohsiung J Med Sci 28(12):673–678
Pithon MM, Figueiredo DS, Oliveira DD (2013) Mechanical evaluation of orthodontic mini-implants of different lengths. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 71(3):479–486
Schwarz F, Sager M, Kadelka I et al (2010) Influence of titanium implant surface characteristics on bone regeneration in dehiscence-type defects: an experimental study in dogs. J Clin Periodontol 37(5):466–473
Schwarz F, Sahm N, Iglhaut G et al (2011) Impact of the method of surface debridement and decontamination on the clinical outcome following combined surgical therapy of peri-implantitis: a randomized controlled clinical study. J Clin Periodontol 38(3):276–284
Su YY (2009) Primary stability of orthodontic mini-implants: analysis of biomechanical properties and clinical relevance. Doctoral thesis, Department of Orthodotnics Heinrich-Heine-Universität, Düsseldorf
Wilmes B, Rademacher C, Olthoff G et al (2006) Parameters affecting primary stability of orthodontic mini-implants. J Orofac Orthop 67(3):162–174
Wilmes B, Su YY, Drescher D (2008) Insertion angle impact on primary stability of orthodontic mini-implants. Angle Orthod 78(6):1065–1070
Wilmes B, Drescher D (2009) Impact of insertion depth and predrilling diameter on primary stability of orthodontic mini-implants. Angle Orthod 79(4):609–614
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Nienkemper, N. Santel, R. Hönscheid, and D. Drescher state that there are no conflicts of interest.
The accompanying manuscript does not include studies on humans or living animals.
Additional information
PD Dr. Manuel Nienkemper.
Rights and permissions
About this article
Cite this article
Nienkemper, M., Santel, N., Hönscheid, R. et al. Orthodontic mini-implant stability at different insertion depths. J Orofac Orthop 77, 296–303 (2016). https://doi.org/10.1007/s00056-016-0036-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-016-0036-2