Abstract
Background: Olanzapine is prescribed for a number of psychiatric disorders, including schizophrenia, bipolar mania, and unipolar and bipolar depression. Olanzapine treatment is associated with tolerability issues such as metabolic adverse effects (e.g. weight gain, increase in blood glucose, triglycerides and total cholesterol levels), extrapyramidal symptoms [EPS] (e.g. parkinsonism, akathisia, tardive dyskinesia) and sedative adverse effects. Metabolic issues lead to some long-term consequences, which include cardiovascular diseases (CVD) and type 2 diabetes mellitus, and these complications cause high rates of mortality and morbidity among patients with severe mental illnesses. The expanded indications of olanzapine in psychiatry suggest a need to investigate whether there is a difference in the incidence and severity of adverse effects related to category diagnosis. Are the adverse effects expressed differently according to phenotype? Unfortunately, there are no reported studies that investigated these differences in adverse effects associated with olanzapine treatment in psychiatric patients with different phenotypes.
Objective: The aim of the present meta-analysis is to separately examine olanzapine-induced cardiometabolic adverse effects and EPS in patients with schizophrenia and affective disorders.
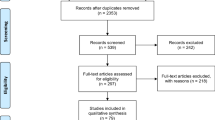
Data Sources: A search of computerized literature databases PsycINFO (1967–2010), PubMed (MEDLINE), EMBASE (1980–2010) and the clinicaltrials.gov website for randomized clinical trials was conducted. A manual search of reference lists of published review articles was carried out to gather further data.
Study Selection: Randomized controlled trials were included in our study if (i) they assessed olanzapine adverse effects (metabolic or extrapyramidal) in adult patients with schizophrenia or affective disorders; and (ii) they administered oral olanzapine as monotherapy during study.
Data Extraction: Two reviewers independently screened abstracts for choosing articles and one reviewer extracted relevant data on the basis of predetermined exclusion and inclusion criteria. It should be mentioned that for the affective disorders group we could only find articles related to bipolar disorder.
Data Synthesis: Thirty-three studies (4831 patients) that address olanzapine monotherapy treatment of adults with schizophrenia or bipolar disorder were included in the analysis. The primary outcomes were metabolic adverse effects (changes in weight, blood glucose, low-density lipoprotein, total cholesterol and triglyceride levels). The secondary outcomes of our study were assessing the incidence of some EPS (parkinsonism, akathisia and use of antiparkinson medication). The tolerability outcomes were calculated separately for the schizophrenia and bipolar disorder groups and were combined in a meta-analysis. Tolerability outcomes show that olanzapine contributes to weight gain and elevates blood triglycerides, glucose and total cholesterol levels in both schizophrenia and bipolar disorder patients. However, olanzapine treatment produced significantly more weight gain in schizophrenia patients than in bipolar disorder patients. In addition, increases in blood glucose, total cholesterol and triglyceride levels were higher in the schizophrenia group compared with the bipolar disorder group, even though these differences were not statistically significant. Based on our results, the incidence of parkinsonism was significantly higher in the schizophrenia group than in the bipolar disorder group. Subgroup analysis and logistic regression were used to assess the influence of treatment duration, dose, industry sponsorship, age and sex ratio on tolerability outcome.
Conclusions: Our results suggest that schizophrenia patients may be more vulnerable to olanzapine-induced weight gain. The findings may be explained by considering the fact that in addition to genetic disposition for metabolic syndrome in schizophrenia patients, they have an especially high incidence of lifestyle risk factors for CVD, such as poor diet, lack of exercise, stress and smoking. It might be that an antipsychotic induces severity of adverse effect according to the phenotype.









Similar content being viewed by others
Notes
‘N’ refers to the number of articles whereas ‘n’ is the number of patients.
References
Zhornitsky S, Potvin S, Moteshafi H, et al. Dose-response and comparative efficacy and tolerability of quetiapine across psychiatric disorders: a systematic review of the placebo-controlled monotherapy and add-on trials. Int Clin Psychopharmacol 2011 Jul; 26(4): 183–92
Tohen M, Sanger TM, McElroy SL, et al. Olanzapine versus placebo in the treatment of acute mania. Olanzapine HGEH Study Group. Am J Psychiatry 1999 May; 156(5): 702–9
Tohen M, Jacobs TG, Feldman PD. Onset of action of antipsychotics in the treatment of mania. Bipolar Disord 2000 Sep; 2 (3 Pt 2): 261–8
Keck Jr PE. Bipolar depression: a new role for atypical antipsychotics? Bipolar Disord 2005; 7 Suppl. 4: 34–40
Bhana N, Perry CM. Olanzapine: a review of its use in the treatment of bipolar I disorder. CNS Drugs 2001; 15(11): 871–904
Frampton JE. Olanzapine long-acting injection: a review of its use in the treatment of schizophrenia. Drugs 2010 Dec 3; 70(17): 2289–313
Parsons B, Allison DB, Loebel A, et al. Weight effects associated with antipsychotics: a comprehensive database analysis. Schizophr Res 2009 May; 110(1–3): 103–10
L’Italien GJ, Casey DE, Kan HJ, et al. Comparison of metabolic syndrome incidence among schizophrenia patients treated with aripiprazole versus olanzapine or placebo. J Clin Psychiatry 2007 Oct; 68(10): 1510–6
Pramyothin P, Khaodhiar L. Metabolic syndrome with the atypical antipsychotics. Curr Opin Endocrinol Diabetes Obes 2010 Oct; 17(5): 460–6
Fagiolini A, Frank E, Scott JA, et al. Metabolic syndrome in bipolar disorder: findings from the Bipolar Disorder Center for Pennsylvanians. Bipolar Disord 2005 Oct; 7(5): 424–30
Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res 2010 Nov; 123(2–3): 225–33
Fleischhacker WW, Cetkovich-Bakmas M, De Hert M, et al. Comorbid somatic illnesses in patients with severe mental disorders: clinical, policy, and research challenges. J Clin Psychiatry 2008 Apr; 69(4): 514–9
van Winkel R, De Hert M, Wampers M, et al. Major changes in glucose metabolism, including new-onset diabetes, within 3 months after initiation of or switch to atypical antipsychotic medication in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 2008 Mar; 69(3): 472–9
Laursen TM, Munk-Olsen T, Agerbo E, et al. Somatic hospital contacts, invasive cardiac procedures, and mortality from heart disease in patients with severe mental disorder. Arch Gen Psychiatry 2009 Jul; 66(7): 713–20
Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis 2006 Apr; 3 (2): A42
Cavazzoni PA, Berg PH, Kryzhanovskaya LA, et al. Comparison of treatment-emergent extrapyramidal symptoms in patients with bipolar mania or schizophrenia during olanzapine clinical trials. J Clin Psychiatry 2006 Jan; 67(1): 107–13
Leucht S, Corves C, Arbter D, et al. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 2009 Jan 3; 373(9657): 31–41
Miller CH, Mohr F, Umbricht D, et al. The prevalence of acute extrapyramidal signs and symptoms in patients treated with clozapine, risperidone, and conventional antipsychotics. J Clin Psychiatry 1998 Feb; 59(2): 69–75
Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry 2009 May; 70(5): 627–43
Kane JM. Tardive dyskinesia rates with atypical antipsychotics in adults: prevalence and incidence. J Clin Psychiatry 2004; 65 Suppl. 9: 16–20
Rummel-Kluge C, Komossa K, Schwarz S, et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr Bull 2010 May 31; 38(1): 167–77
Muscettola G, Barbato G, Pampallona S, et al. Extrapyramidal syndromes in neuroleptic-treated patients: prevalence, risk factors, and association with tardive dyskinesia. J Clin Psychopharmacol 1999 Jun; 19(3): 203–8
Tenback DE, van Harten PN, Slooff CJ, et al. Evidence that early extrapyramidal symptoms predict later tardive dyskinesia: a prospective analysis of 10,000 patients in the European Schizophrenia Outpatient Health Outcomes (SOHO) study. Am J Psychiatry 2006 Aug; 163(8): 1438–40
Nasrallah HA, Churchill CM, Hamdan-Allan GA. Higher frequency of neuroleptic-induced dystonia in mania than in schizophrenia. Am J Psychiatry 1988 Nov; 145(11): 1455–6
Stahl SM, Mignon L, Meyer JM. Which comes first: atypical antipsychotic treatment or cardiometabolic risk? Acta Psychiatr Scand 2009; 119(3): 171–9
van Winkel R, van Os J, Celic I, et al. Psychiatric diagnosis as an independent risk factor for metabolic disturbances: results from a comprehensive, naturalistic screening program. J Clin Psychiatry 2008 Aug; 69(8): 1319–27
Ryan MC, Collins P, Thakore JH. Impaired fasting glucose tolerance in first-episode, drug-naive patients with schizophrenia. Am J Psychiatry 2003 Feb; 160(2): 284–9
Spelman LM, Walsh PI, Sharifi N, et al. Impaired glucose tolerance in first-episode drug-naive patients with schizophrenia. Diabet Med 2007 May; 24(5): 481–5
Venkatasubramanian G, Chittiprol S, Neelakantachar N, et al. Insulin and insulin-like growth factor-1 abnormalities in antipsychotic-naive schizophrenia. Am J Psychiatry 2007 Oct; 164(10): 1557–60
Zhang ZJ, Yao ZJ, Liu W, et al. Effects of antipsychotics on fat deposition and changes in leptin and insulin levels: magnetic resonance imaging study of previously untreated people with schizophrenia. Br J Psychiatry 2004 Jan; 184: 58–62
Arranz B, Rosel P, Ramirez N, et al. Insulin resistance and increased leptin concentrations in noncompliant schizophrenia patients but not in antipsychotic-naive first-episode schizophrenia patients. J Clin Psychiatry 2004 Oct; 65(10): 1335–42
Huang J, Perlis RH, Lee PH, et al. Cross-disorder genome-wide analysis of schizophrenia, bipolar disorder, and depression. Am J Psychiatry 2010 Oct; 167(10): 1254–63
Peerbooms OL, van Os J, Drukker M, et al. Meta-analysis of MTHFR gene variants in schizophrenia, bipolar disorder and unipolar depressive disorder: evidence for a common genetic vulnerability? Brain Behav Immun 2011; 25(8): 1530–43
Purcell SM, Wray NR, Stone JL, et al. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 2009 Aug 6; 460(7256): 748–52
Borenstein M, Rothstein H. Comprehensive meta-analysis: a computer program for research synthesis. Englewood (NJ): Biostat, 1999
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986 Sep; 7(3): 177–88
Alvarez E, Ciudad A, Olivares JM, et al. A randomized, 1-year follow-up study of olanzapine and risperidone in the treatment of negative symptoms in outpatients with schizophrenia. J Clin Psychopharmacol 2006 Jun; 26(3): 238–49
Beasley Jr CM, Sanger T, Satterlee W, et al. Olanzapine versus placebo: results of a double-blind, fixed-dose olanzapine trial. Psychopharmacology (Berl) 1996 Mar; 124(1–2): 159–67
Bhowmick S, Hazra A, Ghosh M. Amisulpride versus olanzapine in the treatment of schizophrenia in Indian patients: randomized controlled trial. Aust N Z J Psychiatry 2010 Mar; 44(3): 237–42
Bitter I, Dossenbach MR, Brook S, et al. Olanzapine versus clozapine in treatment-resistant or treatment-intolerant schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 2004 Jan; 28(1): 173–80
Breier A, Berg PH, Thakore JH, et al. Olanzapine versus ziprasidone: results of a 28-week double-blind study in patients with schizophrenia. Am J Psychiatry 2005 Oct; 162(10): 1879–87
Chan HY, Chang CJ, Chiang SC, et al. A randomised controlled study of risperidone and olanzapine for schizophrenic patients with neuroleptic-induced acute dystonia or parkinsonism. J Psychopharmacol 2010 Jan; 24(1): 91–8
Dollfus S, Olivier V, Chabot B, et al. Olanzapine versus risperidone in the treatment of post-psychotic depression in schizophrenic patients. Schizophr Res 2005 Oct 15; 78(2–3): 157–9
Kane JM, Osuntokun O, Kryzhanovskaya LA, et al. A 28-week, randomized, double-blind study of olanzapine versus aripiprazole in the treatment of schizophrenia. J Clin Psychiatry 2009 Apr; 70(4): 572–81
Lecrubier Y, Quintin P, Bouhassira M, et al. The treatment of negative symptoms and deficit states of chronic schizophrenia: olanzapine compared to amisulpride and placebo in a 6-month double-blind controlled clinical trial. Acta Psychiatr Scand 2006 Nov; 114(5): 319–27
Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005 Sep 22; 353(12): 1209–23
McIntyre RS, Cohen M, Zhao J, et al. A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord 2009 Nov; 11(7): 673–86
McIntyre RS, Cohen M, Zhao J, et al. Asenapine versus olanzapine in acute mania: a double-blind extension study. Bipolar Disord 2009 Dec; 11(8): 815–26
McIntyre RS, Cohen M, Zhao J, et al. Asenapine in the treatment of acute mania in bipolar I disorder: a randomized, double-blind, placebo-controlled trial. J Affect Disord 2010 Apr; 122(1–2): 27–38
McIntyre RS, Cohen M, Zhao J, et al. Asenapine for long-term treatment of bipolar disorder: a double-blind 40-week extension study. J Affect Disord 2010 Nov; 126(3): 358–65
McQuade RD, Stock E, Marcus R, et al. A comparison of weight change during treatment with olanzapine or aripiprazole: results from a randomized, double-blind study. J Clin Psychiatry 2004; 65 Suppl. 18: 47–56
Riedel M, Muller N, Spellmann I, et al. Efficacy of olanzapine versus quetiapine on cognitive dysfunctions in patients with an acute episode of schizophrenia. Eur Arch Psychiatry Clin Neurosci 2007 Oct; 257(7): 402–12
Saddichha S, Manjunatha N, Ameen S, et al. Effect of olanzapine, risperidone, and haloperidol treatment on weight and body mass index in first-episode schizophrenia patients in India: a randomized, double-blind, controlled, prospective study. J Clin Psychiatry 2007 Nov; 68(11): 1793–8
Sanger TM, Tohen M, Vieta E, et al. Olanzapine in the acute treatment of bipolar I disorder with a history of rapid cycling. J Affect Disord 2003 Jan; 73(1–2): 155–61
Sirota P, Pannet I, Koren A, et al. Quetiapine versus olanzapine for the treatment of negative symptoms in patients with schizophrenia. Hum Psychopharmacol 2006 Jun; 21(4): 227–34
Tohen M, Calabrese JR, Sachs GS, et al. Randomized, placebo-controlled trial of olanzapine as maintenance therapy in patients with bipolar I disorder responding to acute treatment with olanzapine. Am J Psychiatry 2006 Feb; 163(2): 247–56
Tohen M, Goldberg JF, Gonzalez-Pinto Arrillaga AM, et al. A 12-week, double-blind comparison of olanzapine vs haloperidol in the treatment of acute mania. Arch Gen Psychiatry 2003 Dec; 60(12): 1218–26
Tohen M, Jacobs TG, Grundy SL, et al. Efficacy of olanzapine in acute bipolar mania: a double-blind, placebo-controlled study. The Olanzipine HGGW Study Group. Arch Gen Psychiatry 2000 Sep; 57(9): 841–9
Tohen M, Sutton VK, Calabrese JR, et al. Maintenance of response following stabilization of mixed index episodes with olanzapine monotherapy in a randomized, double-blind, placebo-controlled study of bipolar 1 disorder. J Affect Disord 2009 Jul; 116(1–2): 43–50
Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003 Nov; 60(11): 1079–88
Tohen M, Vieta E, Goodwin GM, et al. Olanzapine versus divalproex versus placebo in the treatment of mild to moderate mania: a randomized, 12-week, double-blind study. J Clin Psychiatry 2008 Nov; 69(11): 1776–89
Vanelle JM, Douki S. A double-blind randomised comparative trial of amisulpride versus olanzapine for 2 months in the treatment of subjects with schizophrenia and comorbid depression. Eur Psychiatry 2006 Dec; 21(8): 523–30
Wu RR, Zhao JP, Liu ZN, et al. Effects of typical and atypical antipsychotics on glucose-insulin homeostasis and lipid metabolism in first-episode schizophrenia. Psychopharmacology (Berl) 2006 Jul; 186(4): 572–8
Janssen-Cilag International NV. Prospective randomized open-label 6-month head-to-head trial to compare metabolic effects of paliperidone ER and olanzapine in subjects with schizophrenia [ClinicalTrials.gov identifier NCT00645099]. US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov [Accessed 2011 May 18]
Eli Lilly and Company. A randomized, open-label study comparing the effects of olanzapine pamoate depot with oral olanzapine on treatment outcomes in outpatients with schizophrenia [ClinicalTrials.gov identifier NCT00320489]. US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov [Accessed 2010 Oct 25]
Eli Lilly and Company. Efficacy and safety of olanzapine in the treatment of patients with bipolar I disorder, depressed: a randomized, double-blind comparison with placebo [ClinicalTrials.gov identifier NCT00510146]. US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov [Accessed 2011 Apr 26]
Schering-Plough. A multicenter, double-blind, flexible-dose, 6-month trial comparing the efficacy and safety of asenapine with olanzapine in stable subjects with predominant, persistent negative symptoms of schizophrenia [Clinical-Trials.gov identifier NCT00145496]. US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov [Accessed 2010 Apr 8]
Eli Lilly and Company. Placebo- and haloperidol-controlled double-blind trial of olanzapine in patients with manic or mixed episode of bipolar I disorder [ClinicalTrials.gov identifier NCT00129220]. US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov [Accessed 2010 Dec 10]
Henderson DC, Cagliero E, Copeland PM, et al. Glucose metabolism in patients with schizophrenia treated with atypical antipsychotic agents: a frequently sampled intravenous glucose tolerance test and minimal model analysis. Arch Gen Psychiatry 2005 Jan; 62(1): 19–28
Newcomer JW, Haupt DW, Fucetola R, et al. Abnormalities in glucose regulation during antipsychotic treatment of schizophrenia. Arch Gen Psychiatry 2002 Apr; 59(4): 337–45
Bond DJ, Kauer-Sant’Anna M, Lam RW, et al. Weight gain, obesity, and metabolic indices following a first manic episode: prospective 12-month data from the Systematic Treatment Optimization Program for Early Mania (STOP-EM). J Affect Disord 2010 Jul; 124(1–2): 108–17
De Hert M, Dobbelaere M, Sheridan EM, et al. Metabolic and endocrine adverse effects of second-generation anti-psychotics in children and adolescents: a systematic review of randomized, placebo controlled trials and guidelines for clinical practice. Eur Psychiatry 2011 Apr; 26(3): 144–58
Peuskens J, De Hert M, Mortimer A. Metabolic control in patients with schizophrenia treated with amisulpride or olanzapine. Int Clin Psychopharmacol 2007 May; 22(3): 145–52
Allison DB, Mentore JL, Heo M, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 1999 Nov; 156(11): 1686–96
Czobor P, Volavka J, Sheitman B, et al. Antipsychotic-induced weight gain and therapeutic response: a differential association. J Clin Psychopharmacol 2002 Jun; 22(3): 244–51
Haddad P. Weight change with atypical antipsychotics in the treatment of schizophrenia. J Psychopharmacol 2005 Nov; 19 (6 Suppl.): 16–27
Reynolds GP, Yao Z, Zhang X, et al. Pharmacogenetics of treatment in first-episode schizophrenia: D3 and 5-HT2C receptor polymorphisms separately associate with positive and negative symptom response. Eur Neuropsychopharmacol 2005 Mar; 15(2): 143–51
Correll CU, Lencz T, Malhotra AK. Antipsychotic drugs and obesity. Trends Mol Med 2011; 17: 97–107
De Hert M, Detraux J, Van Winkel R, et al. Metabolic and cardiovascular adverse effects associated with anti-psychotic drugs. Nat Rev Endocrinol 2011 Oct; 8(2): 114–26
Nakamura M, Nagamine T. Severe hyperglycemia induced by olanzapine was improved with a recovery of insulin secretion after switching to risperidone and introducing insulin therapy. Intern Med 2010; 49(23): 2635–7
Nasrallah HA. Atypical antipsychotic-induced metabolic side effects: insights from receptor-binding profiles. Mol Psychiatry 2008 Jan; 13(1): 27–35
Bai YM, Chen TT, Liou YJ, et al. Association between HTR2C polymorphisms and metabolic syndrome in patients with schizophrenia treated with atypical antipsychotics. Schizophr Res 2011 Feb; 125(2–3): 179–86
Gunes A, Melkersson KI, Scordo MG, et al. Association between HTR2C and HTR2A polymorphisms and metabolic abnormalities in patients treated with olanzapine or clozapine. J Clin Psychopharmacol 2009 Feb; 29(1): 65–8
Melkersson KI, Gunes A, Dahl ML. Impact of serotonin receptor 2A gene haplotypes on C-peptide levels in clozapine- and olanzapine-treated patients. Hum Psychopharmacol 2010 Jun; 25(4): 347–52
Casey DE. Dyslipidemia and atypical antipsychotic drugs. J Clin Psychiatry 2004; 65 Suppl. 18: 27–35
Chaggar PS, Shaw SM, Williams SG. Effect of antipsychotic mmedications on glucose and lipid levels. J Clin Pharmacol 2011; 51(5): 631–8
Meyer JM. Novel antipsychotics and severe hyperlipidemia. J Clin Psychopharmacol 2001 Aug; 21(4): 369–74
Albaugh VL, Judson JG, She P, et al. Olanzapine promotes fat accumulation in male rats by decreasing physical activity, repartitioning energy and increasing adipose tissue lipogenesis while impairing lipolysis. Mol Psychiatry 2011 May; 16(5): 569–81
Wampers M, Hanssens L, van Winkel R, et al. Differential effects of olanzapine and risperidone on plasma adiponectin levels over time: results from a 3-month prospective open-label study. Eur Neuropsychopharmacol 2012; 22(1): 17–26
Carlson CD, Cavazzoni PA, Berg PH, et al. An integrated analysis of acute treatment-emergent extrapyramidal syndrome in patients with schizophrenia during olanzapine clinical trials: comparisons with placebo, haloperidol, risperidone, or clozapine. J Clin Psychiatry 2003 Aug; 64(8): 898–906
Gao K, Kemp DE, Ganocy SJ, et al. Antipsychotic-induced extrapyramidal side effects in bipolar disorder and schizophrenia: a systematic review. J Clin Psychopharmacol 2008 Apr; 28(2): 203–9
Taylor VH, McIntyre RS, Remington G, et al. Beyond pharmacotherapy: understanding the links between obesity and chronic mental illness. Can J Psychiatry 2012 Jan; 57(1): 5–12
Regenold WT, Thapar RK, Marano C, et al. Increased prevalence of type 2 diabetes mellitus among psychiatric inpatients with bipolar I affective and schizoaffective disorders independent of psychotropic drug use. J Affect Disord 2002; 70: 19–26
Cacabelos R, Hashimoto R, Takeda M. Pharmacogenomics of antipsychotics efficacy for schizophrenia. Psychiatry Clin Neurosci 2011; 65: 3–19
Liou YJ, Bai YM, Lin E, et al. Gene-gene interactions of the INSIG1 and INSIG2 in metabolic syndrome in schizophrenic patients treated with atypical antipsychotics. Pharmacogenomics J 2012 Feb; 12(1): 54–61
Acknowledgements
Emmanuel Stip is holder of the Eli Lilly Chair on Schizophrenia from the University of Montreal. This study was supported in part by an operating grant, IIT (Investigator-Initiated Trial), from Pfizer, AstraZeneca, and Eli Lilly Canada; however, no funding was received for this specific meta-analysis. All other authors have no conflicts of interest to declare that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moteshafi, H., Zhornitsky, S., Brunelle, S. et al. Comparing Tolerability of Olanzapine in Schizophrenia and Affective Disorders. Drug Saf 35, 819–836 (2012). https://doi.org/10.1007/BF03261978
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03261978