Abstract
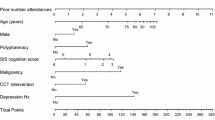
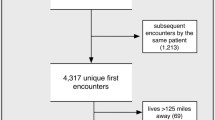
Emergency readmissions among patients discharged from the medical service of an acute-care teaching hospital were analyzed. Using the multivariate technique of recursive partitioning, the authors developed and validated a model to predict readmission based on diagnoses and other clinical factors. Of the 4,769 patients in the validation series, 19% were readmitted within 90 days. Twenty-six per cent of the readmissions occurred within ten days of discharge, and 57% within 30 days. Readmitted patients were older, had longer hospitalizations, and had greater hospital charges (p<0.01). The discharge diagnoses of AIDS, renal disease, and cancer were associated with increased risks of read-mission regardless of patients’ demographics or test results. The relative risks (95% confidence interval) associated with these diagnoses were: AIDS, 3.3 (1.4–7.8); renal disease, 2.3 (1.7–3.0); cancer, 2.8 (2.4–3.4). Other patients at increased risk were those with diabetes, anemia, and elevated creatinine (2.1; 1.6–2.8) and those with heart failure and elevated anion gaps (2.2; 1.7–2.8). For patients without one of these diagnoses, a normal albumin and no prior admission within 60 days identified patients at reduced risk for readmission (0.4; 0.3–0.4). Thus, commonly available clinical data identify patients at increased risk for emergency readmission. Risk factor profiles should alert physicians to these patients, as intensive intervention may be appropriate. Future studies should test the impacts of clinical interventions designed to reduce emergency readmissions.
Similar content being viewed by others
References
Zook CJ, Savickis SF, Moore FD. Repeated hospitalization for the same disease: a multiplier of national health costs. Milbank Mem Fund Q 1980;58:454–71
Zook CJ, Moore FD. High cost users of medical care. N Engl J Med 1980;302:996–1002
Anderson GF, Steinberg EP. Hospital readmissions in the Medicare population. N Engl J Med 1984;311:1349–53
Smith DM, Norton JA, McDonald CJ. Nonelective readmissions of medical patients. J Chronic Dis 1985;38:213–24
Bleich HL, Beckley RF, Horowitz GL, et al. Clinical computing in a teaching hospital. N Engl J Med 1985;312:756–64
ICD9-CM Volume 1 diseases tabular list. Commission on Professional and Hospital Activities. Ann Arbor, MI: Edwards Brothers, 1980
Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and regression trees, Belmont, CA: Wadsworth International Group, 1984
Snedecor GW, Cochran WG. Statistical methods. Ames, IA: Iowa State University Press, 1980
Schroeder SA, Showstack JA, Roberts HE. Frequency and clinical description of high-cost patients in 17 acute-care hospitals. N Engl J Med 1979;300:1306–9
Ellenberg M, Rifkin H (eds.). Diabetes mellitus: theory and practice. 3rd ed. New Hyde Park, NY: Medical Examination Publishing Co., 1983
Allman RM, Laprade CA, Noel LB, et al. Pressure sores among hospitalized patients. Ann Intern Med 1986;105:337–42
Demlo LK, Campbell PM, Brown SS. Reliability of information abstracted from patients’ records. Med Care 1978;16:995–1005
Lloyd SS, Rissing JP. Physician and coding errors in patient records. JAMA 1985;254:1330–6
Still S. The reliability of medical records. J Am Med Rec Assoc 1980;51:20–7
Corn RF. Quality control of hospital discharge data. Med Care 1980;18:416–26
Stern RS, Epstein AM. Institutional responses to prospective payment based on diagnosis-related groups. Implications for cost, quality, and access. N Engl J Med 1984;312:621–7
Cook EF, Goldman L. Empiric analysis of multivariate analytic techniques: advantages and disadvantages of recursive partitioning analysis. J Chronic Dis 1984;37:721–31
Author information
Authors and Affiliations
Additional information
Received from the Division of General Medicine and Primary Care, Department of Medicine, Harvard Medical School. Beth Israel Hospital; the Charles A.Dana Research Institute and Harvard Thorndike Laboratory of Beth Israel Hospital; and the Center for Clinical Computing, Department of Medicine, Harvard Medical School. Beth Israel and Brigham and Women’s Hospitals, Boston, Massachusetts.
Presented in part at the meeting of the American Federation for Clinical Research, Washington, DC, May 1986.
Supported in part by grants HS04928 from the National Center for Health Services Research and LM 04260 from the National Library of Medicine.
Rights and permissions
About this article
Cite this article
Phillips, R.S., Safran, C., Cleary, P.D. et al. Predicting emergency readmissions for patients discharged from the medical service of a teaching hospital. J Gen Intern Med 2, 400–405 (1987). https://doi.org/10.1007/BF02596366
Issue Date:
DOI: https://doi.org/10.1007/BF02596366