Abstract
Background
The universal vaccination of children for influenza has recently been recommended in the UK and is being considered in other developed countries.
Objectives
The aim of this study was to explore the potential costs and benefits of childhood influenza vaccination to gain a better understanding of the key drivers of cost-effectiveness.
Methods
As our case study we examined the cost-effectiveness of vaccination in Australian schoolchildren using an age-stratified Susceptible Exposed Infectious Recovered model.
Results
The results of this study highlight the critical role that methodological choices play in determining the cost-effectiveness of influenza vaccination. These choices include decisions about the structure of the model (including/excluding herd immunity) and what costs and benefits to include in the analysis. In scenarios where herd protection was included we estimated that the program was likely to be cost-effective. The study also illustrates the importance of the inherent seasonal variability of influenza, which can produce counter-intuitive results, with low transmission seasons being easier to control by vaccination but resulting in fewer benefits.
Conclusions
Universal childhood influenza vaccination is likely to be cost-effective if a substantial herd protection effect can be achieved by the program. However, it is important that decision makers understand the role of seasonal variability and the impact of alternative methodological choices in economic evaluations of influenza vaccination.
Similar content being viewed by others
• If universal childhood influenza vaccination results in a substantial herd protection effect then the program is likely to be cost-effective.
• Methodological choices in model structure and the cost and benefits included in evaluations are influential and not always definitively specified in guidelines.
• Year to year variation in influenza transmission is an important factor that needs to be understood alongside other forms of uncertainty.
1 Introduction
The universal vaccination of children for influenza has recently been recommended in the UK and is being considered in other developed countries [1, 2]. The vaccination of schoolchildren against influenza has the capacity to reduce the high burden of infection in this age group [3]. It also offers the potential to reduce influenza transmission in the community through herd protection [4]. These herd effects have become of increasing interest as doubts persist about the magnitude of the direct impact of vaccination in the elderly [5–7], those most at risk of serious complications [8, 9]. Statistical estimates of disease attributable to influenza have consistently found that Australians aged over 65 years have the highest rates of severe disease [10, 11]; however, these estimates can vary by the methodological approach chosen [8].
The evidence of herd protection effects from the vaccination of children against influenza have largely come from ecological studies [12, 13], with recent clinical trial evidence in remote communities providing further evidence [14]. The use of dynamic transmission models offers a way to simulate the effects of vaccination efforts on the wider population by having the risk of infection vary on the basis of the proportion of the population infected [15–17]. These methods have been applied to assess control efforts for both epidemic [18, 19] and pandemic influenza [20–24] but have rarely been linked to economic models in this context, with non-dynamic models primarily used in past studies [4]. In non-dynamic (static) models the risk of infection is constant in time and benefits are (typically) restricted to those vaccinated, with infection in the wider population unaffected by increased childhood vaccination.
In a recent review we identified model structure choices (static or dynamic) and the scope of included costs and benefits as major drivers of between-study differences in the cost-effectiveness of childhood influenza vaccination [4]. The inclusion/exclusion of productivity costs was also found to be highly influential in these analyses [4]. The productivity losses which may be prevented by childhood influenza vaccination and included in a societal perspective [25] result from lost time caring for sick children and/or from secondary infections in adults (herd protection) [4]. How productivity costs are included and the weight that decision makers place on them varies [25], with some government guidelines specifically excluding them or restricting them to absenteeism from paid work. In Australia productivity costs cannot be included in the primary economic analysis, although the cost of lost work time can be presented in a supplementary analysis [26].
The aim of this study was to explore the potential costs and benefits of childhood influenza vaccination to gain a better understanding of the key drivers of cost-effectiveness. As our case study we examined the cost-effectiveness of seasonal vaccination in Australian schoolchildren using a simplified model. The main focus of the analysis was to examine the impact of methodological choices and structural uncertainty (related to including/excluding herd protection). This was combined with consideration of seasonal variations in the transmissibility of influenza to understand how this factor may also influence the cost-effectiveness of vaccination.
2 Methods
2.1 Model
We adapted a previously constructed age-stratified Susceptible Exposed Infectious Recovered (SEIR) model (described in [27]) to estimate the underlying transmission of influenza under alternative vaccination scenarios. The model was able to estimate the herd protection conferred to the population through vaccination. The population was stratified into 5-year age intervals [28] except for the 15 to 19-year age range which was split into 15 to 17-year and 18 to 19-year groups to allow targeting of school-age children. Age-specific infectious contact rates were assumed to be proportional to average “all-reported” contacts rates (adapted from [29]). The model was run over a time horizon of a single year.
The age-specific probabilities of health states occurring (given clinical infection) were equal to the ratio of the population rate for each health state to the age-specific clinical attack rate (CAR) generated by the transmission model under current practice vaccination (Electronic Supplementary Material (ESM) Table A1). Under sensitivity analysis, these ratios were held fixed, so that variation in the population occupying these health states was directly proportional to variation in the CAR. Costs (Australian dollars, A$) and health effects (Quality-Adjusted Life Years, QALYs) were attached to health states.
2.2 Vaccination Strategies
We evaluated a hypothetical government funded school-based influenza (trivalent inactivated vaccine, as currently approved in Australia) vaccination program targeted at all Australian children aged 5–17 years. We assumed a base-case vaccine program uptake of 60 % (varied in sensitivity analysis). This estimate was below that achieved for other school-based vaccination programs [30]. The comparator was that of current practice, where existing vaccination uptake was assumed (less than 6 months, 0 %—not recommended; 6 months to 17 years, 5 %; 18–64 years, 22.8 % [31]; 65 and over, 74.6 % [31]). Vaccination was assumed to occur prior to the epidemic in each simulation.
2.3 Vaccine Efficacy
We assumed an efficacy of 60 % against influenza infection for children and adults (5–64 years) [32]. In the elderly (65 years and older) and in young children (less than 5 years), who are less likely to respond to influenza vaccination [7], we assumed an efficacy of 30 and 40 %, respectively [33]. In our case study, vaccine uptake in these age groups remained constant and had limited impact on cost-effectiveness. We implemented vaccination in the model as a reduction in susceptibility to infection [34] (see [27] for an exploration of alternative methods).
2.4 Transmission
The transmissibility of influenza varies from year to year with the circulating strain. The effective reproductive number (R) for influenza in Australia has previously been estimated to vary year to year in the approximate range 1.1–1.5, with a mean value of 1.3 [35]. We defined R as the number of secondary cases that a representative case infects at the start of an epidemic in a population with the existing levels of vaccine uptake/natural immunity. We assumed asymptomatic individuals were half as infectious as symptomatic individuals [18, 21] and 27 % of the population were immune prior to an epidemic [36, 37].
2.5 Disease
The transmission model calculates an epidemic curve of infections and an overall attack rate for each age group (ESM Table 1A). We assumed that 35 % of individuals infected would develop clinical (fever) symptoms [38], which was broadly consistent with the outcomes study applied (e.g. QALY loss) [39]. The current population rates of general practitioner (GP) visits for influenza were estimated from a study of general practice activity [10]. Population rates of influenza-attributable hospitalisation and death were drawn from a time-series regression analysis of pneumonia and influenza (ICD J10–J18) cases [10, 11]. These rates represent the difference between the observed disease burden under this category (J10–18) and the estimated burden without influenza circulating. Statistical methods are frequently used to estimate influenza disease because of the lack of routine testing in clinical practice. In those aged less than 50 years, no Australian estimates of influenza-attributable deaths were available and laboratory-confirmed influenza deaths were applied [40, 41].
2.6 Costs
We examined two commonly applied perspectives for costs [25]: that of the healthcare payer, which included all healthcare costs irrespective of who incurred them [26]; and a societal perspective, which additionally included productivity losses. All costs are reported in 2010 A$ and adjusted by the Australian consumer price index (CPI) where appropriate.
The assumed cost of the influenza vaccine under a hypothetical government-funded school-based program was set at $9 in the base-case model (approximated from wholesaler cost [42]). The school-based administration costs ($11.60 per dose) were based on estimates for council-delivered vaccination in school-aged children [43]. The small amount of private vaccination in schoolchildren under current practice was assumed to be delivered via GPs ($15.70 [44] plus patient co-payment $5 [45]), with vaccine purchased privately ($12, approximated from [46]). The healthcare costs associated with influenza GP visits ($33.32 [10] plus patient co-payment $5 [45]) and hospitalisation were based on a previous analysis [10]. Detail on age-specific parameters values can be found in the ESM (Table A2).
2.7 Productivity Losses
Productivity losses were based on estimated absences from paid work (consistent with Australian guidelines for supplementary analysis [26]) and were calculated using the human capital approach [25]. For sick children aged less than 15 years, caregiver work loss was included in productivity losses. This was based on average full-time weekly earnings [47] and the time off (66 % female, 34 % male) paid work (0.7 days) caring for a child with clinical illness [48].
For those aged more than 15 years, the cost of absenteeism was based on age-specific average weekly earnings [47] adjusted for workforce participation rates [49]. Clinical cases were assumed to be absent from work for 2.6 days for those who sought GP healthcare [50] and 0.3 days those not seeking healthcare [51]. Average length of stay was used to estimate absenteeism for hospitalised cases [52].
2.8 Quality of Life
We applied a QALY loss for influenza illness of 0.008 [39]. QALY losses from influenza death were calculated by applying quality-of-life norms by age [53] to estimated life expectancy [54]. Future QALYs gained through averted mortality have been discounted to the present time (using a 5 % discount rate) [26]. As we project the impact of vaccination over a single year, costs and QALY loss from short-term illness were not discounted.
2.9 Calculation of the Incremental Cost-Effectiveness Ratio (ICER)
As there is variation in the reproduction number (R) from year to year, we calculated ICERs (Table 1) that could be viewed as the average over many seasons. This is preferable to using a single mid-range R value (e.g. 1.3) owing to the non-linear nature of dynamic model results by variation in transmission parameters [55]. To do this, we calculated the ICER as the ratio of the mean cost and the mean QALYs, computed as the (numerical) integral of ICERs generated with R weighted by the log-normal distribution (μ = 0.2429, σ = 0.2), chosen to match the mean and interquartile ranges of R estimates from Australia [35].
2.10 Sensitivity Analysis
The focus of the sensitivity analyses was on methodological choices as represented in scenario analyses rather than parameter uncertainty. This decision was driven by the aim of the study and our recent review, which identified these choices as drivers of cost-effectiveness [4].
We examined multiple scenarios (Table 1) including the perspective for costs (described above). The other primary scenarios were the inclusion/exclusion of herd immunity. In the ‘no herd’ scenario the vaccine effects were applied only against health outcomes in vaccinated individuals (ESM). We also examined alternative estimates of influenza mortality [11, 40, 41] and restricting QALY loss to mortality only, by excluding the short-term quality-of-life impact from clinical illness. While QALY losses may be used as an outcome measure for non-severe short-term illness, the weight given to the prevention of such illness by decision makers is not always clear [56, 57].
We examined the results in combination with the seasonal variability of influenza transmissibility. Cost-effectiveness analyses typically focus on generating results on ‘average’; however, it is also important to understand the variability in costs and benefits [27] from year to year [4, 55]. Because of our focus on methodological uncertainty, we did not perform probabilistic sensitivity analysis but we have sought to identify the differential impact of each parameter through univariate analysis (ESM, Fig. A1). Finally, we conducted a simplified ‘pessimistic parameter scenario’ (Table 1) where the 20 most influential parameters were set to the value least favourable to vaccination (±25 %, ESM Fig. A1).
3 Results
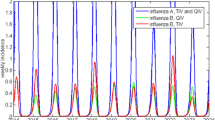
Figure 1 presents the number of influenza clinical cases, GP visits, hospitalisations and deaths as a function of the transmissibility of the epidemic (R). The number of cases for each of these outcomes increases with R. The number of cases prevented by school-based vaccination peaks and then declines moderately for highly transmissible epidemics. The absolute disease burden prevented by vaccination remains substantial even as R increases, as a result of a trade-off between the increasing overall risk of disease and the reduced herd protection.
The age distribution of the prevented cases varies by the outcome considered (Fig. 1). For influenza clinical cases and GP visits the majority of cases prevented occur in schoolchildren and adults, who have the largest overall disease burden for these outcomes. However, for more severe outcomes, a larger number of cases are prevented in the elderly through herd protection. For hospitalisations, the cases prevented by herd protection to children below the age targeted in this program and adults were also substantial.
Figure 2 presents the costs and QALYs saved by school-based vaccination. When herd protection was included, the majority of the potential cost savings resulted from productivity gains by way of reduced absenteeism in adults (and to a lesser extent reduced caregiver absenteeism, related to reduced infections in children). The cost savings from reduced hospitalisation were also substantial, largely as a result of the herd protection to adults and the elderly. The total saving from the program outweighed the cost of vaccination resulting in a net saving of A$56 million; however, when productivity gains were excluded (healthcare perspective) the program resulted in a net loss of A$19 million (Table 1). The ICER for the healthcare perspective was $3,500 per QALY saved. The potential QALY savings from the program came primarily from the prevention of short-term illness, with the prevention of death in the elderly also resulting in a substantial QALY saving (Fig. 2).
Estimated incremental costs (top) and QALYs (bottom) saved from school-based vaccination compared to current practice, with (left) and without (right) herd immunity. The shaded areas indicate the sources for the costs and QALYs saved. The estimated costs of the vaccination program are shown on the right
When herd protection was excluded, the benefits were restricted to the vaccinated schoolchildren. Again, the majority of the potential cost savings came from productivity gains (from reduced caregiver absenteeism); but this was substantially outweighed by the cost of vaccination, resulting in a net loss of A$33 million (societal perspective) or A$43 million (healthcare perspective). However, the ICER for the program remained at (or below) $50,000 per QALY saved for both perspectives, with a break-even cost of vaccination (vaccine and administration) of $9 and $3 per dose, respectively (Table 1). The majority of the QALY savings came from the prevention of short-term illness in schoolchildren, with this age group having relatively low risk of influenza mortality (Fig. 2).
When the QALY loss from short-term illness was excluded, the potential QALY savings remained substantial for scenarios that included herd protection, owing to the reduced mortality in the elderly. The costs were unchanged in these scenarios, with the societal perspective remaining cost saving and the ICER for the healthcare perspective approximately $15,800 per QALY saved (Table 1). However, when herd protection was excluded, the only remaining source for QALY savings was the reduced mortality in vaccinated schoolchildren, and the ICER increased to more than $3 million per QALY saved for both perspectives (Table 1).
We explored the use of two alternative influenza mortality estimates (as available for those older than 50 years), a higher estimate of influenza-attributable deaths from time-series regression analysis of a broader category (respiratory disease) [11] and restricting to laboratory-confirmed influenza deaths only [40, 41]. The use of these alternative estimates substantially changed the QALYs saved under herd protection scenarios but not the ICERs (results not shown in Table 1). This is because the denominator (QALYs) from the prevention of short-term illness was sufficient to maintain a low ICER. However, when QALY loss from short-term illness was excluded, the restriction to laboratory-confirmed influenza deaths only led to an ICER of greater than $100,000 per QALY saved from a healthcare perspective.
The parameter values that had the most influence on results were those related to vaccine efficacy, proportion of cases asymptomatic, vaccination cost, and the quality of life lost from clinical illness (ESM, Fig. A1). Vaccine uptake was important in the dynamic model but was not influential when herd protection was excluded as the costs and benefits of vaccination were then in proportion to doses supplied. Setting multiple parameters to the value least favourable to vaccination led to a significant change to results; however, the ICER remained less than $30,000 per QALY saved for both perspectives (Table 1, ‘Pessimistic parameter scenario’). Only when herd protection was also excluded did the ICER increase to greater than $150,000 per QALY saved.
Figure 3 presents the ICER as a function of R. In seasons with low transmission, the program is less cost-effective, as the overall risk of disease is low and the absolute number of disease cases prevented (and costs and QALYs saved) by a program is limited. The program is most cost-effectiveness in seasons with moderate transmission before declining in highly transmissible seasons. As with Fig. 1, this result is due to the decreasing herd protection as transmissibility increases, which outweighs the potential benefits from the greater preventable disease burden.
Estimated cost-effectiveness of school-based vaccination (healthcare perspective) by seasonal variation in the transmissibility (R) and pathogenicity (see “Methods”) of the epidemic. The results are shown for alternative assumption of vaccine uptake (40, 60 %) and vaccine efficacy (20, 60, 80 %)
Figure 3 also shows how the ICER may vary from year to year with the pathogenicity of the epidemic (i.e. the severity of cases) and the match of the vaccine. The low pathogenicity scenario represents a season where cases were half as likely to suffer complications from influenza (healthcare use or death), with these outcomes being twice as likely in a high pathogenicity season. Although variability in these factors was influential, the cost-effectiveness of the program was robust to these changes, with the ICER less than $50,000 per QALY saved for seasons with low pathogenicity and a relatively poor vaccine match.
4 Discussion
The results of this study highlight the importance of methodological choices in determining the potential costs and benefits of school-based influenza vaccination. These choices include decisions about the structure of the model (including/excluding herd protection) and the costs (societal/healthcare perspective) and health effects (QALY loss from short-term illness and mortality estimates) included in the analysis. These choices often had more influence on cost-effectiveness results than variation due to parameter uncertainty. For example, we found that a single methodological decision, such as the choice of model structure to include or exclude herd protection, could have more influence on results than simultaneously varying the 20 most influential parameter assumptions to the value least favourable to vaccination (Table 1).
Understanding the impact of these methodological decisions is important because a variety of choices (that we explore) have been made in the published literature and these choices help to explain the inconsistency in results between studies [4]. This is true even for analyses conducted for the same country, where government guidelines may not always offer definitive direction and/or where multiple choices may be acceptable [58]. For example, QALY loss for short-term illness has often not been included in economic evaluations of childhood influenza [4]. The reasons for this may vary from a lack of data and difficulties in measuring these outcomes [59], to a desire to avoid ‘double counting’ [60, 61] with productivity costs, or questions about the value decision makers and society place on the prevention of these outcomes [56, 57]. Likewise, statistical estimates of influenza mortality (and hospitalisation) are dependent on methodological choices with no consensus approach available [8, 27].
We found that school-based vaccination may have the potential to produce substantial herd protection effects. These population effects have largely been ignored in previous economic evaluations of childhood vaccination [4]. Failure to include these possible herd benefits could be seen as a ‘conservative’ approach; however, it leaves important structural model uncertainties unexplored [4] and decision makers without potentially important information. The potential for herd protection emphasises the importance of obtaining accurate estimates of influenza-attributable mortality in the elderly [8, 9]. Our analysis suggests that if universal childhood influenza vaccination results in a substantial herd protection effect then the program is likely to be cost-effective. Further empirical evidence of herd protection with childhood influenza vaccination would help to reduce uncertainty in future analyses. Achieving high uptake may present a major practical challenge, given the (partly) altruistic nature of the program and the potential lack of appeal for parents.
As our analysis focused on the impact of methodological choices and these choices were more influential than simultaneous variation of multiple parameters, we did not perform probabilistic sensitivity analysis. Our results illustrate, in the context of infectious disease control, why it is important to go beyond parameter variation to assess other forms of uncertainty in cost-effectiveness models. Probabilistic approaches to exploring parameter uncertainty in combination with other forms of uncertainty, such as alternative model choices and methodological decisions, are being developed [58]. A comprehensive approach to sensitivity analysis which incorporates all known sources of uncertainty will be important to fully understand the cost-effectiveness of influenza vaccination, as well as other vaccination programs. This includes other forms of model uncertainty that were beyond the scope of this analysis [27, 58].
This study also highlights the importance of understanding and appropriately including seasonal variability in economic evaluations of influenza vaccination. The inherent year-to-year variability in the costs and benefits that are likely to occur from vaccination is distinct from the uncertainty as to the correct ‘average’ parameter values (e.g. the estimated CAR for influenza over long periods) [27]. This seasonal variability means that in some years the vaccination program may appear to be a success, largely preventing influenza circulation, whereas in other years it may appear to be a failure. However, the results for cost-effectiveness may often be counter-intuitive, with low transmission seasons being easier to control by vaccination but providing fewer cost and QALY savings (Fig. 3). In the case of influenza this is further complicated because it is not only the transmissibility that varies from year to year but also pathogenicity and the efficacy of the vaccine (Fig. 3).
5 Conclusions
The recommendation by advisory committees, such as the Joint Committee on Vaccination and Immunisation (JCVI), to introduce universal vaccination of schoolchildren [1, 2] highlights the urgent need to understand the factors driving cost-effectiveness. This study illustrates some important methodological choices that can have a critical impact on study outcomes. It is important that decision makers are aware of these choices and their influence in economic evaluations of influenza vaccination.
References
Joint Committee on Vaccination and Immunisation (JCVI). Minutes of the meeting held on 13 April 2012. http://transparency.dh.gov.uk/2012/05/25/jcvi-meeting-april-2012/. Accessed 6 July 2012.
Murphy H. Vaccinating healthy children against flu is cost effective, says committee. BMJ. 2012;344:e3876.
Monto AS, Koopman JS, Longini IM Jr. Tecumseh study of illness. XIII. Influenza infection and disease, 1976–1981. Am J Epidemiol. 1985;121(6):811–22.
Newall AT, Jit M, Beutels P. Economic evaluations of childhood influenza vaccination: a critical review. Pharmacoeconomics. 2012;30(8):647–60.
Kelly H, Newall AT. Mortality benefits of influenza vaccination in elderly people. Lancet Infect Dis. 2008;8(8):462–3.
Simonsen L, Taylor RJ, Viboud C, et al. Mortality benefits of influenza vaccination in elderly people: an ongoing controversy. Lancet Infect Dis. 2007;7(10):658–66.
Jefferson T, Di Pietrantonj C, Al-Ansary LA, et al. Vaccines for preventing influenza in the elderly. Cochrane Database Syst Rev 2010;(2):CD004876.
Newall AT, Viboud C, Wood JG. Influenza-attributable mortality in Australians aged more than 50 years: a comparison of different modelling approaches. Epidemiol Infect. 2010;138(6):836–42.
Thompson WW, Weintraub E, Dhankhar P, et al. Estimates of US influenza-associated deaths made using four different methods. Influenza Other Respi Viruses. 2009;3(1):37–49.
Newall AT, Scuffham PA. Influenza-related disease: the cost to the Australian healthcare system. Vaccine. 2008;26(52):6818–23.
Newall AT, Wood JG, Macintyre CR. Influenza-related hospitalisation and death in Australians aged 50 years and older. Vaccine. 2008;26(17):2135–41.
Charu V, Viboud C, Simonsen L, et al. Influenza-related mortality trends in Japanese and American seniors: evidence for the indirect mortality benefits of vaccinating schoolchildren. PLoS One. 2011;6(11):e26282.
Reichert TA, Sugaya N, Fedson DS, et al. The Japanese experience with vaccinating schoolchildren against influenza. N Engl J Med. 2001;344(12):889–96.
Loeb M, Russell ML, Moss L, et al. Effect of influenza vaccination of children on infection rates in Hutterite communities: a randomized trial. JAMA. 2010;303(10):943–50.
Edmunds J, Medley GF, Nokes DJ. Evaluating the cost-effectiveness of vaccination programmes: a dynamic perspective. Stat Med. 1999;18(23):3.
Kim SY, Goldie SJ. Cost-effectiveness analyses of vaccination programmes: a focused review of modelling approaches. Pharmacoeconomics. 2008;26(3):191–215.
Brisson M, Edmunds WJ. Economic evaluation of vaccination programs: the impact of herd-immunity. Med Decis Making. 2003;23(1):76–82.
Basta NE, Chao DL, Halloran ME, et al. Strategies for pandemic and seasonal influenza vaccination of schoolchildren in the United States. Am J Epidemiol. 2009;170(6):679–86.
Vynnycky E, Pitman R, Siddiqui R, et al. Estimating the impact of childhood influenza vaccination programmes in England and Wales. Vaccine. 2008;26(41):5321–30.
Ferguson NM, Cummings DA, Cauchemez S, et al. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437(7056):209–14.
Ferguson NM, Cummings DA, Fraser C, et al. Strategies for mitigating an influenza pandemic. Nature. 2006;442(7101):448–52.
Germann TC, Kadau K, Longini IM Jr, et al. Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci USA. 2006;103(15):5935–40.
Longini IM Jr, Halloran ME, Nizam A, et al. Containing pandemic influenza with antiviral agents. Am J Epidemiol. 2004;159(7):623–33.
Longini IM Jr, Nizam A, Xu S, et al. Containing pandemic influenza at the source. Science. 2005;309(5737):1083–7.
Drummond M, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2005.
Commonwealth Department of Health and Ageing. 2006 Guidelines for the pharmaceutical industry on preparation of submissions to the Pharmaceutical Benefits Advisory Committee (PBAC) version 4.1. Canberra: Commonwealth Department of Health and Ageing; 2006.
Newall AT, Dehollain JP, Wood J. Under-explored assumptions in influenza vaccination models: implications for the universal vaccination of children. Vaccine. 2012;30(39):5776–81.
Australian Bureau of Statistics. Population by age and sex, Australian states and territories (ABS catalogue number: 3201.0). Canberra: Australian Bureau of Statistics; 2010.
Mossong J, Hens N, Jit M, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008;5(3):e74.
Agius PA, Pitts MK, Smith AMA, et al. Human papillomavirus and cervical cancer: Gardasil® vaccination status and knowledge amongst a nationally representative sample of Australian secondary school students. Vaccine. 2010;28(27):4416–22.
Australian Institute of Health and Welfare. 2009 Adult vaccination survey: summary results (AIHW catalogue number: PHE 135). Canberra: Australian Institute of Health and Welfare; 2010.
Jefferson T, Di Pietrantonj C, Rivetti A, et al. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev 2010;7(CD001269).
Vesikari T, Knuf M, Wutzler P, et al. Oil-in-water emulsion adjuvant with influenza vaccine in young children. N Engl J Med. 2012;365(15):1406–16.
Halloran ME, Haber M, Longini IM Jr. Interpretation and estimation of vaccine efficacy under heterogeneity. Am J Epidemiol. 1992;136(3):328–43.
Chowell G, Miller MA, Viboud C. Seasonal influenza in the United States, France, and Australia: transmission and prospects for control. Epidemiol Infect. 2008;136(6):852–64.
Cauchemez S, Valleron AJ, Boelle PY, et al. Estimating the impact of school closure on influenza transmission from Sentinel data. Nature. 2008;452(7188):750–4.
Longini IM Jr, Koopman JS, Haber M, et al. Statistical inference for infectious diseases. Risk-specific household and community transmission parameters. Am J Epidemiol. 1988;128(4):845–59.
Carrat F, Vergu E, Ferguson NM, et al. Time lines of infection and disease in human influenza: a review of volunteer challenge studies. Am J Epidemiol. 2008;167(7):775–85.
van Hoek AJ, Underwood A, Jit M, et al. The impact of pandemic influenza H1N1 on health-related quality of life: a prospective population-based study. PLoS One. 2011;6(3):e17030.
Chiu C, Dey A, Wang H, et al. Vaccine preventable diseases and vaccination coverage in Australia, 2005 to 2007. Commun Dis Intell. 2010;34:S1–167.
Brotherton J, Wang H, Schaffer A, et al. Vaccine preventable diseases and vaccination coverage in Australia, 2003 to 2005. Commun Dis Intell. 2007;31(Suppl):S1–152.
Amaproducts.com.au. http://www.amaproducts.com.au/FLUVAC_form.pdf. Accessed 6 July 2012.
Municipal association of Victoria. Cost of Victorian local government immunisation services. Melbourne: Municipal Association of Victoria; 2004.
Australian Government Department of Health and Ageing. Medicare benefits scheme book. Canberra: Commonwealth of Australia; 2010.
Australian Government Department of Health and Aging. Medicare statistics—September quarter 2010, average patient contribution per service—out of hospital services only; 2010.
Chemistwarehouse.com.au. http://www.chemistwarehouse.com.au/product.asp?id=58821&pname=Influvac+0.5ml+. Accessed 6 July 2012.
Australian Bureau of Statistics. Employee earnings, benefits and trade union membership, Australia, August 2010 (ABS catalogue number 6310.0). Canberra: Australian Bureau of Statistics; 2010.
Lambert SB, Allen KM, Carter RC, et al. The cost of community-managed viral respiratory illnesses in a cohort of healthy preschool-aged children. Respir Res. 2008;9:11.
Australian Bureau of Statistics. Australian labour market statistics (ABS catalogue number: 6105.0). October 2010 ed. Canberra: Australian Bureau of Statistics; 2010.
AIHW GP Statistics and Classification Unit. SAND abstract No 9 from the BEACH program: Influenza and absenteeism. 2000.
Carrat F, Sahler C, Rogez S, et al. Influenza burden of illness: estimates from a national prospective survey of household contacts in France. Arch Intern Med. 2002;162(16):1842–8.
Australian Refined Diagnosis Related Group (AR-DRG) (version 5.1) data recorded for each public patient hospitalised under the ICD categories for pneumonia and influenza.
Hawthorne G, Osborne R. Population norms and meaningful differences for the Assessment of Quality of Life (AQoL) measure. Aust N Z J Public Health. 2005;29(2):136–42.
Australian Bureau of Statistics. Life tables, Australia, 2007–2009 (ABS catalogue number: 3302.0.55.001): Commonwealth of Australia; 2010.
Newall AT, Wood JG, Oudin N, et al. Cost-effectiveness of pharmaceutical-based pandemic influenza mitigation strategies. Emerg Infect Dis. 2010;16(2):224–30.
Beutels P, Scuffham PA, MacIntyre CR. Funding of drugs: do vaccines warrant a different approach? Lancet Infect Dis. 2008;8(11):727–33.
Weinstein MC. A QALY is a QALY is a QALY—or is it? J Health Econ. 1988;7(3):289–90.
Bilcke J, Beutels P, Brisson M, et al. Accounting for methodological, structural, and parameter uncertainty in decision-analytic models: a practical guide. Med Decis Making. 2011;31(4):675–92.
Griebsch I, Coast J, Brown J. Quality-adjusted life-years lack quality in pediatric care: a critical review of published cost-utility studies in child health. Pediatrics. 2005;115(5):e600–14.
Knies S, Severens JL, Ament AJHA, et al. The transferability of valuing lost productivity across jurisdictions. Differences between national pharmacoeconomic guidelines. Value Health. 2010;13(5):519–27.
Brouwer WBF, Koopmanschap MA, Rutten FFH. Productivity costs measurement through quality of life? A response to the recommendation of the Washington Panel. Health Econ. 1997;6(3):253–9.
Acknowledgements
This research was supported by a National Health and Medical Research Council (NHMRC) grant (630779). ATN holds an NHMRC Training Fellowship (630724—Australian Based Public Health Fellowship). ATN, JGW and PB are members of a Centre for Research Excellence (CRE) funded by the NHRMC (APP1031963).
Conflict of interest
ATN and JGW have in the past received research funding from a manufacturer of influenza vaccine for other previous projects.
Contribution of Authors
ATN initiated and led the project, methodological and parameterisation decisions, designed the structure of the economic aspects of the model, reviewed the literature and drafted the manuscript. JPD and PC reviewed the literature, assisted with parameterisation, helped to develop and edit the model, performed analysis, prepared figures and tables, and edited the manuscript. JW and PB were involved in model design and parameterisation decisions, and reviewed and modified the manuscript. JW also implemented and designed technical aspects of the dynamic model including calibration methods and averaging of ICER values. All authors approved the final manuscript. ATN acts as the guarantor for the project.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Newall, A.T., Dehollain, J.P., Creighton, P. et al. Understanding the Cost-Effectiveness of Influenza Vaccination in Children: Methodological Choices and Seasonal Variability. PharmacoEconomics 31, 693–702 (2013). https://doi.org/10.1007/s40273-013-0060-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-013-0060-7