Abstract
Background
Elderly people, particularly those with dementia, are sensitive to adverse anticholinergic drug effects. This study examines the prevalence of anticholinergic medication, and anticholinergic load and its predictors, in community-dwelling elderly patients (aged 75 years and older) in Australia.
Methods
A research nurse visited the home of each participant (n = 1,044), compiled a list of current medications, and assessed participants’ cognitive status using a subsection of the revised Cambridge Examination for Mental Disorders of the Elderly (CAMCOG-R). Anticholinergic load was determined for each patient using the Anticholinergic Drug Scale (ADS).
Results
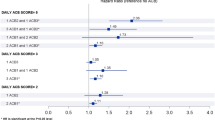
Multivariate analysis identified several patient factors that were associated with higher anticholinergic burden, including polypharmacy (i.e. taking five or more medications) (p < 0.001), increasing age (p = 0.018), CAMCOG-R dementia (p = 0.003), depression (p = 0.003), and lower physical quality of life (p < 0.001). The dementia group (n = 86) took a significantly higher number of medications (4.6 vs. 3.9; p = 0.04), and had a significantly higher anticholinergic load (1.5 vs. 0.8; p = 0.002) than those without dementia (n = 958). Approximately 60 % of the dementia group and 40 % of the non-dementia group were receiving at least one anticholinergic drug. This difference was due to the higher proportion of dementia patients taking level 1 (potentially anticholinergic) (p = 0.002) and level 3 (markedly anticholinergic) (p = 0.005) drugs.
Conclusions
There is considerable scope for the improvement of prescribing practices in the elderly, and particularly those with dementia. Importantly, level 1 anticholinergics have been identified as major contributors to the anticholinergic load in people with dementia. Longitudinal studies are required to determine the effects of increased and decreased anticholinergic load on cognitive function and other clinical outcomes for people with dementia.
Similar content being viewed by others
References
Feinberg M. The problems of anticholinergic adverse effects in older patients. Drugs Aging. 1993;3(4):335–48.
Sera LC, McPherson ML. Pharmacokinetics and pharmacodynamic changes associated with aging and implications for drug therapy. Clin Geriatr Med. 2012;28(2):273–86.
Mannesse CK, Derkx FH, de Ridder MA, Man in’t Veld AJ, van der Cammen TJ. Contribution of adverse drug reactions to hospital admission of older patients. Age Ageing. 2000;29(1):35–9.
American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4):616–31.
Schliebs R, Arendt T. The significance of the cholinergic system in the brain during aging and in Alzheimer’s disease. J Neural Transm. 2006;113(11):1625–44.
Carriere I, Fourrier-Reglat A, Dartigues JF, Rouaud O, Pasquier F, Ritchie K, et al. Drugs with anticholinergic properties, cognitive decline, and dementia in an elderly general population: the 3-city study. Arch Intern Med. 2009;169(14):1317–24.
Fox C, Richardson K, Maidment ID, Savva GM, Matthews FE, Smithard D, et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc. 2011;59(8):1477–83.
Bell JS, Mezrani C, Blacker N, LeBlanc T, Frank O, Alderman CP, et al. Anticholinergic and sedative medicines - prescribing considerations for people with dementia. Aust Fam Physician. 2012;41(1–2):45–9.
Tohgi H, Abe T, Kimura M, Saheki M, Takahashi S. Cerebrospinal fluid acetylcholine and choline in vascular dementia of Binswanger and multiple small infarct types as compared with Alzheimer-type dementia. J Neural Transm. 1996;103(10):1211–20.
Pasina L, Djade CD, Lucca U, Nobili A, Tettamanti M, Franchi C, et al. Association of anticholinergic burden with cognitive and functional status in a cohort of hospitalized elderly: comparison of the anticholinergic cognitive burden scale and anticholinergic risk scale: results from the REPOSI study. Drugs Aging. 2013;30(2):103–12.
Cancelli I, Gigli GL, Piani A, Zanchettin B, Janes F, Rinaldi A, et al. Drugs with anticholinergic properties as a risk factor for cognitive impairment in elderly people: a population-based study. J Clin Psychopharmacol. 2008;28(6):654–9.
Ancelin ML, Artero S, Portet F, Dupuy AM, Touchon J, Ritchie K. Non-degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort study. BMJ. 2006;332(7539):455–9.
Roe CM, Anderson MJ, Spivack B. Use of anticholinergic medications by older adults with dementia. J Am Geriatr Soc. 2002;50(5):836–42.
Campbell N, Boustani M, Limbil T, Ott C, Fox C, Maidment I, et al. The cognitive impact of anticholinergics: a clinical review. Clin Interv Aging. 2009;4:225.
Magin P, Goode S, Pond D. GPs, medications and older people: a qualitative study of general practitioners’ approaches to potentially inappropriate medications in older people. Aust J Ageing. 2014;. doi:10.1111/ajag.12150.
Tune LE. Anticholinergic effects of medication in elderly patients. J Clin Psychiatry. 2001;62(Suppl 21):11–4.
Gerretsen P, Pollock BG. Drugs with anticholinergic properties: a current perspective on use and safety. Expert Opin Drug Saf. 2011;10(5):751–65.
Tune L, Carr S, Hoag E, Cooper T. Anticholinergic effects of drugs commonly prescribed for the elderly: potential means for assessing risk of delirium. Am J Psychiatry. 1992;149(10):1393–4.
Chan WY, Setter SM, Sclar DA, Salek S, Corbett C, Henriksen AL. The use of anticholinergic medications in homebound elderly patients with dementia. Consult Pharm. 2006;21(5):391–9.
Bhattacharya R, Chatterjee S, Carnahan RM, Aparasu RR. Prevalence and predictors of anticholinergic agents in elderly outpatients with dementia. Am J Geriatr Pharmacother. 2011;9(6):434–41.
Sura SD, Carnahan RM, Chen H, Aparasu RR. Prevalence and determinants of anticholinergic medication use in elderly dementia patients. Drugs Aging. 2013;30(10):837–44.
Chatterjee S, Mehta S, Sherer JT, Aparasu RR. Prevalence and predictors of anticholinergic medication use in elderly nursing home residents with dementia: analysis of data from the 2004 National Nursing Home Survey. Drugs Aging. 2010;27(12):987–97.
Carnahan RM, Lund BC, Perry PJ, Chrischilles EA. The concurrent use of anticholinergics and cholinesterase inhibitors: rare event or common practice? J Am Geriatr Soc. 2004;52(12):2082–7.
Pond CD, Brodaty H, Stocks NP, Gunn J, Marley J, Disler P, et al. Ageing in general practice (AGP) trial: a cluster randomised trial to examine the effectiveness of peer education on GP diagnostic assessment and management of dementia. BMC Family Pract. 2012;13:12.
Sheikh JI, Yesavage JA. Geriatric depression scale (GDS): recent evidence and development of a shorter version. In: Brink TL, editor. Clinical gerontology: a guide to assessment. New York: Haworth Press; 1986. pp. 165–73.
Roth M, Huppert FA, Mountjoy CQ, Tym E. CAMDEX-R: the Cambridge examination for mental disorders of the elderly-revised. Cambridge: Cambridge University Press; 1998.
Hawthorne G, Herrman H, Murphy B. Interpreting the WHOQOL-Bref: preliminary population norms and effect sizes. Soc Indic Res. 2006;77(1):37–59.
Carnahan RM, Lund BC, Perry PJ, Pollock BG, Culp KR. The Anticholinergic Drug Scale as a measure of drug-related anticholinergic burden: associations with serum anticholinergic activity. J Clin Pharmacol. 2006;46(12):1481–6.
Lampela P, Lavikainen P, Garcia-Horsman JA, Bell JS, Huupponen R, Hartikainen S. Anticholinergic drug use, serum anticholinergic activity, and adverse drug events among older people: a population-based study. Drugs Aging. 2013;30(5):321–30.
Guthrie B, Clark SA, McCowan C. The burden of psychotropic drug prescribing in people with dementia: a population database study. Age Ageing. 2010;39(5):637–42.
Guthrie B, McCowan C, Davey P, Simpson CR, Dreischulte T, Barnett K. High risk prescribing in primary care patients particularly vulnerable to adverse drug events: cross sectional population database analysis in Scottish general practice. BMJ. 2011;342:d3514.
Steffensen FH, Schonheyder HC, Sorensen HT. High prescribers of antibiotics among general practitioners—relation to prescribing habits of other drugs and use of microbiological diagnostics. Scand J Infect Dis. 1997;29(4):409–13.
Egger SS, Bachmann A, Hubmann N, Schlienger RG, Krähenbühl S. Prevalence of potentially inappropriate medication use in elderly patients. Drugs Aging. 2006;23(10):823–37.
Ness J, Hoth A, Barnett MJ, Shorr RI, Kaboli PJ. Anticholinergic medications in community-dwelling older veterans: prevalence of anticholinergic symptoms, symptom burden, and adverse drug events. Am J Geriatr Pharmacother. 2006;4(1):42–51.
Schubert CC, Boustani M, Callahan CM, Perkins AJ, Carney CP, Fox C, et al. Comorbidity profile of dementia patients in primary care: are they sicker? J Am Geriatr Soc. 2006;54(1):104–9.
Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002;50(10):1723–32.
Gnjidic D, Hilmer SN, Hartikainen S, Tolppanen AM, Taipale H, Koponen M, et al. Impact of high risk drug use on hospitalization and mortality in older people with and without Alzheimer’s disease: a national population cohort study. PloS One. 2014;9(1):e83224.
Sittironnarit G, Ames D, Bush AI, Faux N, Flicker L, Foster J, et al. Effects of anticholinergic drugs on cognitive function in older Australians: results from the AIBL study. Dement Geriatr Cogn Disord. 2011;31(3):173–8.
Sanderson M, Wang J, Davis DR, Lane MJ, Cornman CB, Fadden MK. Co-morbidity associated with dementia. Am J Alzheimer’s Dis Other Dement. 2002;17(2):73–8.
Poblador-Plou B, Calderon-Larranaga A, Marta-Moreno J, Hancco-Saavedra J, Sicras-Mainar A, Soljak M, et al. Comorbidity of dementia: a cross-sectional study of primary care older patients. BMC Psychiatry. 2014;14:84.
Wang J, Zhao Z, Lin E, Zhao W, Qian X, Freire D, et al. Unintended effects of cardiovascular drugs on the pathogenesis of Alzheimer’s disease. PloS One. 2013;8(6):e65232.
Jewart RD, Green J, Lu CJ, Cellar J, Tune LE. Cognitive, behavioral, and physiological changes in Alzheimer disease patients as a function of incontinence medications. Am J Geriatr Psychiatry. 2005;13(4):324–8.
Staskin DR, Rosenberg MT, Dahl NV, Polishuk PV, Zinner NR. Effects of oxybutynin transdermal system on health-related quality of life and safety in men with overactive bladder and prostate conditions. Int J Clin Pract. 2008;62(1):27–38.
Birns J, Lukkari E, Malone-Lee JG. A randomized controlled trial comparing the efficacy of controlled-release oxybutynin tablets (10 mg once daily) with conventional oxybutynin tablets (5 mg twice daily) in patients whose symptoms were stabilized on 5 mg twice daily of oxybutynin. BJU Int. 2000;85(7):793–8.
Kay GG, Ebinger U. Preserving cognitive function for patients with overactive bladder: evidence for a differential effect with darifenacin. Int J Clin Pract. 2008;62(11):1792–800.
Mitchell AJ, Vaze A, Rao S. Clinical diagnosis of depression in primary care: a meta-analysis. Lancet. 2009;374(9690):609–19.
Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168(5):508–13.
Boustani M, Campbell N, Munger S, Maidment I, Fox C. Impact of anticholinergics on the aging brain: a review and practical application. Aging Health. 2008;4:311–20.
Pond CD, Mate KE, Phillips J, Stocks NP, Magin PJ, Weaver N, et al. Predictors of agreement between general practitioner detection of dementia and the revised Cambridge Cognitive Assessment (CAMCOG-R). Int Psychogeriatr. 2013;25(10):1639–47.
Kouladjian L, Gnjidic D, Chen TF, Mangoni AA, Hilmer SN. Drug Burden Index in older adults: theoretical and practical issues. Clin Interv Aging. 2014;9:1503–15.
van Eijk ME, Avorn J, Porsius AJ, de Boer A. Reducing prescribing of highly anticholinergic antidepressants for elderly people: randomised trial of group versus individual academic detailing. BMJ. 2001;322(7287):654–7.
He ZK, Ball PA. Can medication management review reduce anticholinergic burden (ACB) in the elderly? Encouraging results from a theoretical model. Int Psychogeriatr. 2013;25(9):1425–31.
Topinkova E, Baeyens JP, Michel JP, Lang PO. Evidence-Based strategies for the optimization of pharmacotherapy in older people. Drugs Aging. 2012;29(6):477–94.
Acknowledgments
The authors thank the project officers and research nurses involved in this project for their skilled assistance, and the patient and GP participants for their involvement. This study was supported by the Australian Government’s National Health and Medical Research Council (grant ID#351220).
Dimity Pond has received financial support for speaking from Alzheimer’s Australia, and has served on advisory boards for Pfizer, Eli Lilly, and Nutricia within the past 3 years. Henry Brodaty has been a consultant, advisory board member, and/or sponsored speaker for Eli Lilly, Merck, Baxter, Sanofi, Servier, and Tau Therapeutics. Karen Mate, Karen Kerr, Evan Williams, John Marley, Peter Disler, and Parker Magin have no conflict of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mate, K.E., Kerr, K.P., Pond, D. et al. Impact of Multiple Low-Level Anticholinergic Medications on Anticholinergic Load of Community-Dwelling Elderly With and Without Dementia. Drugs Aging 32, 159–167 (2015). https://doi.org/10.1007/s40266-014-0230-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-014-0230-0