Abstract
The aim of the present study was to investigate anticonvulsant effect of Fragaria vesca L. ethanolic etract in chemically induced epilepsy.Fragaria vesca L. ethanolic extract (FVEE) was prepared by extracting the fruit with 95 % ethanol. Seizures were induced by intraperitoneal injection of pentylenetetrazole, strychnine, isoniazid and subcutaneous injection of picrotoxin in male swiss albino mice. The in-vitro parameters were also determined including brain gamma amino butyric acid, nitric oxide.Single dose of PTZ, PTX, STR and INH resulted in resulted in hind-limb, tonic-clonic convulsion along with mortality in mice. Treatment with FVEE (250 and 500 mg/kg, p.o.) significantly and dose dependently (P < 0.01 and P < 0.001 respectively) attenuated onset of convulsion and duration of tonic convulsion induced by PTZ, PTX and INH. It also significantly inhibited the incidence of convulsion and mortality in the mice. Mice treated with FVEE (250 and 500 mg/kg, p.o.) showed significant elevation in brain GABA level and lowering in NO level as compared to vehicle treated mice. Mice treated with FVEE showed significant reduction in the locomotor activity. Treatment with FVEE failed to produce any significant change in STR induced convulsion.The findings of present investigation suggest that FVEE bears a profile similar to agent elevating the inhibitory neurotransmitter in brain and restoring the excitatory neurochemistry behind epileptic seizures. Further investigations are being carried out to characterize the biochemical nature to understand the active principles along with structure activity relationship.

Anticonvulsant activity of Fragaria vesca L. ethanolic extract: Role of GABA and NO.
Similar content being viewed by others
Introduction
Neuroinflammation is an important mechanism in the defense response to pathogenic events, traumatic injury and environmental toxins (Choi et al. 2009; Taupin 2008). It is also recognized as a major contributor to various neurological and neurodegenerative diseases such as seizure (Musto and Samii 2011). Epilepsy is a neuroinflammtory disease owing its implication to aberrant neuronal discharges imbalance in GABArgic transmission, traumatic insult and toxins affecting 50 million individual across the globe (Hachinski 1998). According to WHO around 40 to 60 per 1,000,000 population/year is an incidence rate of the epilepsy and almost 80 % of the patient lies in the developing country which do not get adequate medical treatment. An array of factors responsible for generation of epilepsy included modulation in reversible neuronal functions, reduced intracellular calcium concentration (Khanna et al. 2000; Van Luijtelaar et al. 1995).
The current therapy of epilepsy comprise of monotherapy including modern antiepileptic drugs where as some requires polypharmacy, the use of two or more anticonvulsants (Smith and Bleck 1991). Therapeutic strategies range from modulation of GABA mediated Cl- channel suppression of excitatory neurotransmitters and excessive neuronal firing. However, these therapeutic strategies suffer with a wide variety of adverse effect which need to taken care by the caregiver and healthcare team (Samren et al. 1997; Mattson 1995).
Recent advance in preclinical pharmacology allow us to mimic human condition in laboratory animals using various chemical epileptogen for development of new effective anti-epileptic drugs with minimal side effect (Rogawski 2006).
Currently the synthetic moieties which are available for the treatment of epilepsy possess an array of side effects. Thus, there is an urgent need of development of novel drugs which are having better safety and efficacy with fewer side effects. Traditional systems of medicine are popular in developing countries and herbal therapies have an advantage of being safe, effective and promise better patient compliance due to their therapeutic profile (Farnsworth 1988).
Fragaria vesca (wild strawberry), belongs to the family Rosaceae. Whole plant contains flavonoids, tannins, volatile oils, methyl salisylate and borneol (Agrawal and Paridhavi 2007). Its fruits have been implicated in treatment of liver and kidney diseases. Earlier studies have shown that it possesses analgesic (Kanodia and Das 2008), anti-inflammatory, antioxidant (Wang and Lin 2000) potential. It also used in the treatment of rheumatism, gout (Phillips and Foy 1990) and inflammatory bowel disease (Kanodia et al. 2011).
The present investigation was designed to study the effect of ethanolic extract of Fragaria vesca L. on various animal models of epilepsy by determining various behavioral and biochemical parameters in laboratory mice.
Materials and methods
Collection of plant material
The fruits of Fragaria vesca L. were collected from rural areas of Mahableshwar, Satara district, Maharashtra in the month of October 2011. Authentication of Plant was carried out by P.G. Diwakar, Joint Director, Botanical Survey of India, Pune.
Preparation of extract and dose
The fresh fruits (1 kg) of Fragaria vesca L. were peeled, washed, cut into small pieces and homogenized in blender without adding water. Thereafter it was extracted with 95 % ethanol using soxhlet extractor, at room temperature (The Chemist and Druggist, 1950). The ethanolic extract was filtered and concentrated by distillation process. A net yield of 12.3 % w/w was obtained which was kept in a desiccator. The doses of FVEE were selected on the basis of previous studies (Kanodia and Das 2008).
Preliminary phytochemical screening
The Preliminary phytochemical screening of the Fragaria vesca L. ethanolic extract (FVEE) was carried out according to the methods described by Khandelwal 2001.
Animals
Adult male Swiss albino mice (18–22 g) were purchased from National Institute of Biosciences, Pune and housed in quarantine for one week at the institute animal house in groups of six animals per cage at standard laboratory conditions at a temperature of 24°C ± 1°C, relative humidity of 45–55 % and 12:12 h dark and light cycle. The experiments were carried out between 10:00 am to 5:00 pm. Animals had free access to food (standard chaw pellet, Pranav Agro industries Ltd., Sangli, India) and water ad libitum. The research protocol was approved by the Institutional Animal Ethics Committee (IAEC) (CPCSEA/27/2010) and performed in accordance with the guidelines of Committee for Control and Supervision of Experimentation on Animals (CPCSEA), Government of India on animal experimentation. Animals were brought to testing laboratory 1 h before the experimentation for adaptation purpose. The experimentation was carried out in noise free area.
Drugs and chemicals
Pentylenetetrazole (PTZ) (Sigma Aldrich, India), Strychnine (STR) (Sigma Aldrich India), Phenytoin (PHY) (Eptoin®, Sun Pharma Ltd., India), Diazepam (DZP) (Calmpose®, Ranbaxy Ltd., India) and Isoniazid (INH) (Solonex®, Macleods, Mumbai, India) were used in present study. All chemicals were dissolved in saline. All other reagents were purchased from S.D. Fine Chemicals, Mumbai, India.
Assessment of anticonvulsant activity
Pentylenetetrazole (PTZ) induced convulsions
The mice were randomly divided into five groups containing six mice in each group as follows:
-
Group I: FVEE (100 mg/kg, i.p.);
-
Group II: FVEE (250 mg/kg, i.p.);
-
Group III: FVEE (500 mg/kg, i.p.);
-
Group IV: Diazepam (5 mg/kg, i.p.);
-
Group V: Vehicle control (distilled water, i.p.).
A previously reported protocol was followed to induced convulsion using PTZ (Nisar et al. 2008). Vehicle, test drug and standard drugs were administered by intraperitoneal (i.p.) route. PTZ (90 mg/kg) was injected intraperitoneally to mice 45 min after intraperitoneal (i.p.) administration of vehicle (1 % DMSO) or test drug (FVEE) and 30 min after the standard (diazepam) drug. Immediately after PTZ administration mice were observed for next 30 min for following symptoms:
-
Onset of convulsion
-
duration of clonic convulsion
-
duration of tonic convulsion
-
incidence (number of mice showing convulsions);
-
mortality
Picrotoxin (PTX) induced convulsions
The mice were randomly divided into six groups containing six mice in each group as follows:
-
Group I: FVEE (100 mg/kg, i.p.);
-
Group II: FVEE (250 mg/kg, i.p.);
-
Group III: FVEE (500 mg/kg, i.p.);
-
Group IV: Diazepam (5 mg/kg, i.p.);
-
Group V: Vehicle control (distilled water, i.p.).
A previously reported protocol was followed to induced convulsion using PTX (Vogel and Vogel 2002). Vehicle, test drug and standard drugs were administered by intraperitoneal (i.p.) route. PTX (3.5 mg/kg) was injected subcutaneously to mice 45 min after intraperitoneal (i.p.) administration of vehicle (1 % DMSO) or test drug (FVEE) and 30 min after the standard (diazepam) drug. Immediately after PTX administration mice were observed for next 30 min for following symptoms:
-
Onset of convulsion
-
duration of clonic convulsion
-
duration of tonic convulsion
-
incidence (number of mice showing convulsions);
-
mortality
Strychnine (STR) induced convulsions
The mice were randomly divided into five groups containing six mice in each group as follows:
-
Group I: FVEE (100 mg/kg, i.p.);
-
Group II: FVEE (250 mg/kg, i.p.);
-
Group III: FVEE (500 mg/kg, i.p.);
-
Group IV: Phenytoin (25 mg/kg, i.p.);
-
Group V: Vehicle control (distilled water, i.p.).
A previously reported protocol was followed to induced convulsion using STR (Quintans-Junior et al. 2008). Vehicle, test drug and standard drugs were administered by intraperitoneal (i.p.) route. STR (5 mg/kg) was injected intraperitoneally to mice 45 min after intraperitoneal (i.p.) administration of vehicle (1 % DMSO) or test drug (FVEE) and 30 min after the standard (phenytoin) drug. Immediately after STR administration mice were observed for next 60 min for following symptoms:
-
Onset of convulsion
-
duration of clonic convulsion
-
duration of tonic convulsion
-
incidence (number of mice showing convulsions);
-
mortality
Isoniazid (INH) induced convulsions
The mice were randomly divided into five groups containing six mice in each group as follows:
-
Group I: FVEE (100 mg/kg, i.p.);
-
Group II: FVEE (250 mg/kg, i.p.);
-
Group III: FVEE (500 mg/kg, i.p.);
-
Group IV: Diazepam (5 mg/kg, i.p.);
-
Group V: Vehicle control (distilled water, i.p.).
A previously reported protocol was followed to induced convulsion using INH (Vogel and Vogel 2002). Vehicle, test drug and standard drugs were administered by intraperitoneal (i.p.) route. INH (300 mg/kg) was injected intraperitoneally to mice 45 min after intraperitoneal (i.p.) administration of vehicle (1 % DMSO) or test drug (FVEE) and 30 min after the standard (diazepam) drug. Immediately after INH administration mice were observed for next 120 min for following symptoms:
-
Onset of convulsion
-
duration of clonic convulsion
-
duration of tonic convulsion
-
incidence (number of mice showing convulsions);
-
mortality
Locomotor activity
Mice were acclimatized with environment and placed individually in an actophotometer for 10 min and a basal activity score was obtained. Subsequently they were divided into five groups with six animals in each group and all the groups except Group II, were treated as per MES induced seizure model. Group II, positive control was received diazepam (5 mg/kg, i.p.). After 30 min, the activity score was recorded (Kulkarni 1999). The percentage reduction in locomotor activity was calculated.
Biochemical evaluation
Brain GABA estimation
Sample preparation
Forty-five minutes after vehicle (1 % DMSO) or FVEE and 30 min after diazepam (5 mg/kg), Phenytoin (25 mg/kg) mice were sacrificed. PTZ (90 mg/kg), INH (300 mg/kg) and STR (3 mg/kg) treated animals were sacrificed as soon as onset of convulsions occurs. Animals which received PTZ (90 mg/kg), INH (300 mg/kg) and STR (3 mg/kg) after 45 min of FVEE (10 and 25 mg/kg) and sacrificed at the exact time of onset of convulsions. Brain was isolated immediately and transferred to homogenization tube containing 5 ml of chilled 0.01 N hydrochloric acid and homogenized. Brain homogenate was transferred to bottle containing 8 ml of ice cold absolute alcohol and kept for 1 hour at 0°C. The contents were centrifuged for 10 min at 16000 rpm, supernatant was collected in petridish. Precipitate was washed with 3–5 ml of 75 % alcohol for three times and washes were combined with supernatant. Contents in petridish were evaporated to dryness at 70–90°C on water bath under stream of air. To the dry mass 1 ml water and 2 ml chloroform were added and centrifuged at 2000 rpm. Upper phase containing GABA was separated and 10 μl of it was applied as spot on Whatman paper (No. 41).
Chromatographic conditions
The mobile phase consisted of n-butanol (50 ml) acetic acid (12 ml) and water (60 ml). The chamber was saturated for half hour with mobile phase. The paper chromatogram was developed with ascending technique. The paper was dried in hot air and then spread with 0.5 % Ninhydrin solution in 95 % ethanol. The paper was dried for 1 h at 90°C. Blue color spot developed on paper was cut and heated with 2 ml ninhydrin solution on water bath for 5 min. water (5 ml) was added to solution and kept for 1 h Supernatant was decanted and absorbance was measured at 570 nm.
Standards and calculations
Stock solution of standard GABA, 1 mg/ml was prepared in 0.01 N HCl. Serial dilutions were prepared to get concentrations 1 ng/10 μl to 1000 ng/10 μl. To obtain a standard concentration curve for GABA same procedure was followed replacing brain homogenate with standard GABA solutions (Maynert et al. 1962).
Estimation of nitrite/nitrate level
The NO level was estimated as nitrite by the acidic Griess reaction after reduction of nitrate to nitrite by vanadium trichloride according to previously described method (Miranda et al. 2001). The Griess reaction relies on a simple colorimetric reaction between nitrite, sulfonamide and N-(1- naphthyl) ethylenediamine to produce a pink azo-product with maximum absorbance at 543 nm. The concentrations were determined using a standard curve of sodium nitrate and the results were expressed as μg/ml.
Statistical analysis
Data were expressed as mean ± standard error mean (SEM). The data was analyzed using one-way analysis of variance (ANOVA), Dunnett’s multiple range test was applied for post hoc analysis. Data of ‘incidence of convulsion’ was analyzed by Chi2 test. Data of ‘mortality’ was analyzed by Fisher’s exact test. Analysis of all the statistical data was performed using GraphPad Prism 5.0 (GraphPad, San Diego, USA). P < 0.05 was considered as statistically significant.
Results
Preliminary phytochemical screening
The ethanolic extract of Fragaria vesca L. fruit was screened for various chemical tests as per the reported methods and was found to contain Alkaloids, carbohydrates, flavonoids, protein, saponin and polyphenols.
Effects of FVEE and diazepam on pentylenetetrazole induced convulsions in mice
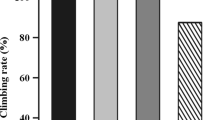
Single dose of PTZ (90 mg/kg) administration resulted in hind-limb, tonic-clonic convulsion as well as mortality in mice. It also significantly decreased (P < 0.001) brain GABA level and significantly elevated (P < 0.001) nitric oxide level as compared to normal mice. Mice pretreated with FVEE (250 and 500 mg/kg, p.o.) significantly (P < 0.01 and P < 0.001 respectively) and dose dependently delayed onset of convulsion as compared to PTZ control mice. When compared with PTZ control mice, treatment with FVEE (100, 250 and 500 mg/kg, p.o.) significantly (P < 0.05, P < 0.01 and P < 0.001 respectively) and dose dependently decreased duration of tonic convulsion where as mice treated with FVEE (500 mg/kg, p.o.) showed significant reduction (P < 0.05) in duration of clonic convulsion. Treatment with FVEE (100 and 250 mg/kg, p.o.) failed to produce any significant reduction in duration of clonic convulsion as compared to PTZ control mice (Fig. 1).
Mice treated with FVEE (100, 250 and 500 mg/kg, p.o.) significantly (P < 0.05, P < 0.01 and P < 0.001 respectively) and dose dependently decreased PTZ induced mortality in the mice. It also significantly decreased incidence of convulsion at a dose of 250 and 500 mg/kg, p.o. (P < 0.01 and P < 0.001 respectively). Treatment with FVEE (100, 250 and 500 mg/kg, p.o.) significantly (P < 0.05, P < 0.01 and P < 0.001 respectively) and dose dependently increased level of brain GABA as compared to PTZ control mice. It significantly attenuated the elevated level of brain NO at a dose of 250 and 500 mg/kg, p.o. (P < 0.01 and P < 0.001 respectively). However, treatment with diazepam (5 mg/kg, i.p.) significantly antagonized (P < 0.001) behavioral and biochemical aberrations induced by a single dose of PTZ (90 mg/kg, i.p.) (Table 1).
Effects of FVEE and diazepam on picrotoxin induced convulsions in mice
Subcutaneous injection of PTX (3.5 mg/kg) resulted in hind-limb, tonic-clonic convulsion along with lethality in mice. A significant decreased (P < 0.001) in brain GABA and increased (P < 0.001) in brain NO was found in mice treated with PTX (3.5 mg/kg, s.c.). Treatment with FVEE (500 mg/kg, p.o.) significantly (P < 0.01) delayed onset of convulsion and decreased duration of clonic (P < 0.05) as well as tonic (P < 0.001) convulsion as compared to PTX control mice. Mice treated with FVEE (100 and 250 mg/kg, p.o.) did not produced any significant delay in onset on convulsion and duration of tonic convulsion as compared PTX control mice (Fig. 2).
When compared with PTX control mice, treatment with FVEE (100, 250 and 500 mg/kg, p.o.) failed to produced any significant change in level of brain GABA and NO. However, mice treated with diazepam (5 mg/kg, i.p.) significantly attenuated (P < 0.001) PTX induced alteration in the brain GABA and NO level. It significantly delayed (P < 0.001) onset on convulsion as well as significantly decreased (P < 0.001) duration of hind limb clonic-tonic convulsion as compared to PTX control mice. Mice treated with diazepam (5 mg/kg, i.p.) significantly reduced (P < 0.001) PTX induced mortality in mice as well as it significantly attenuated (P < 0.001) incidence of convulsion as compared to PTX control mice. The brain GABA and NO level was also significantly attenuated by diazepam (5 mg/kg, i.p.) treatment (Table 2).
Effects of FVEE and phenytoin on strychnine induced convulsions in mice
Intraperitoneal injection of STR (5 mg/kg) induced clonic convulsions followed by THLE and mortality in mice. It also significantly increased (P < 0.001) level of brain NO as compared to normal mice. Treatment with FVEE (500 mg/kg, p.o.) significantly delayed (P < 0.05) onset of convulsion as well as decreased (P < 0.05) duration of tonic convulsion as compared to STR control mice. Mice treated with FVEE (100 and 250 mg/kg, p.o.) failed to produced any significant change in duration of onset of convulsion as well as duration of clonic-tonic convulsion (Fig. 3). It also did not showed any significant protection against STR induced mortality in mice and incidence of convulsion. Whereas mice treated with phenytoin (25 mg/kg, i.p.) significantly antagonized (P < 0.001) duration of hind-limb, tonic-clonic convulsion. It also significantly protects the mice from STR induced morality (P < 0.001) as well as incidence of convulsion (P < 0.001). Treatment with phenytoin (25 mg/kg, i.p.) significantly attenuated (P < 0.001) effect produced by the STR on brain GABA and NO level (Table 3).
Effects of FVEE and diazepam on isoniazid induced convulsions in mice
Elicited tonic-clonic convulsions followed by THLE was produced in isoniazid (300 mg/kg i.p.) treated mice. Mice treated with FVEE (100, 250 and 500 mg/kg, p.o.) significantly and dose dependently (P < 0.05, P < 0.01 and P < 0.001 respectively) delayed the onset of convulsion as compared to INH control mice where as it significantly and dose dependently (P < 0.05, P < 0.01 and P < 0.001 respectively) attenuated the duration of tonic convulsion in mice as compared to INH control mice (Fig. 4).
FVEE (250 and 500 mg/kg, p.o.) treated mice showed significant protection against incidence of convulsion (P < 0.01) and INH induced mortality in mice (P < 0.05). Brain GABA level was significantly and dose dependently (P < 0.05 and P < 0.01 respectively) increased in mice treated with FVEE (250 and 500 mg/kg, p.o.) as compared to INH control mice. However as compared to INH control mice, FVEE (500 mg/kg, p.o.) treated mice showed significant decreased (P < 0.01) in brain NO level. Diazepam (5 mg/kg, i.p.) treated mice significantly antagonized (P < 0.001) behavioral and biochemical alteration produced by INH as compared to INH control mice (Table 4).
Effects of FVEE and diazepam on locomotor activity
The locomotor activity in FVEE (250 and 500 mg/kg, p.o.) treated mice was significantly and dose dependently (P < 0.01 and P < 0.001 respectively) reduced as compared to normal mice. Similarly, treatment with standard DZP (5 mg/kg, i.p.) also showed significant (P < 0.001) reduction in the locomotor activity when compared to normal mice (Table 5).
Discussion
Epilepsy is a common chronic neurological ailment caused due to tumours, degenerative conditions or cerebrovascular diseases. Experimental epilepsy in laboratory animals is exhibited by various chemical such as pentylenetetrazole (PTZ), picrotoxin (PTX), isoniazid (INH) and strychnine (STR). These chemicals have discrete mechanism independent of each other. However, the behavioral features of convulsion are identical, physiological, pathobiological is exhibited via visually discernable behavioral parameters which include tonic, clonic seizures, onset of convulsion, mortality and incidence of convulsion. However, underlying molecular perturbations are independent of each of these animal models (McNamara 1994). Hence, it is necessary to subject the drug to these chemicals to understand the mechanism of action of Fragaria vesca.
The biochemical parameters determined were GABA and nitric oxide (NO). It has been reiterated in literature that these neurotransmitters are modulated in epileptic stress in rodent models (Rohkamm 2004; Dawson and Snyder 1994). GABA is the major inhibitory neurotransmitter in the brain while NO acts as a multifunctional messenger and neurotransmitter, which causes activation of the cycline Guanine Monophosphate (cGMP) via guanylate cyclase in the CNS. An increase in cGMP follows stimulation of L-glutamate and result in convulsion (Zandieh et al. 2010). Hence, these biomarkers were traced and their levels measured to provide an insight in the neurochemical changes occurring due to epileptic stress and its amelioration by FVEE.
Pentylenetetrazole (PTZ) is an antagonist at GABA mediated Cl- channels thereby damaging the endogenous antiepileptic activity of GABA (Samini et al. 2005; De Sarro et al. 1999). Diazepam exerts its anticonvulsant effects by enhancing GABA mediated inhibition in the brain (Rang et al. 2005). The behavioral changes along with neurochemical alteration were restored in the animals treated with FEVV proving its mechanism to be mediated by activation of GABA mediated Cl- channel. It also significantly reduced the elevated level of brain nitric oxide. The result of present investigation was in accordance with the previous findings (Mudnic et al. 2009).
Picrotoxin has malefic effect on the suppressed calcium released. Calcium released is limited in normal physiological condition which becomes uninterrupted leading to excess calcium released which precipitate exitotoxicity (Rang et al. 2005). Diazepam and FEVV showed significant amelioration property in PTX induced convulsion i.e. delay in the latency of picrotoxin–induced seizures as well as mortality in mice via its ability to modulate calcium channel in brain.
Glycine is inhibitory neurotransmitter, maintaining electrophysiological balance concomitantly with excitatory neurotransmitter like glutamate and aspartate (Rang et al. 2005). Imbalance in the level of these excitatory and inhibitory neurotransmitters may lead to convulsions. STR is a glycine synthesis inhibitor and hence precipitated seizure in laboratory animals (Parmar and ShivPrakash 2006). However, FVEE did not significantly ameliorate these changes which were reflected by its inability to protect animals from STR induced seizures.
Glutamic acid and aspartic acid are excitatory neurotransmitter where as GABA and glycine are inhibitory neurotransmitters. Glutamic acid decarboxylase (GAD) is responsible for maintainace of physiological level of glutamic acid and inhibits excess excitation produced by glutamate and aspartate (Vergnes et al. 2000). When this balance is altered then epileptic seizures are exhibited. INH inhibits glutamic acid decarboxylase leading to increased amount of glutamate and decreased GABA level. The excitatory neurotransmitter instigates neuronal firing and epileptic seizures. FVEE significantly ameliorated the biochemical factors which intern is responsible for behavioral neurological discrepancies.
Elevated level of brain GABA is associated with the decrease in dopaminergic transmission which leading to decreased locomotor activity (Sokoloff et al. 1990). Locomotor activity is considered as an indicator of alertness, and a decrease indicates a sedative effect (Thakur and Mengi 2005). Mice treated with the diazepam and FVEE showed significant decreased in locomotor activity revealing its mechanism action via regulation of brain GABA.
The phytochemical screening of the ethanolic extract of Fragaria vesca L. (FVEE) showed the presence of alkaloids, cardiac glycosides, phenolic compounds, flavonoids and saponins. The result of present investigation is in accordance with earlier report by Agrawal and Paridhavi 2007. It has been well documented that alkaloids, flavonoids, phenolic compounds as well as triterpenoidal saponins possess anticonvulsant activity in experimental models of epilepsy including PTZ (Kasture et al. 2002; Chauhan et al. 1988) and PTX (Librowski et al. 2000; Brum et al. 2001).
Recently many herbal drugs have been proven clinically for treatment of idiopathic epilepsy including Atropa belladonna (Varshney 2007) and Ginkgo biloba (Harms et al. 2006). Hence, it could be deduced that FVEE bears a profile similar to an agents elevating inhibitory neurotransmitters in brain and restoring the excitatory neurochemistry behind epileptic seizures. Further investigations are being carried out to characterize the biochemical nature to understand the active principles along with structural activity relationship.
References
Agrawal SS, Paridhavi M (2007) Essentials of crude drugs. In: Herbal drug technology. 1st ed. Hyderabad, India, Universities Press, pp 583–87.
Brum LF, Elisabetsky E, Souza D (2001) Effects of linalool on [(3) H] MK801 and [(3) H] muscimol binding in mouse cortical membranes. Phytother Res 5:422–425
Chauhan AK, Dobhal MP, Joshio BC (1988) A review of medicinal plant showing anticonvulsant activity. J Ethnopharmacol 22:11–23
Choi J, Nordli DR Jr, Alden TD, DiPatri A Jr, Laux L, Kelley K et al (2009) Cellular injury and neuroinflammation in children with chronic intractable epilepsy. J Neuroinflammation 19(6):38
Dawson TM, Snyder SH (1994) Gases as biological messengers: nitric oxide and carbon monoxide in the brain. J Neurosci 14:5147–5159
De Sarro A, Cecchetti V, Fravoloni V, Naccari F, Tabarrinia O, De Sarro G (1999) Effects of novel 6-desfluoroquirolones and classic quinolones on pentylenetetrazole-induced seizure in mice. Antimicrob Agents Chemother 43:1729–1736
Extracta liquid-liquid extracts (1950) In: Pharmaceutical formulos. 1st ed. London, England, The Chemist and Druggist, p 183
Farnsworth NR (1988) Screening plants for new medicines. In: Wilson EO (ed) Biodiversity, Chapter 9 Part II. National Academy Press, Washington DC, pp 83–97
Hachinski V (1998) New antiepileptic drugs: the cost of innovation. Arch Neurol 55:1142
Harms SL, Garrard J, Schwinghammer P, Eberly LE, Chang Y, Leppik IE (2006) Ginkgo biloba use in nursing home elderly with epilepsy or seizure disorder. Epilepsia 47(2):323–329
Kanodia L, Das S (2008) A comparative study of analgesic property of whole plant and fruit extracts of Fragaria vesca in experimental animal models. Bangladesh J Pharmacol 4:35–38
Kanodia L, Borgohain M, Das S (2011) Effect of fruit extract of Fragaria vesca L. on experimentally induced inflammatory bowel disease in albino rats. Indian J Pharmaco 43:18–21
Kasture VS, Kasture SB, Chopde CT (2002) Anticonvulsive activity of Butea monosperma flowers in laboratory animals. Pharmacol Biochem Behav 72:965–972
Khandelwal KR (2001) Preliminary phytochemicals screening, In: Practical pharmacognosy Techniques and Experiments. 8th edn. Nirali Publication, Pune, pp 149–156
Khanna N, Bhalla S, Verma V, Sharma KK (2000) Modulatory effects of nifedipine and nimodipine in experimental convulsions. Indian J Pharmacol 32(6):347–352
Kulkarni SK (1999) Hand book of experimental pharmacology. Vallabh Prakashan, New Delhi, pp 117–119
Librowski T, Czarnecki R, Mendyk A, Jastrzebska M (2000) Influence of new monoterpenes homologues of GABA on the central nervous system activity in mice. Polish J Pharmacol 52:317–321
Mattson RH (1995) Efficacy and adverse effects of established and new antiepileptic drugs. Epilepsia 36(2):S13–S26
Maynert EW, Klingman GI, Kaji HK (1962) Tolerance to morphine. II. Lack of effects on brain 5-HT and GABA. J Pharmacol Exp Ther 135:296–299
McNamara JO (1994) Cellular and molecular basis of epilepsy. J Neurosci 14:3413–3425
Miranda K, Espy MG, Wink DA (2001) A rapid and simple spectrophotometric method for simultaneous detection of nitrate and nitrite. Nitric Oxide 5:62–71
Mudnic I, Modun D, Brizic I, Vukovic J, Generalic I, Katalinic V et al (2009) Cardiovascular effects in vitro of aqueous extract of wild strawberry (Fragaria vesca, L.) leaves. Phytomedicine 16(5):462–469
Musto AE, Samii M (2011) Platelet-activating factor receptor antagonism targets neuroinflammation in experimental epilepsy. Epilepsia 52(3):551–561
Nisar M, Khan I, Simjee SU, Gilani AH, Obaidullah PH (2008) Anticonvulsant, analgesic and antipyretic activities of Taxus wallichiana Zucc. J Ethnopharmacol 116:490–494
Parmar NS, Shiv Prakash (2006) Screening methods in Pharmacology. Narosa Publishing House, New Delhi, pp 90–91
Phillips R, Foy N (1990) London: Herbs Pan Books Ltd., Plants for a future: edible, medicinal and useful plants for a healthier world. Accessed on 25th May, 2008, at www.pfaf.org/index.htm
Quintans-Junior LJ, Souza TT, Leite BS, Lessa NMN, Bonjardim LR, Santos MRV et al (2008) Phythochemical screening and anticonvulsant activity of Cymbopogon winterianus Jowitt (Poaceae) leaf essential oil in rodents. Phytomedicine 15:619–624
Rang HP, Dale MM, Ritter JM, Moore PK (2005) Pharmacology, 5th edn. Churchill Livingstone, India, pp 456–473
Rogawski MA (2006) Molecular target versus models for new antiepileptic drug discovery. Epilepsy Res 68:22–28
Rohkamm R (2004) Epilepsy: seizures and types. In: Colour Atlas of Neurology, Malestrom. Thieme Flexi book, 2nd edn. Georg Thieme Verlag, Stuttgart, pp 192–196
Samini M, Shafaroodi H, Sehat VS (2005) Comparison of the effects of lindane and permethrin on pentylenetetrazole-induced clonic seizure in mice. Online J Vet Res 9(1):37–47
Samren EB, Van Duijn CM, Koch S, Hiilesmaa VK, Klepel H, Bardy AH et al (1997) Maternal use of antiepileptic drugs and the risk of major congenital malfor malformations: a joint European prospective study of human teratogenesis associated with maternal epilepsy. Epilepsia 38:981–990
Smith MC, Bleck TP (1991) Convulsive disorders: toxicity of anticonvulsants. Clin Neuropharmacol 14:97–115
Sokoloff P, Giros B, Martres MP, Bouthenet ML, Schwartz JC (1990) Molecular cloning and characterization of a novel dopamine receptor (D3) as a target for neuroleptics. Nature 347:146–151
Taupin P (2008) Adult neurogenesis, neuroinflammation and therapeutic potential of adult neural stem cells. Int J Med Sci 5(3):127–132
Thakur VD, Meng SA (2005) Neuropharmacological profile of Eclipta alba (Linn.) Hassk. J Ethnopharmacol 31:102(1):23–31
Van Luijtelaar ELJM, Ales N, Coenen AML (1995) Role of L-type calcium channel modulation in nonconvulsive epilepsy in rats. Epilepsia 36(1):86–92
Varshney JP (2007) Clinical management of idiopathic epilepsy in dogs with homeopathic Belladonna 200C: a case series. Homeopathy 96:46–48
Vergnes M, Boehrer A, Reibel S, Simler A, Marescaux C (2000) Selective susceptibility to inhibitors of GABA synthesis and antagonists of GABAA receptor in rats with genetic absence epilepsy. Exp Neurol 161:714–723
Vogel HG, Vogel WH (2002). In: Psychotropic and neurotropic activity. Drug discovery and evaluation: pharmacological assays, Editors: Vogel WH, Schlkens BA, Sandow J, et al., 2nd edn. Springer, Berlin, Germany, pp 422–424
Wang SY, Lin HS (2000) Antioxidant activity in fruits and leaves of blackberry, raspberry, and strawberry varies with cultivar and developmental stage. J Agric Food Chem 48(2):140–146
Zandieh A, Maleki F, Hajimirzabeigi A, Zandieh B, Khalilzadeh O et al (2010) Anticonvulsant effect of celecoxib on pentylenetetrazole-induced convulsion: Modulation by NO pathway. Acta Neurobiol Exp 70:390–397
Acknowledgements
The authors would like to acknowledge Prof. R. D. Patankar, Principal, Abhinav College of Pharmacy and Dr. S. L. Bodhankar, Head and Professor, Department of Pharmacology, Poona College of Pharmacy, Bharati Vidyapeeth Deemed University, Pune, India for their constant support and valuable suggestions for the research work. We are also thankful to Dr. Vasant Narke, Director, TOXINDIA, Pune, India for providing necessary facilities to carry out the study.
Disclosure of interest
There is no conflict of interest between any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patil, M.V.K., Kandhare, A.D., Ghosh, P. et al. Determination of role of GABA and nitric oxide in anticonvulsant activity of Fragaria vesca L. ethanolic extract in chemically induced epilepsy in laboratory animals. Orient Pharm Exp Med 12, 255–264 (2012). https://doi.org/10.1007/s13596-012-0072-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13596-012-0072-4