Abstract
Background
By 2030, 80 % of people with diabetes will be living in developing countries.
Purpose
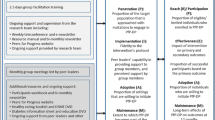
The purpose of this pre-post quasi-experimental study was to test the feasibility of a peer intervention to improve the following: (1) diabetes self-care behaviors, (2) glycemic control, (3) social support and emotional well-being, (4) linkages to health care providers, and (5) to assess the sustainability of the intervention 18 months later.
Method
Participants were adults with type 2 diabetes who resided in rural Uganda. Participants (n = 46) attended a 1-day diabetes education program and agreed to make weekly contacts over 4 months with each other by phone or in person to assist with daily management, provide social and emotional support, and encourage appropriate contact with health care providers.
Results
Results indicated improvement in glycosylated hemoglobin (A1C), diastolic blood pressure, and eating behaviors.
Conclusions
A short-term peer support program was a feasible intervention to improve diabetes care in rural Uganda. Participants were successfully recruited and retained, and they experienced positive behavioral and physiologic outcomes. Elements of the intervention were sustained 18 months after the intervention.

Similar content being viewed by others
References
International Diabetes Federation [IDF]. A Call to Action. Brussels: Author; 2010. Accessed 11 April 2011 from http://www.idf.org/webdata/Call-to-Action-on-Diabetes.pdf.
International Diabetes Federation. IDF Diabetes Atlas, 5th ed. Brussels, Belgium: Author; 2012. (www.idf.org/diabetesatlas/5e).
World Health Organization [WHO]. Counting health workers: definitions, data, methods and global results. Geneva: WHO; 2007.
World Health Organization. Peer support programmes in diabetes. Geneva: WHO; 2008.
Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, et al. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med. 2005;143:427–38.
Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2010;288:2469–75.
Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med. 2010;153:507–15.
Less LA, Ragoobirsingh D, Morrison EY, Boyne M, Anderson JP. A preliminary report on an assessment of a community-based intervention for diabetes control in adults with type 2 diabetes. Fam Pract. 2010;27 suppl 1:i46–52.
Egede LE, Nietert PJ, Zheng D. Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. 2005;28:1339–45.
Fortmann AL, Gallo LC, Walker C, Philis-Tsimikas A. Support for disease management, depression, self-care, and clinical indicators among Hispanics with type 2 diabetes in San Diego County, United States of America. Rev Panam Salud Publica. 2010;28:230–4.
Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ. 2009;35:641–51.
Piette JD. Interactive behavior change technology to support diabetes self-management: where do we stand? Diabetes Care. 2007;30:2425–32.
Gill G, Mbanya JC, Rmaiya KL, Tesfaye S. A sub-Saharan African perspective of diabetes. Diabetologia. 2009;52:8–16. doi:10.1007/s00125-008-1167-9.
Coleman R, Gill G, Wilkinson D. Noncommunicable disease management in resource-poor settings: a primary care model from rural South Africa. Bull World Health Organ. 1998;76:633–40.
Gill GV, Price C, Shandu D, Dedicoatt M, Wilkinson D. An effective system of nurse-led diabetes care in rural Africa. Diabet Med. 2008;25:606–11. doi:10.1111/j.1464-5491.2008.02421.
Labhardt ND, Balo J, Ndam M, Grimm J, Manga E. Task shifting to non-physician clinicians for integrated management of hypertension and diabetes in rural Cameroon: a programme assessment at two years. BMC Health Serv Res. 2010;10:339. doi:10.1186/1472-6963-10-339.
Price C, Shandu D, Dedicoat M, Wilkinson D. An effective system of nurse-led diabetes care in rural Africa. Diabet Med. 2008;25:606–11.
Price C, Shandu D, Dedicoat M, Wilkinson D, Gill GV. Long-term glycaemic outcome of structured nurse-led diabetes care in rural Africa. Q J Med. 2011. doi:10.1093/qjmed/hcr005.
Lekoubou A, Awah P, Fezeu L, Sobngwi E, Kengne AP. Hypertension, diabetes mellitus, and task shifting in their management in sub-Saharan Africa. Int J Environ Res Public Health. 2010;7:353–63.
Funnell MM. Peer-based behavioural strategies to improve chronic disease self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Fam Pract. 2010;27 suppl 1:i17–22. doi:10.1093/fampra/cmp027.
Nettles A, Belton A. An overview of training curricula for diabetes peer educators. Fam Pract. 2010;27 suppl 1:i33–9. doi:10.1093/fampra/cmn102.
Farrell B. Author response. BMJ, accessed 30 April 2011 from http://www.bmj.com/content/342/bmj.d715.abstract/reply#bmj_el_254041. 2011, March.
Fisher EB, Boothroyd RI, Coufal MM, Baumann LC, Mbanya JC, Rotheram-Borus MJ, et al. Peer support for self-management of diabetes improved outcomes in international settings. Health Aff. 2012;31:1–11. doi:10.1377/hlthaff.20211.0914.
Fisher EB, Earp JA, Maman S, Zolotor A. Cross-cultural and international adaptation of peer support for diabetes management. Fam Pract. 2010;27 suppl 1:i6–i16. doi:10.1093/fampra/cmp013.
Merck & Co. The ABCs of diabetes: your personal guide to managing diabetes. Merck & Co; 2008.
American Association of Diabetes Educators. Diabetes self-management and assessment tool®. Chicago: Author; 2000.
Peyrot M, Peeples M, Tomky D, Charron-Prochownik D, Weaver T. Development of the American Association of Diabetes Educators’ Diabetes Self-management Assessment Report Tool. Diabetes Educ. 2007;33:818–26.
Baumann LC, Opio CK, Otim M, Olson L, Ellison S. Self-care beliefs and behaviors in Ugandan adults with type 2 diabetes. Diabetes Educ. 2010;36:293–300.
Cohen J. A power primer. Psychol Bull. 1992;112:155–9.
Alberti H, Boudriga N, Nabli M. Primary care management of diabetes in a low/middle income country: a multi-method, qualitative study of barriers and facilitators to care. BMC Fam Pract. 2007;8:63. doi:10.1186/1471-2296-8-63.
Kalyango JN, Owino E, Nambuya AP. Non-adherence to diabetes treatment at Mulago Hospital in Uganda: prevalence and associated factors. Afr Health Sci. 2008;8:67–73.
Levitt NS. Diabetes in Africa: epidemiology, management and healthcare challenges. Heart. 2008;94:1376–82.
Mbanya JC, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010;375(9733):2254–66.
Leventhal H, Leventhal EA, Breland JY. Cognitive science speaks to the “common-sense” of chronic illness management. Ann Behav Med. 2011;41:152–63.
MacPherson SL, Joseph D, Sullivan E. The benefits of peer support with diabetes. Nurs Forum. 2004;39:5–12.
Heisler M. Different models to mobilize peer support to improve diabetes self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Fam Pract. 2010;27 suppl 1:i23–32. doi:10.1093/fampra/cmp003.
Mbeba MM, Kaponda CP, Jere DL, Kachingwe SI, Crittenden KS, McCreary LL, et al. Peer group intervention reduces personal HIV risk for Malawian health workers. J Nurs Scholarsh. 2011;43:72–81.
Mosaku SK, Kolawol B, Mume C, Ikem R. Depression, anxiety and quality of life among diabetic patients: a comparative study. J Nat Med Assoc. 2008;100:73–8.
Levy J, Jotkowitz AB. Diabetes in Africa: screening for diabetic retinopathy. Eur J Intern Med. 2010;21:145–6.
Conn VS, Algase DL, Rawl SM, Zerwic JJ, Wyman JF. Publishing pilot intervention work. West J Nurs Res. 2010;32:994–1010.
Tang TS, Funnell MM, Gillard M, Nwankwo R, Heisler M. The development of a pilot training program for peer leaders in diabetes: process and content. Diabetes Educ. 2011;37:67–77.
Norris SL, Engelgau MM, Narayan KMV. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–87.
Acknowledgments
This project was supported by a grant from Peers for Progress, a program of the American Academy of Family Physicians Foundation supported by the Eli Lilly Company Foundation. We would like to thank US and Ugandan colleagues who helped to develop and deliver this intervention, especially Dory Blobner, RN, CDE, who provided expert clinical knowledge and experience in diabetes education in developing countries.
Ethical Standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Conflict of Interest
Authors Linda C. Baumann, Nakwagala Frederick, Nankwanga Betty, Ejang Josephine, and Nambuya Agatha declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baumann, L.C., Frederick, N., Betty, N. et al. A Demonstration of Peer Support for Ugandan Adults With Type 2 Diabetes. Int.J. Behav. Med. 22, 374–383 (2015). https://doi.org/10.1007/s12529-014-9412-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-014-9412-8