Abstract
Objective
Patients who need major head and neck surgery like laryngectomy are at risk of postoperative wound infection. Although the role of antibiotics in prophylaxis of clean contaminated head and neck surgery has been well documented, controversy exists in the optimal antibiotic regimen.
Methods
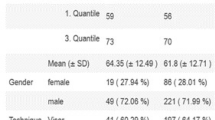
In two tertiary referral hospitals (Imam Khomeini and Amir Alam hospital), 90 patients undergoing laryngectomy were prospectively randomized into two groups receiving cefazolin perioperative prophylaxis either for 2 days or for 5 days from June 2004 to March 2006. Then patients were blindly examined for the development of wound infection.
Results
No wound infection was detected in either group. Two (4.4%) mucocutaneous fistula occurred in the 2-day group, and 3 (6.7%) in the 5-day group. There was no statistically significant difference in the infection rate between two groups.
Conclusion
We conclude that a 2-day perioperative cefazolin prophylaxis is equally effective as longer therapies. The increased morbidity and cost of the latter are in favor of the 2-day prophylactic regimen.
Similar content being viewed by others
References
French RS (2006) The use of prophylactic antibiotics in head and neck oncological surgery. Cur Opin Otol Head Neck Surg 14:55–61
Weber RS, Callender DL (1992) Antibiotic prophylaxis in clean-contaminated head and neck oncologic surgery. Ann Otol Rhinol Laryngol Suppl 155:16–20
Coskun, Levent, Basut, Ogus (2000) Factors affecting wound infection rates in head and neck surgery. Otol Head Neck Surg 123(3):328–333
Penel N, Fournier C, Lefebvre D, et al. (2005) Multivariate analysis of risk factors for wound infection in head and neck squamous cell carcinoma surgery with opening of mucosa. Study of 260 surgical procedures. Oral oncology 41(3): 294–303
Funsconi, Massimo, Andrea, Vitiello, Cecilia, Pagliuca, Giuli (2006) Clean-Contaminated Neck Surgery: Risk of infection by intrinsic and extrinsic factors. Arch Otol — Head and Neck Surgery 132(9):953–957
Johnson JM, Myers, Eugene, Sigler, Barbara (1984) Antimicrobial prophylaxis for contaminated head and neck surgery. Laryngoscope 94(1):46–50
Penel N, Lefebvre D, Fournier C, Sarnia J, Kara A, Lefebvre JL (2001) Risk factors for wound infection in head and neck cancer surgery: a prospective study. Head and Neck 23(6):447–455
Tabet JC JJ (1990) Wound infection in head and neck surgery: prophylaxis, etiology and management. J Otolaryngol 19(3):197–200
Simons JP MJ, Jonas T Yu, Victor L (2001) the role of topical antibiotics in flap reconstruction. The Laryngoscope 111(2):329–335
Blair EA, Johnson JT, Wagner RL, Carrau RL, Bizakis JG (1995) Cost analysis of antibiotic prophylaxis in clean head and neck surgery. Arch Otolaryngol — Head and Neck Surg 121(3):269–271
Callender DL (1999) Antibiotic prophylaxis in head and neck oncologic surgery: the role of gram-negative coverage. Int J Antimicrob Agents 12:21–27
Skitarelic N, Morovic M, Manestar D (2007) Antibiotic prophylaxis in clean-contaminated head and neck oncological surgery. J Craniomaxillofac Surg 35(1):15–20
Rodrigo JP, Alvarez JC, Gomez JR, Suarez C, Fernandez JA, Martinez JA (1997) Comparison of three prophylactic antibiotic regimens in clean-contaminated head and neck surgery. Head Neck 9(3):188–193
Johnson WRL (1987) Infection following uncontaminated head and neck surgery. Arch otolaryngol and head and neck surgery 113(4)
Rebecca Fraioli JT, Johnson (2004) Prevention and treatment of postsurgical head and neck infections. Current Infectious Disease Reports 62 4:172–180
Johnson JT, Schuller DE, Silver F, Gluckman JL, Newman RK, Shagets FW, et al. (1986) Antibiotic prophylaxis in high-risk head and neck surgery: One-day vs. five-day therapy. Otolaryngol Head Neck Surg 95(5):554–557
Johnson JT, Yu VL, Myers EN, Wagner RL (1987) An assessment of the need for gram-negative bacterial coverage in antibiotic prophylaxis for oncological head and neck surgery. J infect disea 155(2):331–333
Mombelli G, Coppens L, Dor P, Klastersky J (1981) Antibiotic prophylaxis in surgery for head and neck cancer. Comparative study of short and prolonged administration of carbenicillin. J Antimicro Chemoth 7(6):665–671
Schwartz Yueh, Bevand (2004) Maynard Predictors of wound complications after laryngectomy: A study of over 2000 patients. Otolaryngol Head and Neck Surg 131(1): 61–68
Ganly I, Patel S, Matsuo J, Singh B, Kraus D, Boyle J, et al. (2005) Postoperative complications of salvage total laryngectomy. Cancer 103(10):2073–2081
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taghy, M., Ashtiani, K., Sadeghi, M. et al. Comparative study of two cefazolin prophylactic protocols in oncologic surgery of the larynx: A randomized trial. Indian J Otolaryngol Head Neck Surg 62, 55–59 (2010). https://doi.org/10.1007/s12070-010-0002-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-010-0002-z