Opinion statement
There are few conditions in neurology that are diagnosed with such ease and certainty as benign paroxysmal positional vertigo (BPPV). Repositioning maneuvers are highly effective in treating BPPV, inexpensive, and easy to apply. Surgery has a very minor role in the management of BPPV, and although medications may transiently ameliorate symptoms, they do not treat the underlying process. There is good evidence to support treatment of posterior canal BPPV with Epley or Semont maneuvers and horizontal canal BPPV with Gufoni maneuvers or BBQ roll (also known as Lempert 360 roll or log roll); and weaker evidence for head hanging maneuvers in the least common anterior canal variant. Since the therapeutic efficacy amongst maneuvers for each canal is comparable, the choice of treatment is generally based on clinician preference, complexity of the maneuvers themselves, poor treatment response to specific maneuvers, and musculoskeletal considerations such as arthritic changes and range of motion of the cervical spine.
-
Treating posterior canal BPPV with Epley or Semont manuevers is comparable as far as efficacy and the ease with which maneuvers are performed.
-
For horizontal canal BPPV, the Gufoni maneuver is easier to perform compared to the BBQ roll, as it requires that the clinician only identify the side of weaker nystagmus (regardless of whether it’s geotropic or apogeotropic) and not necessarily the side involved.
-
Anterior canal BPPV is rare and generally short-lived, but there is weak evidence that deep head hanging and a variety of eponymous maneuvers may hasten recovery. The advantage of deep head hanging maneuvers is that they can be effectively performed without knowledge of the side involved.
Similar content being viewed by others
Introduction
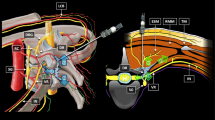
Benign paroxysmal positional vertigo (BPPV) is an exceedingly common disorder of the vestibular system, representing about one-fifth of all referrals to vertigo clinics, with an incidence of 64 per 100,000 population per year [1]. It is more common in women, and prevalence in the elderly population may approach 9 % [2]. Historical features include transient vertigo and oscillopsia (from spontaneous nystagmus) triggered by certain head movements, usually when going from lying to seated, seated to lying, or looking up or down with posterior canal (PC)-BPPV, and rolling over in bed in the case of PC or horizontal canal (HC)-BPPV. Characteristics include a short latency before symptoms occur, fatigability, and habituation. As the name implies: 1) Benign—innocuous disorder that does not result in permanent vestibular dysfunction; 2) Paroxysmal—sudden, short-lived (generally <60 seconds) owing to the mechanical properties of the semicircular canals (SCC angular acceleration detectors), endolymph (fluid contained within the canals, Fig. 1), and otoconia (calcium carbonate crystals normally located on the maculae of the utricle [linear acceleration detectors]) which may slough off spontaneously or as the result of trauma or other processes (Figs. 1 and 2 [3]); 3) Positional—symptoms/signs are dependent on the head movement(s)/gravitational vector(s) that cause movement of any free-floating otoconia and maximally stimulate each SCC; 4) Vertigo—false perception of motion (generally rotation, spinning) as the otoconia (denser than endolymph) move with gravity to the dependent portion of the canal, which causes flow of endolymph, deflection of the cupula, and firing of the vestibular nerve [4] (Fig. 1).
(a)Semicircular canal and structures relevant to BPPV. Endolymph is contained within the canals, and its movement relative to the canal during angular acceleration of the head deflects the cupula. Depending on the direction of movement, either excitation or inhibition of the vestibular hair cells and nerve occurs. (b) When otoconia enter an SCC, they settle in the dependent portion of the canal. (c) Movement of the head/SCC causes the otoconia (more dense than endolymph) to move relative to gravity, inducing endolymph flow. (d) After a brief lag (responsible for BPPV latency), the cupula is deflected, and if deflected in an excitatory direction, results in increased firing of the vestibular nerve.
The labyrinth contains three semicircular canals (anterior, posterior, horizontal), two otoliths (utricle, saccule), and the cochlea (auditory apparatus). Otoconia are normally present within the otoliths. Their dense structure and adherence to the otolithic membrane leads to movement relative to the stereocilia and kinocilium with linear acceleration (horizontal and vertical), which causes inhibition or excitation depending on the direction. When otoconia slough off of the otolithic membrane in the utricle, they are most likely to enter the lowermost, posterior canal, and least likely to enter the uppermost, anterior canal, since the ampulla of the anterior canal lies above the utricle.
Posterior canal BPPV is by far the most common variant, (80-90 % [5]), followed by the horizontal canal (10-31 % [6–8]), and least commonly, the anterior canal (AC; 1-20 % [9–14]) is involved. This discrepancy is most likely due to the orientation of the various canals [15] and how the otoconia may find their way into the respective canals given the influence of gravity and head position (e.g., prolonged head extension during a dental procedure). The PC is the lowermost canal and thus the most commonly affected SCC given the effects of gravity.
Positional maneuvers performed at the bedside illustrate characteristic patterns of nystagmus and symptoms. Familiarity with Ewald’s three laws [16] allows one to localize the side and canal involved based on the nystagmus alone. 1) The vector(s) of nystagmus is within the plane of the canal stimulated (e.g., pure horizontal nystagmus with stimulation of a horizontal canal). 2) Ampullopetal (towards the ampulla) flow of endolymph causes more stimulation than ampullofugal (away from the ampulla) flow in the HC. 3) In the vertical canals (AC and PC), ampullofugal flow is excitatory, and ampullopetal flow inhibitory.
Caution must be paid to a history or examination that is not entirely typical for BPPV, as central positional vertigo may also occur in which the duration of symptoms, pattern of nystagmus, and positions that trigger attacks may vary. Brainstem or cerebellar symptoms or signs may be present, and while attacks will not fulfill all BPPV criteria, they may mimic individual features. Examples include medullary or cerebellar stroke or demyelination, cervicomedullary (e.g., Chiari malformation) or pontomedullary lesion, and cerebellar degeneration (e.g., multiple systems atrophy, spinocerebellar ataxia) [17].
Patients with unrecognized or untreated BPPV may be functionally debilitated, and positional symptoms can lead to phobias and anxiety. Therefore, prompt recognition and treatment can alleviate patient angst, not to mention reduce health care spending on unnecessary testing. The remainder of this article will focus on the diagnosis and treatment of BPPV.
Repositioning maneuvers for posterior canal BPPV
Posterior canal BPPV
There have been several randomized controlled trials (RCT) that have investigated the treatment options for resolving PC-BPPV (Table 1 [7, 18•, 19–23, 24••, 25–27]). Although the study parameters are heterogeneous in frequency of maneuvers and outcome measures utilized, the evidence still clearly shows that treatment of BPPV via repositioning maneuvers is effective. The two most recommended intervention options for resolving PC-BPPV are: 1) Canalith Repositioning Maneuver (CRM), also known as the Epley or Modified Epley Maneuver, and the 2) Liberatory Maneuver, also known as the Semont or Modified Semont Maneuver. These have been shown to be equally effective [28].
Diagnosis
-
1)
Dix-Hallpike test
The patient is placed on an exam table or bed in the long-sitting position. To test the right PC, the head is rotated 45 degrees to the right, and the patient is lowered into a supine position with the head extended 30 degrees beyond earth horizontal. This position moves the right PC into a plane aligned with the gravitational vector, which induces movement of otoconial debris through the posterior canal and causes excitation (ampullofugal direction of endolymph flow). This position is held for at least 30 seconds to allow for a potential latency in the onset of nystagmus, as there is characteristically a lag between the movement of otoconial debris and deflection of the cupula (Fig. 1). The patient is then asked to report symptoms of vertigo, dizziness, or perhaps falling. Upbeat-torsional nystagmus is seen with PC-BPPV, where the torsional component beats towards the lowermost ear or clockwise from the patient’s perspective (rightward in right PC-BPPV). This is because stimulation of the right PC leads to conjugate (i.e., equal movement in each eye in a direction determined by Ewald’s first law) downward and counterclockwise (from the patient’s perspective; towards the left ear with right PC-BPPV) torsional drift of the eyes. This is followed by a position reset mechanism (fast or named phase of nystagmus) that is upbeating and torsional (towards the right ear). This procedure is reversed when assessing for left PC-BPPV. (Table 2) Cupulolithiasis (otoconia attached to the cupula) of the PC occurs rarely, and a weaker (compared with canalolithiasis) nystagmus persists for as long as the head is positioned, given the effects of gravity.
Table 2 Characteristic nystagmus for each canal assuming right-sided canalithiasis BPPV and appropriate test position (Dix Hallpike vs Roll) -
2)
Sidelying Dix-Hallpike test:
For those patients unable to tolerate supine positioning or the 30 degrees of neck extension required for the Dix-Hallpike test, the sidelying Dix-Hallpike test can be done instead [29]. The head is first rotated 45 degrees towards one side, and the patient lies down on the opposite shoulder. The head should be positioned towards the sky (from the original 45-degree rotation), and the ear towards the ground is the ear being tested. Interpretation of nystagmus is the same as for the traditional Dix-Hallpike test.
Treatment
-
1)
Canalith Repositioning Maneuver or Modified Epley Maneuver (Fig. 3):
Figure 3 CRP. For right PC-BPPV: (a) The patient begins in the long-sitting position; (b) the head is rotated 45 degrees to the right, and (c) then the patient is lowered into the supine position where the head is in 30 degrees of cervical extension. In this position, nystagmus is identified and symptoms are noted. Once nystagmus has resolved and symptoms are such that the patient can tolerate the next position, (d) the patient’s head is rotated 90 degrees, from 45 degrees of rotation to the right to 45 degrees of rotation to the left. (e) The patient is rolled into a left-side lying position, and the head is maintained in 45 degrees of rotation to the left, so that the head is facing the floor. This position is held for up to one minute or until resolution of nystagmus and symptoms. (f) The patient sits up slowly with the head still facing down towards the floor and rotated 45 degrees to the left and (g) then slowly moved back to neutral.
For the right posterior canal, the patient is positioned identically as for the Dix-Hallpike test, in the long-sitting position. (a) With the head rotated 45 degrees to the right, the patient is lowered into (b) the supine position, and the head is lowered to 30 degrees of cervical extension. In this position, nystagmus is identified and symptoms are noted. Once nystagmus has resolved and symptoms are such that the patient can tolerate the next position, (c) the patient’s head is rotated 90 degrees, from 45 degrees of rotation to the right to 45 degrees of rotation to the left. (d) The third position involves the patient rolling into a left side-lying position. The patient’s head is maintained in 45 degrees of rotation to the left, so that the head is facing the floor. This position is held for up to one minute or until resolution of nystagmus and symptoms. (e) The patient sits up slowly with the head still facing down towards the floor and rotated 45 degrees to the left. Care must be taken when the patient initially sits up, as the patient may experience postural instability and increased dizziness.
-
2)
Liberatory or Modified Semont Maneuver (Fig. 4)
Figure 4 Semont. For right PC-BPPV: (a) The patient sits at the edge of the table, and (b) the head is turned 45 degrees to the left. (c) The patient is quickly brought into a right side-lying position, and this position is maintained for 1 minute. (d) The patient is then guided quickly from right to left side-lying positions within 1.5 seconds, without stopping in the center. The head should be maintained in the initial 45 degrees of leftward rotation, so that at the end of the maneuver the patient is facing the table/ground. This position is maintained for 1 minute. (e) The patient is then guided into a seated position slowly, with the head maintained in 45 degrees of leftward rotation and (f) slowly moved back to neutral.
For a right posterior canal maneuver, the patient sits at the edge of the table, and (a) the head is turned 45 degrees to the left. (b) The patient is quickly brought into a right side-lying position, which is maintained for 1 minute. (c) The patient is then guided quickly from right to left side-lying within 1.5 seconds, without stopping in the center. The head should be maintained in the initial 45 degrees of leftward rotation so that at the end of the maneuver, the patient is facing the table/ground. This position is maintained for 1 minute. (d) The patient is then guided into a seated position slowly, with the head maintained in 45 degrees of leftward rotation.
-
3)
Brandt-Daroff Exercises
Brandt-Daroff exercises were developed prior to repositioning maneuvers for treatment of PC-BPPV [30]. These exercises were subsequently found to be less effective than repositioning maneuvers, but were still used following repositioning to prevent recurrence [31•]. However, Helminski et al. found that the rate of recurrence and time to recurrence were not improved with daily performance of Brandt-Daroff exercises following canalith repositioning treatments [32]. The exercises are still beneficial for the management of phobic responses to lying supine or side-lying after resolution of BPPV. The patient begins in a seated position, and then moves to a side-lying position with the head angled upward by 45 degrees. This position is held for 30 seconds or until dizziness subsides, then back to the seated position. The side-lying position is then initiated in the opposite direction and maintained in the same way before moving back to the seated position.
Alternatives to the Brandt Daroff exercises involving the patient performing the modified Epley or modified Semont maneuvers at home have been developed and studied for their effectiveness. Radke et al. reported an effectiveness of 95 % with the modified Epley maneuver and 58 % with the modified Semont maneuver, with both having similar treatment side effects [33]. The modified Epley maneuver for home use was found to be more effective than Brandt-Daroff exercises [34]. However, without adequate patient education, there is a risk of canal conversion (e.g., causing HC-BPPV) or ineffectiveness of the self-administered treatment [34].
Repositioning maneuvers for horizontal canal BPPV
Horizontal canal BPPV
There have been several RCTs that have investigated the treatment options for resolving HC-BPPV (Table 1 [7, 35••, 36••, 37••]). HC-BPPV causes a horizontal nystagmus, regardless of side-lying position, which may lead to confusion regarding the side involved. As is the case for the vertical SCCs, two types of HC-BPPV are possible, canalolithiasis or cupulolithiasis. This distinction is most relevant for HC-BPPV, and is made by observing the direction and duration of nystagmus.
If the nystagmus seen with HC-BPPV beats towards the lowermost ear (towards earth) in the side-lying position, it is called geotropic nystagmus [38, 39]. This is thought to be the result of ampullopetal flow of otoconial debris within the endolymph of the canal, i.e., canalolithiasis [39, 40]. In contrast, apogeotropic nystagmus is the termed used when the fast phase beats towards the uppermost ear (away from earth) [41–43], and is the result of otoconial debris that is either adherent to the cupula (i.e., cupulolithiasis), or free-floating but located in the anterior arm of the HC near the cupula (technically still canalolithiasis) [44, Class II].
Diagnosis
-
Geotropic nystagmus
Based on Ewald’s 2nd law, ampullopetal (towards the ampulla) endolymph flow is more excitatory as compared with ampullofugal (away from the ampulla) flow [16]. Therefore, when otoconial debris is present in the right HC (middle or posterior arms), turning the head to the right while the patient is supine results in ampullopetal flow, excitation, and right-beating (geotropic) nystagmus (slow [pathologic via right excitation] phase to the left, fast, position reset phase to the right). If the head is then turned to the left, the same otoconial debris induces ampullofugal flow in the right HC and inhibition, causing a left-beating (still geotropic) nystagmus (slow [pathologic via right inhibition] phase to the right and fast, position reset phase to the left). The nystagmus is generally <60 seconds, and of greater velocity with ampullopetal endolymph flow (e.g., geotropic nystagmus is more intense with head rotation to the right in right HC-BPPV). Simply put, geotropic nystagmus will be more intense towards the affected ear.
-
Apogeotropic nystagmus
If the otoconia are adherent to the cupula of the HC, nystagmus will be apogeotropic. The nystagmus will beat away from the earth regardless of right or left head position when supine. In cupulolithiasis, the otoconia weigh down the cupula and cause it to deflect towards or away from the utricle depending on the direction of head movement. For example, when the head is rolled to the right, otoconia stuck to the cupula of the right HC will deflect the cupula away from the utricle (ampullofugal - inhibitory) causing left-beating (apogeotropic) nystagmus (slow [pathologic via right inhibition] phase to the right and fast, position reset phase to the left). When the head is rolled to the left, otoconia stuck to the cupula of the right HC will deflect the cupula away from the utricle (ampullopetal - excitatory) causing right-beating (apogeotropic) nystagmus (slow [pathologic via right excitation] phase to the left and fast, position reset phase to the right). The nystagmus is generally >60 seconds, and of greater velocity with ampullofugal endolymph flow (e.g., apogeotropic nystagmus is more intense with head rotation to the left in right HC-BPPV). Simply put, apogeotropic nystagmus will be more intense towards the unaffected ear. It is also possible to have apogeotropic nystagmus <60 seconds in duration due to otoconial debris moving in the ampullofugal direction within the anterior arm of the HC.
-
1)
Supine roll test
Various clinical tests can be used to test for HC-BPPV and determine the affected ear. The most commonly used test is the supine roll test [39]. This test is also known as the Pagnini-McClure test [38]. The supine roll test places the patient supine with the head flexed 30° to bring the HC in alignment with the gravitational vector. Next the head is turned to one side and then the other as the clinician notes nystagmus and vertigo. To prevent neck injury, the patient may move his or her own head in rotation.
-
2)
Bow and Lean test
The Bow and Lean test is mainly used to help lateralize the affected HC, and is best used in conjunction with or after the supine roll test has been performed [45, Class III]. Pitching the head down 60 degrees (bow) or up 30 degrees (lean) will enable cupular deflection if otoconia are displaced in the HC. A downward pitch of the head will allow any free-floating otoconia (canalolithiasis) to move towards the cupula (ampullopetal) and cause nystagmus that will beat towards the affected ear. For example, canalolithiasis of the right HC will cause a right-beating nystagmus (slow [pathologic via right excitation] phase to the left and fast, position reset phase to the right) in the bow head position. An upward pitch of the head (lean) will cause any freely floating otoconia to move away from the cupula (ampullofugal) and cause an inhibitory nystagmus (e.g., left-beating nystagmus in right HC-BPPV). In cupulolithiasis, a head bow may create nystagmus that beats away from the affected ear, where a head lean may cause nystagmus to beat towards the affected ear. There typically exists a “null point” where the nystagmus will extinguish because the cupula is in a gravity-neutral position.
-
1)
Treatment
-
1)
BBQ Roll (Fig. 5)
Figure 5 BBQ. For right HC-BPPV: (a) The patient begins in the long-sitting position, and (b) is then placed in a supine position with the head elevated 30 degrees. (c) Next, the patient’s head (or whole body) should be rotated 90 degrees to the right side and maintained for 30 seconds or until the nystagmus and vertigo cease. (d) From this position, the head is rotated back to neutral, then (e) 90 degrees to the left side, (f) into the prone position, (g) 90 degrees to the right side, and finally (h) back into the long-sitting position. Each of these positions is maintained for 30 seconds or until the nystagmus and vertigo cease.
This maneuver has the subject roll away from the affected side in 90 degree increments. (a) First, the patient is placed in a supine position with the head elevated 30 degrees. (b) Next, the patient’s head (or whole body) should be rotated 90 degrees to the affected side and maintained for 30 seconds or until the nystagmus and vertigo cease. (c) From this position, the head is rotated back to neutral, then (d) 90 degrees to the unaffected side, and then (e) into the prone position. Each of these positions is maintained for 30 seconds or until the nystagmus and vertigo cease. This maneuver has been shown to be more effective than sham based on a Level I classification study [35••]. (Table 1)
-
2)
Gufoni Maneuver (Fig. 6)
Figure 6 Gufoni. For right apogeotropic HC-BPPV or left geotropic HC-BPPV: (a) From a seated position, (b) the subject is asked to quickly lie to the unaffected side (side of weaker nystagmus – e.g., to the right in right apogeotropic or left geotropic HC-BPPV). This position, where the head is not rotated but remains in a neutral spine orientation, is held for 2 minutes. (c) After 2 minutes, the patient moves the head 45 degrees towards the ceiling and holds another 2 minutes, and (d) then returns back up to a seated position.
This maneuver is done from a seated position. (a) The subject is asked to quickly lie to the unaffected side with geotropic (e.g., to the left in right geotropic HC-BPPV), or to the affected side with apogeotropic HC-BPPV (e.g., to the right in right apogeotropic HC-BPPV). Or, the examiner need only remember that the initial position is to the side of weakest nystagmus. This position, where the head is not rotated but remains in a neutral spine orientation, is held for 2 minutes. (b) After 2 minutes, the patient moves the head 45 degrees down for the geotropic variant or head 45 degrees up for the apogeotropic variant, and this position is maintained for another 2 minutes. This maneuver has been shown to be more effective than sham based on three Level I classification studies [36••, 37••]. (Table 1)
Unfortunately, in the case of persistent cupulolithiasis of the HC, we cannot know for certain whether the otoconia are adherent to the utricular or canal side of the cupula. In either case, deflection of the cupula during testing and treatment would be similar. Therefore, we recommend that clinicians modify the repositioning maneuvers accordingly. For example, applying a Gufoni maneuver for treating a cupulolithiasis affecting the right HC might instead have the subject lie on the unaffected side, presuming the otoconia are attached to the utricular side of the cupula.
Repositioning maneuvers for anterior canal BPPV
Anterior canal BPPV is the least common variant, as the location of the AC on top of the vestibule makes it unlikely that otoconial debris enter either end of the canal against gravity unless the head is brought upside down. Thus, AC-BPPV is often the result of canal switch in the course of treating other canal variants. For the same reason, canalolithiasis involving the posterior arm of the AC can be short-lived, as the effect of gravity in the upright head position pulls the debris back to the vestibule. In the head down position, the movement of otoconial debris will be in the same direction with the anterior arm of the AC for both cupulolithiasis and canalolithiasis [46].
Diagnosis
According to Ewald’s 3rd law, ampullofugal flow is excitatory and ampullopetal inhibitory within the AC and PC. Downbeat-torsional nystagmus is seen with AC-BPPV, where the torsional component beats towards the lowermost ear, or clockwise from the patient’s perspective (rightward in right AC-BPPV). This is because stimulation of the right AC leads to conjugate (i.e., equal movement in each eye in a direction determined by Ewald’s first law) upward and counterclockwise (from the patient’s perspective; towards the left ear with right AC-BPPV) torsional drift of the eyes. (Table 2). This is followed by a position-reset mechanism (fast, or named phase, of nystagmus) that is downbeat-torsional (towards the right ear). The patients are also asked to report any symptoms of vertigo, dizziness, or perhaps falling.
Since each AC is coplanar to the PC on the opposite side, the nystagmus in AC-BPPV is seen with the Dix-Hallpike maneuver on the opposite side (e.g., right AC-BPPV diagnosed with left Dix-Hallpike). In practice, however, the nystagmus may be triggered by the Dix-Hallpike maneuver on either side or by straight head hanging, showing low specificity for detecting the side involved in AC-BPPV. This finding has been attributed to the upright orientation of the ampullary segment of the anterior SCCs, making the excitation of the canal possible irrespective of the direction of the head rotation during the Dix-Hallpike maneuver [47]. Thus, in order to trigger AC-BPPV, the head rotation in the canal plane appears to be less relevant than a final head down position. The nystagmus in AC-BPPV is fatigable, but tends to be long-lasting and of low intensity (especially the torsional component) [47, 48]. Furthermore, in contrast to PC-BPPV, it often does not reverse direction on return to upright position at the end of the Dix-Hallpike maneuver [48]. Positional downbeat nystagmus is also sometimes a feature of central dysfunction, and such etiologies should be excluded [49].
Treatments
The proposed treatments for AC-BPPV are mostly based on non-controlled studies [9, 10, 50, 51•, 52•, 53].
-
1)
‘Reverse Epley’ or ‘reverse Semont’ maneuvers have been suggested, but there are no studies regarding their efficacy [9].
-
2)
In a CRP described by Rahko, 53 of 57 patients were reported as symptom-free after treatment [50]. In this maneuver, (a) the patient first laid on the healthy side. (b) The head was brought down 45 degrees, then (c) back to horizontal and (d) finally upwards 45°, each for 30 seconds. (e) The patient then sat up for 3 minutes while supported.
-
3)
Kim et al. proposed another method and reported efficacy of 96.7 % in 30 patients [51•]. In their maneuver, (a) the head was first turned 45° towards the unaffected side.(b) The patient was then brought down to lay supine with the head hanging 30° below the end of the examination table. (c) After about 2 minutes, the head was brought up to supine position, and (d) then in one minute, the patient was brought back to sit upright with the chin tilted down about 30°.
-
4)
Yacovino et al. described a ‘deep head hanging’ maneuver (Fig. 7) [52•], which was similar to but shorter than the “prolonged forced position procedure” proposed by Crevits [10] for treatment of refractory AC-BPPV. The advantage of the deep head hanging maneuver is that it can be done properly without knowledge of the side affected. It consists of three steps with four position changes at intervals of about 30 seconds: (a) the head is first brought to at least 30° below the horizontal from a sitting position with the head straight up. This step is similar to the straight deep head hanging often used to provoke nystagmus in AC-BPPV. Once the nystagmus induced by this step is over, (b) the head is brought up quickly to touch the chest while the patient is still supine. As the final step, (c) the patient is brought back to sit up with the head straight.
Figure 7 Deep head hanging (a) The patient is in the long-sitting position, and (b) the head is first brought to at least 30° below the horizontal with the head straight up. Once the nystagmus induced by this step is over, (c) the head is brought up quickly to touch the chest while the patient is still supine, and after 30 seconds (d) the patient is brought back to a seated position with head flexion maintained. (e) The patient is brought back to a neutral head position.
For all BPPV variants
Contraindications
-
Clinicians treating patients for BPPV must consider the following pre-existing conditions: occipitoatlantal or atlantoaxial instability, cervical myelopathy or radiculopathy, severe carotid stenosis, orthopnea, or unstable cardiac condition.
-
In the case of orthopedic limitations (mainly cervical), because the maneuvers only utilize gravitational force to move the otoconia through the canals, the only real requirement is that the head is in the correct plane. Therefore, rolling the patient instead of rotating the cervical spine may be used to achieve 45 degrees of cervical rotation. Pillows or a wedge under the thoracic spine, or a reverse tilt table may be used as ways to modify the maneuver in order to achieve 30 degrees of cervical extension.
Complications
-
Due to the repetitive position changes that must be endured when testing and treating with canalith repositioning maneuvers (especially the higher velocity Semont Maneuver), caution should be taken when delivering the treatments, particularly in those with comorbidities (see contraindications).
-
In approximately 6 % of cases, posterior canal BPPV converts to horizontal or anterior canal BPPV [23].
-
The process of testing and/or treating BPPV involves vestibular stimulation that can induce nausea and vomiting. Medications such as prochlorperazine, promethazine, ondansetron, or benzodiazepines may be used to mitigate these symptoms. Alternatively, if medications are not readily available or desired, cooling the patient with ice packs on the cervical spine and trunk can help to raise the nausea threshold.
-
Vestibular stimulation can also induce significant anxiety and panic, which is often managed with encouragement, but may also be ameliorated with medication if warranted (e.g., anxiolytics).
-
Strong vestibular stimulation has been found to trigger migraines, so care must be taken when treating those with active migraines [54].
Cost/cost effectiveness
The repositioning maneuvers are highly cost effective, as they are relatively simple procedures that can resolve debilitating symptoms. The procedure is performed during an office visit and requires no equipment other than an exam table and, optimally, a mechanism to inhibit visual fixation.
Special notes
How can I best visualize and interpret nystagmus?
Frenzel goggles or video-oculography are preferred for assessment and treatment to improve identification of the direction of nystagmus and to monitor the response to treatment while performing the repositioning maneuvers. When the patient is able to fixate, there may be suppression of the horizontal or vertical component, so that the torsional component is most prominent (humans have a poor torsional suppression mechanism). With fixation removed (e.g., Frenzel goggles or video-oculography), all components of the nystagmus are better appreciated.
How much treatment is enough?
Original recommendations by Epley were that the CRMs be repeated as many times as necessary in one treatment session in order to achieve a negative Dix-Hallpike, until the patient can no longer tolerate the maneuvers, or until there is no improvement made in the last two maneuvers [55]. In a subsequent study by Gordon, et al. repeated maneuvers in one session were also found to be superior to one maneuver [56]. Reassessment of the success of repositioning maneuvers and subsequent treatment if not resolved should be no more often than every 48 hours [57].
What instructions should I give post-CRM?
Historically, post-maneuver instructions were given to patients in order to maximize the effectiveness of treatment. These included not lying on the affected side for a week, sleeping in a sitting position for 48 hours, and wearing a cervical collar to limit head movement [22]. These instructions can be difficult for the patient to follow and result in poor sleep. Post-treatment instructions have been investigated to determine their necessity for both the Epley and Semont maneuvers [58, Class IV; 59, Class III]. Outcomes, as determined by repeat Dix-Hallpike tests and symptoms, were similar with or without post-maneuver instructions. The instructions are, therefore, no longer recommended [58, 59]. Because it has been shown that postural stability may be affected by CRMs, instructing the patient to be cautious in the ensuing 24 hours is recommended [60].
What about intractable cases of BPPV?
According to an epidemiologic study of 2,270 patients, 1.7 % had intractable BPPV that could not be resolved with repositioning maneuvers [5]. There are no clear guidelines for abandoning repositioning as a treatment modality. Generally, if the patient does not respond within 4 visits, one should consider alternative diagnoses (e.g., central vestibular disorder). Alternate explanations for recalcitrant BPPV may be the patient’s SCC morphology, difficulties achieving optimal positioning during maneuvers (e.g., cervical spine disease), or perhaps an anomaly in the anatomical alignment of the canals. Comorbidities such as migraine or Meniere’s disease may also play a role in resolution of BPPV [61, 62]. Traumatic origin of BPPV has been implicated in a prolonged recovery and multiple canal involvement [63, 64]. For those with intractable BPPV, surgical occlusion of the canal is a viable option for management [65, 66].
Surgery
Semicircular canal plugging/occlusion and singular neurectomy
CRPs done repeatedly and properly almost always obviate the need for surgical intervention.
However, singular neurectomy may be effective in some refractory patients, but carries a risk of sensorineural hearing loss [67, 68]. Section of the nerve (branch of vestibulocochlear nerve that innervates the PC) is confirmed during surgery when down-beat nystagmus is seen as the result of transient ipsilateral PC hypofunction (nerve to PC lesioned during surgery) and relative ipsilateral AC hyperfunction (i.e., slow pathologic upward phase and fast corrective downward phases). Surgery is performed through the external auditory canal.
Plugging or occlusion of the PC has a low risk of sensorineural hearing loss and has also been shown to be effective in treating refractory BPPV [65, 66, 69–72], but a mastoidectomy and general anesthesia is required, making it more invasive. The rationale is that by plugging the involved canal, there is no longer an endolymphatic current flow induced by debris. One retrospective review found that vestibular symptoms (persistent or new, generally BPPV in other canals) were common following surgery despite resolution of BPPV in the treated canal [73]. Evidence for efficacy of these procedures is limited to case reports and series.
Assistive devices
Oscillators
Performing mastoid vibration during CRPs was proposed as a means of augmenting the efficacy of the maneuvers in refractory cases [74]. Subsequent to this report, it has repeatedly been shown to be no more effective than CRPs performed without vibration [75, 76]. In an experimental frog model, vibration was found to be an effective stimulus for treating cupulolithiasis [77]; however, more work is necessary to determine its utility in human subjects.
Conclusions
The vast majority of patients with complaints of positional vertigo will, in fact, have benign paroxysmal positional vertigo. The characteristic history guides the examination, and the Dix-Hallpike maneuver (to diagnose PC or AC-BPPV) is obligatory in this population. If negative, supine roll testing (to diagnose HC-BPPV) should also be performed. Knowledge of the orientation and physiological features of the SCCs allows for accurate diagnosis of the side and canal affected, and the specific therapeutic maneuvers detailed above are then applied. The maneuvers are cost-effective, require little to no equipment, are relatively easy to perform, and highly efficacious. Thus, successful treatment of BPPV can be a highly satisfying experience for both the patient and clinician alike.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Froehling DA, Silverstein MD, Mohr DN, et al. Benign positional vertigo: incidence and prognosis in a population-based study in Olmsted County, Minnesota. Mayo Clin Proc. 1991;66:596–601.
von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78:710–5.
Fife TD, Iverson DJ, Lempert T, et al. Practice parameter: therapies for benign paroxysmal positional vertigo (an evidence-based review). Neurology. 2008;70:2067–74.
Parnes LS, McClure JA. Free-floating endolymph particles: a new operative finding during posterior semicircular canal occlusion. Laryngoscope. 1992;102:988–92.
Caruso G, Nuti D. Epidemiological data from 2270 BPPV patients. Audiol Med. 2005;3:7–11.
De la Meilleure G, Dehaene I, Depondt M, et al. Benign paroxysmal positional vertigo of the horizontal canal. J Neurol Neurosurg Psychiatry. 1996;60:68–71.
Prokopakis EP, Chimona T, Tsagournisakis M, et al. Benign paroxysmal positional vertigo: 10-year experience in treating 592 patients with canalith repositioning procedure. Laryngoscope. 2005;115:1667–71.
Moon SY, Kim JS, Kim BK, et al. Clinical characteristics of benign paroxysmal positional vertigo in Korea: a multicenter study. J Korean Med Sci. 2006;21:539–43.
Honrubia V, Baloh RW, Harris MR, Jacobson KM. Paroxysmal positional vertigo syndrome. Am J Otol. 1999;20:465–70.
Crevits L. Treatment of anterior canal benign paroxysmal positional vertigo by a prolonged forced position procedure. J Neurol Neurosurg Psychiatry. 2004;75:779–81.
Korres S, Balatsouras DG, Kaberos A, et al. Occurrence of semicircular canal involvement in benign paroxysmal positional vertigo. Otol Neurotol. 2002;23:926–32.
Schratzenstaller B, Wagner-Manslau C, Strasser G, Arnold W. Canalolithiasis of the superior semicircular canal: an anomaly in benign paroxysmal vertigo. Acta Otolaryngol. 2005;125:1055–62.
Jackson LE, Morgan B, Fletcher JC, Krueger WW. Anterior canal benign paroxysmal positional vertigo: an underappreciated entity. Otol Neurotol. 2007;28:218–22.
Soto-Varela A, Santos-Perez S, Rossi-Izquierdo M, Sanchez-Sellero I. Are the three canals equally susceptible to benign paroxysmal positional vertigo? Audiol Neurotol. 2013;18:327–34.
Bradshaw AP, Curthoys IS, Todd MJ, et al. A mathematical model of human semicircular canal geometry: a new basis for interpreting vestibular physiology. J Assoc Res Otolaryngol. 2010;11:145–59.
Ewald JR. Physiologische Untersuchungen ueber das Endorgan des Nervus Octavus. Bergmann; 1892. p. 324.
Fife TD. Positional dizziness. Continuum. 2012;18:1060–85.
Asawavichianginda S, Isipradit P, Snidvongs K, Supiyaphun P. Canalith repositioning for benign paroxysmal positional vertigo: a randomized, controlled trial. Ear Nose Throat J. 2000;79:732–4. 736–7. A randomized-controlled trial for the modified Epley maneuver for posterior canal BPPV with 2 week follow-up.
Blakley B. A randomized, controlled assessment of the canalith repositioning maneuver. Otolaryngol Neck Surg. 1994;110:391–6.
Chang AK, Schoeman G, Hill M. A randomized clinical trial to assess the efficacy of the Epley maneuver in the treatment of acute benign positional vertigo. Acad Emerg Med. 2004;11:918–24.
Chen Y, Zhuang J, Zhang L, et al. Short-term efficacy of Semont maneuver for benign paroxysmal positional vertigo: a double-blind randomized trial. Otol Neurotol. 2012;33:1127–30.
Lynn S, Rose O, Brey R, Suman V. Randomized trial of the canalith repositioning procedure. Otolaryngol Head Neck Surg. 1995;113:712–20.
Yimtae K, Srirompotong S, Srirompotong S, Sae-Seaw P. A randomized trial of the canalith repositioning procedure. Laryngoscope. 2003;113:828–32.
Mandalà M, Santoro GP, Asprella Libonati G, et al. Double-blind randomized trial on short-term efficacy of the Semont maneuver for the treatment of posterior canal benign paroxysmal positional vertigo. J Neurol. 2012;259:882–5. A randomized-controlled trial for the Semont maneuver showing efficacy.
Munoz JE, Miklea JT, Howard M, et al. Canalith repositioning maneuver for benign paroxysmal positional vertigo: randomized controlled trial in family practice. Can Fam Physician. 2007;53:1049–53.
Simhadri S, Panda N, Raghunathan M. Efficacy of particle repositioning maneuver in BPPV: a prospective study. Am J Otolaryngol. 2003;24:355–60.
von Brevern M, Seelig T, Radtke A, et al. Short-term efficacy of Epley’s manoeuvre: a double-blind randomised trial. J Neurol Neurosurg Psychiatry. 2006;77:980–2.
Herdman SJ, Tusa RJ, Zee DS, et al. Single treatment approaches to benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg. 1993;119:450–4.
Cohen HS. Side-lying as an alternative to the Dix-Hallpike test of the posterior canal. Otol Neurotol. 2004;25:130–4.
Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg. 1980;106:484–5.
Amor-Dorado JC, Barreira-Fernández MP, Aran-Gonzalez I, et al. Particle repositioning maneuver versus Brandt-Daroff exercise for treatment of unilateral idiopathic BPPV of the posterior semicircular canal: a randomized prospective clinical trial with short- and long-term outcome. Otol Neurotol. 2012;33:1401–7.This paper shows that CRM is more effective than Brandt-Daroff exercises
Helminski JO, Kotaspouikis D, Kovacs K, et al. Strategies to prevent recurrence of benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg. 2005;131:344–8.
Radtke A, von Brevern M, Tiel-Wilck K, et al. Self-treatment of benign paroxysmal positional vertigo: Semont maneuver vs Epley procedure. Neurology. 2004;63:150–2.
Radtke A, Neuhauser H, von Brevern M, Lempert T. A modified Epley’s procedure for self-treatment of benign paroxysmal positional vertigo. Neurology. 1999;53:1358–60.
Kim JS, Oh S-Y, Lee S-H, et al. Randomized clinical trial for geotropic horizontal canal benign paroxysmal positional vertigo. Neurology. 2012;79:700–7. This is a randomized, controlled trial that showed that there was no difference in effectiveness between the BBQ roll and Gufoni maneuvers for geotropic HC-BPPV.
Kim JJ-S, Oh S-YS, Lee S-HS, et al. Randomized clinical trial for apogeotropic horizontal canal benign paroxysmal positional vertigo. Neurology. 2012;78:159–66. This is a randomized, controlled trial that showed the effectiveness of Gufoni maneuvers for apogeotropic HC-BPPV.
Mandalà M, Pepponi E, Santoro GP, et al. Double-blind randomized trial on the efficacy of the Gufoni maneuver for treatment of lateral canal BPPV. Laryngoscope. 2013;123:1782–6. This paper is the most recent randomized, controlled trial that determined that the Gufoni maneuver is effective for horizontal canal BPPV.
McClure JA. Horizontal canal BPPV. J Otolaryngol. 1985;14:30–5.
Baloh RW, Jacobson K, Honrubia V. Horizontal semicircular canal variant of benign positional vertigo. Neurology. 1993;43:2542–9.
Lempert T. Horizontal benign positional vertigo. Neurology. 1994;44:2213–4.
Baloh RW, Yue Q, Jacobson KM, Honrubia V. Persistent direction-changing positional nystagmus: another variant of benign positional nystagmus? Neurology. 1995;45:1297–301.
Casani A, Giovanni V, Bruno F, Luigi GP. Positional vertigo and ageotropic bidirectional nystagmus. Laryngoscope. 1997;107:807–13.
Fife TD. Recognition and management of horizontal canal benign positional vertigo. Am J Otol. 1998;19:345–51.
Nuti D, Vannucchi P, Pagnini P. Benign paroxysmal positional vertigo of the horizontal canal: a form of canalolithiasis with variable clinical features. J Vestib Res. 1998;6:173–84.
Choung Y-H, Shin YR, Kahng H, et al. “Bow and lean test” to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. 2006;116:1776–81.
Büki B. Benign paroxysmal positional vertigo–toward new definitions. Otol Neurotol. 2014;35:323–8.
Bertholon P, Bronstein AM, Davies RA, et al. Positional down beating nystagmus in 50 patients: cerebellar disorders and possible anterior semicircular canalithiasis. J Neurol Neurosurg Psychiatry. 2002;72:366–72.
Cambi J, Astore S, Mandalà M, et al. Natural course of positional down-beating nystagmus of peripheral origin. J Neurol. 2013;260:1489–96.
Kheradmand A, Zee DS. Cerebellum and ocular motor control. Front Neurol. 2011;2:53.
Rahko T. The test and treatment methods of benign paroxysmal positional vertigo and an addition to the management of vertigo due to the superior vestibular canal (BPPV-SC). Clin Otolaryngol Allied Sci. 2002;27:392–5.
Kim YK, Shin JE, Chung JW. The effect of canalith repositioning for anterior semicircular canal canalithiasis. ORL J Otorhinolaryngol Relat Spec. 2005;67:56–60. This article describes a canalith repositioning mauever for anterior semicircular canal BPPV.
Yacovino DA, Hain TC, Gualtieri F. New therapeutic maneuver for anterior canal benign paroxysmal positional vertigo. J Neurol. 2009;256:1851–5. This article describes a canalith repositioning mauever for anterior semicircular canal BPPV.
Korres S, Riga M, Sandris V, et al. Canalithiasis of the anterior semicircular canal (ASC): treatment options based on the possible underlying pathogenetic mechanisms. Int J Audiol. 2010;49:606–12.
Murdin L, Davies RA, Bronstein AM. Vertigo as a migraine trigger. Neurology. 2009;73:638–42.
Epley JM. Positional vertigo related to semicircular canalithiasis. Otolaryngol Head Neck Surg. 1995;112:154–61.
Gordon CRGN. Repeated vs single physical maneuver in benign paroxysmal positional vertigo. Acta Neurol Scand. 2004;110:166–9.
Epley JM. Particle repositioning for benign paroxysmal positional vertigo. Otolaryngol Clin N Am. 1996;29:323–31.
Massoud EA, Ireland DJ. Post-treatment instructions in the nonsurgical management of benign paroxysmal positional vertigo. J Otolaryngol. 1996;25:121–5.
Nuti D, Nati C, Passali D. Treatment of benign paroxysmal positional vertigo: no need for postmaneuver restrictions. Otolaryngol Head Neck Surg. 2000;122:440–4.
Blatt PJ, Georgakakis GA, Herdman SJ, et al. The effect of the canalith repositioning maneuver on resolving postural instability in patients with benign paroxysmal positional vertigo. Am J Otol. 2000;21:356–63.
Gross EM, Viirre ES, Nelson JR, Harris JP. Intractable benign paroxysmal positional vertigo in patients with Meniere’s disease. Laryngoscope. 2000;110:655–9.
Ishiyama Jacobsom K, Baloh R. Migraine and benign positional vertigo. Ann Otol Rhinol Larynology. 2000;190:377–80.
Katsarkas A. Benign paroxysmal positional vertigo (BPPV): idiopathic versus post-traumatic. Acta Otolaryngol. 1999;119:745–9.
Gordon CR, Levite R, Joffe V, Gadoth N. Is posttraumatic benign paroxysmal positional vertigo different from the idiopathic form? Arch Neurol. 2004;61:1590–3.
Shaia WT, Zappia JJ, Bojrab DI, et al. Success of posterior semicircular canal occlusion and application of the dizziness handicap inventory. Otolaryngol Head Neck Surg. 2006;134:424–30.
Ahmed RM, Pohl D, MacDougall HG, et al. Posterior semicircular canal occlusion for intractable benign positional vertigo: outcome in 55 ears in 53 patients operated upon over 20 years. J Laryngol Otol. 2012;126:677–82.
Pournaras I, Kos I, Guyot JP. Benign paroxysmal positional vertigo: a series of eight singular neurectomies. Acta Otolaryngol. 2008;128:5–8.
Gacek RR. Transection of the posterior ampullary nerve for the relief of benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1974;83:596–605.
Parnes LS, McClure JA. Posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1990;99:330–4.
Walsh RM, Bath AP, Cullen JR, Rutka JA. Long-term results of posterior semi-circular canal occlusion for intractable benign paroxysmal positional vertigo. Clin Otolaryngol. 1999;24:316–23.
Seo T, Hashimoto M, Saka N, Sakagami M. Hearing and vestibular functions after plugging surgery for the posterior semicircular canal. Acta Otolaryngol. 2009;129:1148–52.
Agrawal SK, Parnes LS. Human experience with canal plugging. Ann N Y Acad Sci. 2001;942:300–5.
Kisilevsky V, Bailie NA, Dutt SN, Rutka JA. Lessons learned from the surgical management of benign paroxysmal positional vertigo: the University Health Network experience with posterior semicircular canal occlusion surgery (1988-2006). J Otolaryngol Head Neck Surg. 2009;38:212–21.
Li JC. Mastoid oscillation: a critical factor for success in canalith repositioning procedure. Otolaryngol Head Neck Surg. 1995;112:670–5.
Ruckenstein MJ, Shepard NT. The canalith repositioning procedure with and without mastoid oscillation for the treatment of benign paroxysmal positional vertigo. ORL J Otorhinolaryngol Relat Spec. 2007;69:295–8.
Hain TC, Helminski JO, Reis IL, Uddin MK. Vibration does not improve results of the canalith repositioning procedure. Arch Otolaryngol Head Neck Surg. 2000;126:617–22.
Otsuka K, Suzuki M, Negishi M, et al. Efficacy of physical therapy for intractable cupulolithiasis in an experimental model. J Laryngol Otol. 2013;127:463–7.
Compliance with Ethics Guidelines
Conflict of Interest
Daniel Gold, Laura Morris, Amir Kheradmand, and Michael Schubert all declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Neurologic Ophthalmology and Otology
Rights and permissions
About this article
Cite this article
Gold, D.R., Morris, L., Kheradmand, A. et al. Repositioning Maneuvers for Benign Paroxysmal Positional Vertigo. Curr Treat Options Neurol 16, 307 (2014). https://doi.org/10.1007/s11940-014-0307-4
Published:
DOI: https://doi.org/10.1007/s11940-014-0307-4