Abstract
Ventilator-associated pneumonia (VAP), an infection of the lower respiratory tract which occurs in association with mechanical ventilation, is one of the most common causes of nosocomial infection in the intensive care unit (ICU). VAP causes significant morbidity and mortality in critically ill patients including increased duration of mechanical ventilation, ICU stay and hospitalization. Current knowledge for its prevention, diagnosis and management is therefore important clinically and is the basis for this review. We discuss recent changes in VAP surveillance nomenclature incorporating ventilator-associated conditions and ventilator-associated events, terms recently proposed by the Centers for Disease Control. To the extent possible, we rely predominantly on data from randomized control trials (RCTs) and meta-analyses.
Similar content being viewed by others
Introduction
Ventilator-associated pneumonia (VAP) is an infection of the lower respiratory tract associated with endotracheal intubation and which causes significant morbidity and mortality in the intensive care unit (ICU). It is one of the most common health-care-associated infections arising in the ICU [1]. Approximately 10 % of ventilated patients will develop the disease, with the risk of VAP rising as the duration of mechanical ventilation increases reaching a maximum on day 5 post-intubation [2]. Pooled rates of 0–4.4 cases of VAP per 1000 days of mechanical ventilation have been reported from surveillance data with the rates depending on the underlying population, type of ICU and surveillance method [3]. The degree of VAP-attributable mortality is controversial, but well-conducted studies reported it as being significant and between 1 to 1.5 % [4, 5]. Further, VAP is associated with significant morbidity as it significantly increases the length of stay in the ICU, the duration of mechanical ventilation and hospital stay [6]. The cost to the health care system has been estimated to range from $10,000 to $13,000 USD per case of VAP [7, 8]. In addition, VAP has longitudinal deleterious effects at the level of the individual patient, leading to the increased utilization of the health care system after ICU, further increasing the economic burden of this disease [9].The implications for the individual patient and the cost to the health care system underscore the importance of VAP prevention, along with its early diagnosis and effective management. There have been recent changes to the nomenclature used for surveillance of VAP and VAP-related phenomenon, as well as advances in the diagnosis of VAP and treatment modalities for the disease, all of which will be focus of this review.
Pathophysiology of VAP
The pathophysiology of VAP is mediated largely by the introduction of a foreign body, the endotracheal tube (ETT), into the upper airway [10]. This subverts the patient’s natural mechanisms for preventing access of microorganisms to the lower respiratory tract. ETTs are associated with significant impairment of mucociliary clearance of secretions, the formation of bacterial biofilms upon the ETT polymer, microaspiration and leakage of oropharyngeal secretions around the inflated ETT cuff (Fig. 1) [10–12]. These are exacerbated in the context of positive pressure ventilation, which combines with gravity to move secretions and microorganisms into the distal respiratory tract. Additionally, it is becoming increasingly recognized that critically ill patients have impaired innate and adaptive immunity [13]. This is an emerging area of critical care medicine that will influence our understanding of the pathophysiology of VAP and its response to treatment in the future.
Bacteriology of VAP
There is a diversity of microorganisms that cause VAP including both gram-negative and gram-positive organisms. Traditionally, the duration of mechanical ventilation was felt to be one of the most important factors determining the composition of offending VAP pathogens [14, 15]. For example, in early VAP (typically considered <5 days of mechanical ventilation), Haemophilus influenzae, Streptococcus pneumoniae, methicillin-sensitive Staphylococcus aureus (MSSA), or Enterobacteriaceae were considered to be the predominant pathogens. In contrast, in late VAP (>5 days of mechanical ventilation), multidrug-resistant organisms, such as Pseudomonas aeruginosa, Acinetobacter spp., and methicillin-resistant S. aureus (MRSA) were considered to predominate. However, there have been recent studies which contradict this [16–18, 19•, 20]. Indeed, Restrepo et al. and Golia et al. showed that P. aeruginosa and Acinetobacter baumanii were isolated from both early and late-VAP patients [16, 19•]. Chi et al. also found that there was no difference in VAP isolates from early or late sources [20]. Importantly, Martin-Loeches et al. examined pathogens from VAP patients with and without risk factors for infection with multidrug resistant (MDR) organisms. They found that patients at risk for MDR infection had higher rates of these pathogens which included P. aeruginosa and A. baumanii, MRSA and Stenotrophomonas maltophilia. In contrast, patients not at risk for infection with MDR organisms had higher rates of MSSA, S. pneumonia, and H. influenzae. Based on this, the bacteriology of VAP may not follow a pattern of early versus late infection, particularly in patients that are at risk for MDR infections.
Furthermore, the type of ICU population (i.e. medical, surgical and trauma) can also be associated with specific microorganisms as the causative VAP agent. For example, A. baumanii and S. aureus have been linked with VAP that develops in neurosurgical and head trauma patients [21, 22]. Trauma patients have higher rates of infection with Haemophilus sp. or S. pneumonia [21]; COPD patients are at higher risk for H. influenzae and Moraxella catarrhalis; patients with underlying bronchiectasis are often infected with P. aeruginosa and S. aureus [14, 15]. It is important to note, however, that the causative bacteria can also differ among critical care centres. This final point underscores the importance of having unit and hospital-specific antibiograms to guide empiric therapy of VAP.
Diagnosis of VAP
Traditionally, the clinical diagnosis of VAP has included a combination of the following: clinical symptoms/signs, chest radiography, and microbiological data [23]. Clinical symptoms and signs include changes in sputum or tracheal secretions in terms of purulence, colour and/or increasing production; cough; temperature >38 or <36 °C; rales or bronchial breath sounds on examination and worsening oxygenation. Laboratory findings include non-specific indicators of infection including leukocytosis (>12 × 109 WBC/L) or leukopenia (<4.0 × 109 WBC/L). Findings on chest radiography (CXR) include the development of new infiltrates or the presence of persistent and/or worsening infiltrates. Published case definitions for VAP have included a variety of combinations of these [24, 25].
There is no reference standard for the diagnosis of VAP, and clinical criteria plus microbiological sampling techniques lack specificity and sensitivity when compared to the demonstration of pneumonia on histological samples obtained by either biopsy or necropsy [26]. For example, clinical criteria alone have been reported to have a sensitivity and specificity of 91 and 15 % [26].
Similarly, the Clinical Pulmonary Infection Score (CPIS) uses a combination of CXR and clinical, physiological and microbiological information for the diagnosis of VAP [27]. However, a recent meta-analysis of 13 studies showed that the sensitivity and specificity for diagnosing VAP were about 65 % for each of these [28] confirming an older post-mortem study of mechanically ventilated patients in which the sensitivity and specificity were less than 70 % [29]. This is not surprising given that infiltrates on CXR can have multiple aetiology types other than infection, such as pulmonary oedema, atelectasis, acute respiratory distress syndrome, and other causes in mechanically ventilated patients [30]. Indeed, the most accurate predictor for autopsy-proven VAP on CXR was the presence of air bronchograms but this was also low [29]. As well, the aetiology of other clinical criteria such as fever or leukocytosis/leukopenia in critically ill patients is also broad. In the absence of a reference standard and the poor reliability of clinical criteria, the clinician needs to weigh all factors, including the overall clinical status of the patient, to arrive at a treatment decision.
Respiratory tract sampling should be routinely conducted when there is a clinical suspicion of VAP. This can be done via non-bronchoscopic or bronchoscopic techniques. Bronchoscopic sampling includes bronchoalveolar lavage (BAL) or protected specimen brush (PSB), while non-bronchoscopic techniques include endotracheal aspirates and mini-BAL. Bacterial growth in semi-quantitative cultures is usually reported as heavy, moderate, light or no growth. Typically, quantitative cultures are done on BAL or PSB specimens, while semi-quantitative cultures are done on other samples such as endotracheal aspirates. If quantitative cultures are done, thresholds have been ascribed to the presence of infection as 104 colony forming units/mL (cfu/mL) for BAL and 103 cfu/mL for PSB. Although quantitative cultures are touted as being more specific for infection, a recent Cochrane analysis that included five randomized control trials (RCTs) (n = 1240 patients) found no change in mortality, days on mechanical ventilation, number of days in the ICU, or antibiotic utilization when compared to semi-quantitative cultures [31]. In the absence of demonstrated superiority of one technique over another, the relative invasiveness of bronchoscopy and its requirement for specialized expertise and equipment, endotracheal aspirates are the preferred method of respiratory tract sampling for microbiology. There may be other indications for bronchoscopy such tracheobronchial toileting, but there is little rationale for its routine utilization for the diagnosis of VAP.
Ventilator-Associated Events: New Terminology and Its Relationship to VAP
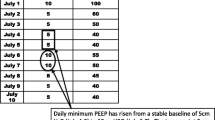
Previous clinical and laboratory definitions of VAP, given their limited sensitivity and specificity, are not ideal for surveillance and reporting, a critical issue if used as a metric of quality of care received [32•]. Therefore, the CDC developed new surveillance criteria for deterioration in the status of mechanically ventilated patients (http://www.cdc.gov/nhsn/acute-care-hospital/vae). This was termed a ventilator-associated event (VAE) and aims to capture all complications leading to the worsening of gas exchange in mechanically ventilated patients, which could include VAP. This deterioration is objectively defined as an increase in positive end-expiratory pressure (PEEP) of at least 3 cm H2O for the maintenance of oxygenation in an individual patient whose PEEP was stable or falling in the 3 days prior to the increase and/or a greater than 20 % increase in the daily minimum FiO2. Importantly, the aetiology of hypoxemia is not part of this definition.
The VAE system has three tiers: ventilator-associated conditions (VACs), infection-related VAC (iVAC) and VAP (Fig. 2). VAC identifies patients who meet only the criteria for VAE as outlined above and none of the criteria for iVAC and VAP. For iVAC, the patient meets the definition of VAC, but there is an associated infectious or inflammatory process; iVAC patients are required to have an abnormal temperature (>38 or <36 °C), leukocytosis or leukopenia (>12,000 or <4000 WBC/L) and be treated with antibiotics for at least 4 days. The third tier is ‘probable or possible VAP’. Here, the patient is required to have the criteria for iVAC but also have quantitative (endotracheal aspirate ≥105 CFU/mL, BAL ≥104 CFU/mL, lung tissue ≥104 CFU/g, PSB ≥103 CFU/mL) or semi-quantitative cultures growing respiratory pathogens.
VAE definition algorithm for surveillance. From CDC NHSN Ventilator-associated Events (VAE) http://www.cdc.gov/nhsn/PDFs/pscManual/10-VAE_FINAL.pdf
These new definitions expand the focus of surveillance from VAP alone to include other deleterious complications that may arise in mechanically ventilated patients. They are advantageous in that they are objective, are easier to collect and can be tracked and quantified using electronic medical records. Furthermore, Klompas et al. demonstrated that VAEs are associated with increased days of mechanical ventilation, length of hospital stay and increased mortality [33].
However, in observational studies, it has been found that there is poor agreement between VAC, iVACs and VAP as determined by traditional clinical criteria [34]. The main causes of VAE are atelectasis, pulmonary oedema, acute respiratory distress syndrome and pneumonia [32•]. Although there is a suggestion that measures designed to prevent VAP as traditionally defined may also improve the rate of VAE, this is not clear [34]. Surveillance for VAE has not been shown to improve patient outcomes and further study is required. Ideally, the prevention of VAEs, as for traditional VAP, could ultimately improve patient outcomes and decrease health care cost; however, at this point, it is unknown if this will happen and studies are needed to determine this.
Biomarkers for VAP
An ideal VAP biomarker would be a measurable entity in serum or in BAL fluid (BALF) that is reliably elevated or down-regulated in patients with VAP, is responsive to therapy and is not altered in critically ill patients without VAP. The rationale for using biomarkers is that the clinical criteria for the diagnosis and management of VAP are unreliable and that biomarkers would be useful to facilitate its early diagnosis and treatment. The most studied and promising serum biomarker is procalcitonin.
Procalcitonin is a protein containing 116 amino acids and is the precursor to the calcium regulatory molecule, calcitonin [35]. It is up-regulated in response to inflammation, and it is useful for the differentiation of bacterial and non-bacterial inflammatory states [36].Increased plasma procalcitonin levels are associated with VAP; in a recent meta-analysis (including seven studies that involved 373 patients), it was found to have a sensitivity and specificity of 76 and 79 % [37]. Furthermore, serial procalcitonin monitoring has been used as a strategy to aid in the discontinuation of antibiotic therapy [38, 39]. In three studies (with a total of 323 patients) in which a drop in procalcitonin level below a set threshold was used as a trigger to stop antibiotic therapy, there was a significant decrease in days of antibiotic therapy (9.2 days for the procalcitonin group vs. 12.1 days for the conventional group) [38]. However, although promising, antibiotic discontinuation based on procalcitonin monitoring still requires further study. Procalcitonin monitoring may not be applicable to institutions or clinicians who have adopted shorter courses of antibiotic therapy of 7–8 days as recommended in many guidelines [40].
Biomarkers can also be isolated from BALF, and these include (but are not limited to) the proinflammatory cytokines interleukin-1β (IL-1β), interleukin-8 (IL-8), and triggering receptor expressed on myeloid cells-1 (TREM-1), the latter a member of the immunoglobulin superfamily. Both IL-1β and IL-8 are significantly elevated in BALF from patients with confirmed VAP [41]. Hellyer et al. carried out a prospective, multicentre study which showed that there is a high negative predictive value when IL-1β and IL-8 are used together [41]. In combination, they were found to have a sensitivity of 94 %, with specificity of 56 %, and negative predictive value of 97 %. TREM-1 has generated significant interest, and although promising when initially described, later data have demonstrated conflicting results [42]. In a recent observational study, TREM-1 levels isolated from BALF were not able to identify VAP patients when compared to quantitative respiratory cultures as the gold standard, with a sensitivity and specificity of 79 and 23 % [43]. In contrast, however, Grover et al. showed thatTREM-1 levels in BALF and expressed on the surface of neutrophils and monocytes were higher in VAP versus non-VAP patients [44].
At this time, the data for biomarkers are conflicting and there is no single reliable biomarker from the serum or BALF available for the diagnosis of VAP although procalcitonin is promising as an aid for the management of VAP. Further study is required in this regard, and in the future, biomarkers will most likely find utility in conjunction with clinical and culture criteria to aid in the diagnosis and management of VAP.
Prevention of VAP
Current modalities for the prevention of VAP (Table 1), and the evidence for these modalities, are based on the traditional definition of VAP. It is unknown if VACs and iVACs are preventable with the VAP prevention modalities.
Non-invasive Positive Pressure Ventilation (NIPPV)
Avoiding intubation and limiting the duration of mechanical ventilation can reduce the occurrence of VAP. Use of NIPPV is one important way to either avoid the need for intubation or terminate mechanical ventilation as early as possible by extubation to NIPPV. In a meta-analysis including 12 studies, the rate of pneumonia in patients while on NIPPV was lower than in mechanically ventilated patients at 2 and 10 %, respectively [45]. Furthermore, data from a recent Cochrane Review suggest that NIPPV used as a weaning strategy from mechanical ventilation, primarily in COPD patients, may reduce the rate of VAP without increasing the risk of subsequent reintubation [46•].
Positioning
Limiting aspiration of oropharyngeal secretions is a further strategy to prevent VAP. This can be done in part by maintaining a semi-recumbent position to maintain the head of the bed between 30 and 45°. A meta-analysis of three RCTs investigating the efficacy of semi-recumbent versus the supine position found an odds ratio of 0.47 (n = 337 patients, confidence interval 0.27–0.82) for the development of VAP [47]. Given that this is a simple intervention, it is worth implementing unless there are contraindications in the specific patient. Many patients, such as those who are haemodynamically unstable, have unstable spinal fractures or are morbidly obese and may not be candidates for semi-recumbent positioning, and concerns have been raised over the occurrence of sacral ulcers.
Probiotics
There is early evidence that probiotics may be both safe and effective at decreasing the incidence of VAP [48]. A recent Cochrane analysis which included eight RCTs and included 1083 patients who received various forms of probiotics (e.g. Lactobacillus, Ergyphilus and Bifidobacterium) found that the incidence of VAP was significantly lower in patients who received probiotics compared to controls, but there was uncertainty as to their effect on mortality, days of mechanical ventilation and length of ICU stay. The quality of evidence in these studies was either low quality or very low quality, and further study is required before probiotics are routinely implemented. RCTs which will provide further evidence in this regard are currently underway (https://clinicaltrials.gov/ct2/show/NCT01782755).
ETT Modifications
Endotracheal tubes represent a foreign body in the upper airway and are prone to bacterial colonization and the development of biofilms. Biofilms are highly organized bacterial structures hindering the penetration of antibiotics and thus protecting the bacteria ensconced in them. The evaluation of ETTs coated in silver as a means to retard bacterial growth and biofilm formation has been conducted; Rello et al. demonstrated that intubated patients with silver-coated ETTs grew fewer pathogens than those with non-coated ETTs [49]. A subsequent multicentre, prospective, randomized study by Kollef et al. showed that the incidence of VAP was lower in patients intubated with a silver-coated ETT compared to non-coated tubes, with VAP rates of 4.8 and 7.5 %, respectively [50]. There was, however, no statistically significant difference between the two cohorts in mortality, length of ICU stay and duration of mechanical ventilation.
Use of endotracheal tubes with subglottic secretion drainage ports can limit aspiration of oropharyngeal secretions. In a meta-analysis of 13 RCTs studying the efficacy of subglottic secretion drainage, 12 of these RCTs demonstrated a decrease in the rates of VAP, and overall, there was a decrease in length of ICU stay and days of mechanical ventilation [51]. There was, however, no decrease in mortality. Interestingly, in a recent RCT by Damas et al., comparing the efficacy of subglottic secretion drainage on rates of VAP and VAC, they determined that subglottic secretion drainage decreased the frequency of VAP, length of ICU stay, and days of mechanical ventilation but did not reduce the frequency of VAC [52•]. There has not been any comparison of silver-coated ETTs with ETTs with subglottic secretion drainage; although there is evidence for the effectiveness of both, the lower cost and extent of study of ETTs with subglottic secretion drainage would favour their utilization over silver-coated ETTs.
The maintenance of ETT cuff pressure, by automated or continuous means compared to an intermittent manual method, can also potentially reduce the aspiration of oropharyngeal secretions and thus VAP. In two recently reported trials, the use of continuous cuff pressure control resulted in a decrease in the incidence of VAP [53, 54] but contradicted earlier results by Valencia et al. [55]. In all these studies, there was no significant difference in mortality, days of mechanical ventilation, and length of ICU stay.
Oral Hygiene
A recent meta-analysis which included 35 RCTs (5374 patients) by Shi et al. demonstrated a significant benefit of preventing VAP with oral care using chlorhexidine mouth wash compared to placebo [56]. The number needed to treat (NNT) was 15, meaning that for every 15 mechanically ventilated patients treated with chlorhexidine, one incidence of VAP will be prevented. There was no significant benefit on mortality, days of mechanical ventilation or length of ICU stay. A recent RCT by Munro et al. used chlorhexidine prior to intubation to determine if this would decrease the rates of VAP compared to patients who were not pre-treated with chlorhexidine before being intubated [57]. All patients subsequently received chlorhexidine twice daily. There was no statistically significant difference in the rates of VAP in these two treatment groups, suggesting that pre-treatment with chlorhexidine is ineffective at preventing VAP and that the clinician should focus on more important tasks during intubation.
Treatment of VAP
Inappropriate or delayed antibacterial treatment of VAP is important because it has been associated with increased VAP mortality [58, 59]. The administration of empiric antimicrobial therapy should therefore be initiated as early as possible when VAP is suspected. If possible, respiratory and blood samples for culture should be taken prior to the administration of antibiotics to guide continued therapy. There is no universal regimen for VAP treatment. Important factors influencing the choice of empiric therapy include but are not limited to institutional or unit-specific antibiograms and patient risk factors including any prior cultures or colonization data, duration of mechanical ventilation, prior exposure to other antibiotics and severity of the illness. All empiric antibiotic therapy should include coverage for both gram positive and gram-negative organisms.
Indeed, if the patient has been on mechanical ventilation for less than 3–5 days and has no risk factors for developing multiple-drug-resistant infection (e.g. methicillin-resistant S. aureus, P. aeruginosa and extended-spectrum beta-lactamases), monotherapy with fluoroquinolone, third-generation cephalosporin or a penicillin + beta-lactamase inhibitor would provide appropriate antimicrobial coverage.
If the patient has been on prolonged mechanical ventilation >3–5 days, has risk factors for MDR infection, or has a history of previous MDR infection, treatment should reflect a combination of drugs that provides coverage for these organisms including Pseudomonas. For pseudomonal coverage, there are several options which include third of fourth-generation cephalosporins, an aminopenicillin + beta-lactamase inhibitor, an antipseudomonal fluoroquinolone, the carbapenems (but not ertapenem), aminoglycosides or aztreonam. In many institutions where there is significant antibiotic resistance, to ensure that the empiric coverage is appropriate, double antipseudomonal coverage is required to ensure that all the responsible pathogens are susceptible to a least one of the antibiotics. In institutions or ICUs with high rates of MRSA or where there are risk factors for MRSA, gram-positive coverage should include either vancomycin or linezolid.
There has been considerable debate concerning the efficacy of vancomycin compared to that of linezolid for the treatment of MRSA VAP with studies demonstrating conflicting results [60–64]. However, in a meta-analysis by Kalil et al. of RCTs, enrolling a total of 2329 patients, there was no difference in mortality between vancomycin and linezolid in treating VAP, but there was a significant increased risk of thrombocytopenia and gastrointestinal side effects with linezolid [65•]. Given that there is no convincing evidence of the superiority of one agent over another; both vancomycin and linezolid can be considered to be equally efficacious for the treatment of MRSA VAP.
In general, there is reasonable consensus that shorter duration of treatment for VAP is adequate. In an RCT, comparing 8 and 15 days of antibiotic therapy, there was no difference in mortality in patients treated for 8 days [66], and this was confirmed in a meta-analysis [67•] and a 2011 Cochrane study which included eight studies involving 1703 patients [38]. Optimal treatment duration for MDR VAP or recurrent VAP has not been yet determined [68].
Conclusions
VAP is associated with significant morbidity and mortality in critically ill mechanically ventilated patients and has deleterious economic impact on the health care system. The most important step in the approach to VAP is therefore its prevention. There are many preventative modalities which have been demonstrated to be effective. These include the utilization of NIPPV, oral hygiene measures, modification of ETTs (subglottic secretion drainage or silver-coated) and positioning. There are other promising preventive measures such as probiotics, but they require further study.
The management of VAP relies upon its prompt diagnosis and involves clinical signs, laboratory investigations, chest radiography, and microbiological data from lung cultures. Unfortunately, a reference standard for VAP remains elusive, and further advances in rapid, definitive diagnosis may lie in the use of biomarkers from the serum or BALF although this will not occur in the near future.
Finally, there has been significant evolution for the surveillance of VAP. These terms, VAC and iVACs, do not replace the traditional diagnosis of VAP but capture a broader variety of pathologies including pneumonia that may impair gas exchange in mechanically ventilated patients. The preventability of VAC and iVACs as a broad category needs to be determined and requires further study.
The decision on the antimicrobial management of VAP is a multifaceted that begins with consideration of the duration of ventilation; risk factors for infection with MDR organisms; and the potential causative microorganisms based on institutional factors, prior cultures and any screening that has taken place.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, et al. The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA. 1995;274(8):639–44.
Cook DJ, Walter SD, Cook RJ, Griffith LE, Guyatt GH, Leasa D, et al. Incidence of and risk factors for ventilator-associated pneumonia in critically ill patients. Ann Intern Med. 1998;129(6):433–40.
Dudeck MA, Horan TC, Peterson KD, Allen-Bridson K, Morrell G, Anttila A, et al. National Healthcare Safety Network report, data summary for 2011, device-associated module. Am J Infect Control. 2013;41(4):286–300.
Melsen WG, Rovers MM, Groenwold RH, Bergmans DC, Camus C, Bauer TT, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013;13(8):665–71.
Bekaert M, Timsit JF, Vansteelandt S, Depuydt P, Vesin A, Garrouste-Orgeas M, et al. Attributable mortality of ventilator-associated pneumonia: a reappraisal using causal analysis. Am J Respir Crit Care Med. 2011;184(10):1133–9.
Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review. Crit Care Med. 2005;33(10):2184–93.
Restrepo MI, Anzueto A, Arroliga AC, Afessa B, Atkinson MJ, Ho NJ, et al. Economic burden of ventilator-associated pneumonia based on total resource utilization. Infect Control Hosp Epidemiol. 2010;31(5):509–15.
Muscedere JG, Martin CM, Heyland DK. The impact of ventilator-associated pneumonia on the Canadian health care system. J Crit Care. 2008;23(1):5–10.
Yang CC, Shih NC, Chang WC, Huang SK, Chien CW. Long-term medical utilization following ventilator-associated pneumonia in acute stroke and traumatic brain injury patients: a case-control study. BMC Health Serv Res. 2011;11:289.
Zolfaghari PS, Wyncoll DL. The tracheal tube: gateway to ventilator-associated pneumonia. Crit Care. 2011;15(5):310.
Rubin BK, Dhand R, Ruppel GL, Branson RD, Hess DR. Respiratory care year in review 2010: part 1. Asthma, COPD, pulmonary function testing, ventilator-associated pneumonia. Respir Care. 2011;56(4):488–502.
D’Haese J, De Keukeleire T, Remory I, Van Rompaey K, Umbrain V, Poelaert J. Assessment of intraoperative microaspiration: does a modified cuff shape improve sealing? Acta Anaesthesiol Scand. 2013;57(7):873–80.
Conway Morris A, Anderson N, Brittan M, Wilkinson TS, McAuley DF, Antonelli J, et al. Combined dysfunctions of immune cells predict nosocomial infection in critically ill patients. Br J Anaesth. 2013;111(5):778–87.
Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867–903.
Quartin AA, Scerpella EG, Puttagunta S, Kett DH. A comparison of microbiology and demographics among patients with healthcare-associated, hospital-acquired, and ventilator-associated pneumonia: a retrospective analysis of 1184 patients from a large, international study. BMC Infect Dis. 2013;13:561.
Golia S, Sangeetha KT, Vasudha CL. Microbial profile of early and late onset ventilator associated pneumonia in the intensive care unit of a tertiary care hospital in Bangalore, India. J Clin Diagn Res. 2013;7(11):2462–6.
Charles MP, Easow JM, Joseph NM, Ravishankar M, Kumar S, Sivaraman U. Aetiological agents of ventilator-associated pneumonia and its resistance pattern - a threat for treatment. Australas Med J. 2013;6(9):430–4.
Martin-Loeches I, Deja M, Koulenti D, Dimopoulos G, Marsh B, Torres A, et al. Potentially resistant microorganisms in intubated patients with hospital-acquired pneumonia: the interaction of ecology, shock and risk factors. Intensive Care Med. 2013;39(4):672–81.
Restrepo MI, Peterson J, Fernandez JF, Qin Z, Fisher AC, Nicholson SC. Comparison of the bacterial etiology of early-onset and late-onset ventilator-associated pneumonia in subjects enrolled in 2 large clinical studies. Respir Care. 2013;58(7):1220–5. Study demonstrating that multi-drug resistant organisms can be found in both early and late VAP isolates, whereas previously, these organisms were thought to be primarily found in late VAP.
Chi SY, Kim TO, Park CW, Yu JY, Lee B, Lee HS, et al. Bacterial pathogens of ventilator associated pneumonia in a tertiary referral hospital. Tuberc Respir Dis. 2012;73(1):32–7.
Baker AM, Meredith JW, Haponik EF. Pneumonia in intubated trauma patients. Microbiology and outcomes. Am J Respir Crit Care Med. 1996;153(1):343–9.
Rello J, Torres A, Ricart M, Valles J, Gonzalez J, Artigas A, et al. Ventilator-associated pneumonia by Staphylococcus aureus. Comparison of methicillin-resistant and methicillin-sensitive episodes. Am J Respir Crit Care Med. 1994;150(6 Pt 1):1545–9.
Klompas M. Does this patient have ventilator-associated pneumonia? JAMA. 2007;297(14):1583–93.
Hansen S, Sohr D, Geffers C, Astagneau P, Blacky A, Koller W, et al. Concordance between European and US case definitions of healthcare-associated infections. Antimicrob Resist Infect Control. 2012;1(1):28.
Mietto C, Pinciroli R, Patel N, Berra L. Ventilator associated pneumonia: evolving definitions and preventive strategies. Respir Care. 2013;58(6):990–1007.
Tejerina E, Esteban A, Fernandez-Segoviano P, Frutos-Vivar F, Aramburu J, Ballesteros D, et al. Accuracy of clinical definitions of ventilator-associated pneumonia: comparison with autopsy findings. J Crit Care. 2010;25(1):62–8.
Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic “blind” bronchoalveolar lavage fluid. Am Rev Respir Dis. 1991;143(5 Pt 1):1121–9.
Shan J, Chen HL, Zhu JH. Diagnostic accuracy of clinical pulmonary infection score for ventilator-associated pneumonia: a meta-analysis. Respir Care. 2011;56(8):1087–94.
Wunderink RG, Woldenberg LS, Zeiss J, Day CM, Ciemins J, Lacher DA. The radiologic diagnosis of autopsy-proven ventilator-associated pneumonia. Chest. 1992;101(2):458–63.
Grgurich PE, Hudcova J, Lei Y, Sarwar A, Craven DE. Diagnosis of ventilator-associated pneumonia: controversies and working toward a gold standard. Curr Opin Infect Dis. 2013;26(2):140–50.
Berton DC, Kalil AC, Teixeira PJ. Quantitative versus qualitative cultures of respiratory secretions for clinical outcomes in patients with ventilator-associated pneumonia. Cochrane Database Syst Rev. 2014;10, CD006482.
Raoof S, Baumann MH. An official multi-society statement: ventilator-associated events: the new definition. Crit Care Med. 2014;42(1):228–9. This manuscript provides a concise overview of the new nomenclature and definitions of VAC and VAEs.
Klompas M, Kleinman K, Murphy MV. Descriptive epidemiology and attributable morbidity of ventilator-associated events. Infect Control Hosp Epidemiol. 2014;35(5):502–10.
Muscedere J, Sinuff T, Heyland DK, Dodek PM, Keenan SP, Wood G, et al. The clinical impact and preventability of ventilator-associated conditions in critically ill patients who are mechanically ventilated. Chest. 2013;144(5):1453–60.
Maruna P, Nedelnikova K, Gurlich R. Physiology and genetics of procalcitonin. Physiol Res. 2000;49 Suppl 1:S57–61.
Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet. 2004;363(9409):600–7.
Sotillo-Diaz JC, Bermejo-Lopez E, Garcia-Olivares P, Peral-Gutierrez JA, Sancho-Gonzalez M, Guerrero-Sanz JE. Role of plasma procalcitonin in the diagnosis of ventilator-associated pneumonia: systematic review and metaanalysis. Med Intensiva. 2014;38(6):337–46.
Pugh R, Grant C, Cooke RP, Dempsey G. Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults. Cochrane Database Syst Rev. 2011;10, CD007577.
Heyland DK, Johnson AP, Reynolds SC, Muscedere J. Procalcitonin for reduced antibiotic exposure in the critical care setting: a systematic review and an economic evaluation. Crit Care Med. 2011;39(7):1792–9.
American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
Hellyer TP, Conway Morris A, McAuley DF, Walsh TS, Anderson NH, Singh S, et al. Diagnostic accuracy of pulmonary host inflammatory mediators in the exclusion of ventilator-acquired pneumonia. Thorax. 2015:70(1):41–7.
Gibot S, Cravoisy A, Levy B, Bene MC, Faure G, Bollaert PE. Soluble triggering receptor expressed on myeloid cells and the diagnosis of pneumonia. N Engl J Med. 2004;350(5):451–8.
Palazzo SJ, Simpson TA, Simmons JM, Schnapp LM. Soluble triggering receptor expressed on myeloid cells-1 (sTREM-1) as a diagnostic marker of ventilator-associated pneumonia. Respir Care. 2012;57(12):2052–8.
Grover V, Pantelidis P, Soni N, Takata M, Shah PL, Wells AU, et al. A biomarker panel (Bioscore) incorporating monocytic surface and soluble TREM-1 has high discriminative value for ventilator-associated pneumonia: a prospective observational study. PLoS ONE. 2014;9(10), e109686.
Hess DR. Noninvasive positive-pressure ventilation and ventilator-associated pneumonia. Respir Care. 2005;50(7):924–9. discussion 929-931.
Burns KE, Meade MO, Premji A, Adhikari NK. Noninvasive positive-pressure ventilation as a weaning strategy for intubated adults with respiratory failure. Cochrane Database Syst Rev. 2013;12, CD004127. This Cochrane Review demonstrates that NIPPV can facilitate earlier extubation and as such this is associated with decreased VAP rates and decreased mortality.
Alexiou VG, Ierodiakonou V, Dimopoulos G, Falagas ME. Impact of patient position on the incidence of ventilator-associated pneumonia: a meta-analysis of randomized controlled trials. J Crit Care. 2009;24(4):515–22.
Bo L, Li J, Tao T, Bai Y, Ye X, Hotchkiss RS, et al. Probiotics for preventing ventilator-associated pneumonia. Cochrane Database Syst Rev. 2014;10, CD009066.
Rello J, Kollef M, Diaz E, Sandiumenge A, del Castillo Y, Corbella X, et al. Reduced burden of bacterial airway colonization with a novel silver-coated endotracheal tube in a randomized multiple-center feasibility study. Crit Care Med. 2006;34(11):2766–72.
Kollef MH, Afessa B, Anzueto A, Veremakis C, Kerr KM, Margolis BD, et al. Silver-coated endotracheal tubes and incidence of ventilator-associated pneumonia: the NASCENT randomized trial. JAMA. 2008;300(7):805–13.
Muscedere J, Rewa O, McKechnie K, Jiang X, Laporta D, Heyland DK. Subglottic secretion drainage for the prevention of ventilator-associated pneumonia: a systematic review and meta-analysis. Crit Care Med. 2011;39(8):1985–91.
Damas P, Frippiat F, Ancion A, Canivet JL, Lambermont B, Layios N, et al. Prevention of ventilator-associated pneumonia and ventilator-associated conditions: a randomized controlled trial with subglottic secretion suctioning. Crit Care Med. 2015;43(1):22–30. The main finding of this study is that subglottic secretion suctioning reduces VAP rates and decreases antibiotic use, although it did not have effect of VAC rates.
Nseir S. Endotracheal cuff pressure monitoring: another alarm in the ICU? Am J Crit Care. 2011;20(6):422–3. author reply 423-424.
Lorente L, Lecuona M, Jimenez A, Lorenzo L, Roca I, Cabrera J, et al. Continuous endotracheal tube cuff pressure control system protects against ventilator-associated pneumonia. Crit Care. 2014;18(2):R77.
Valencia M, Ferrer M, Farre R, Navajas D, Badia JR, Nicolas JM, et al. Automatic control of tracheal tube cuff pressure in ventilated patients in semirecumbent position: a randomized trial. Crit Care Med. 2007;35(6):1543–9.
Shi Z, Xie H, Wang P, Zhang Q, Wu Y, Chen E, et al. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst Rev. 2013;8, CD008367.
Munro CL, Grap MJ, Sessler CN, Elswick RK Jr., Mangar D, Karlnoski-Everall R, et al. Pre-intubation application of oral chlorhexidine does not provide additional benefit in prevention of early onset ventilator-associated pneumonia. Chest. 2015;147(2):328–34.
Wilke M, Grube R. Update on management options in the treatment of nosocomial and ventilator assisted pneumonia: review of actual guidelines and economic aspects of therapy. Infect Drug Resist. 2013;7:1–7.
Kuti EL, Patel AA, Coleman CI. Impact of inappropriate antibiotic therapy on mortality in patients with ventilator-associated pneumonia and blood stream infection: a meta-analysis. J Crit Care. 2008;23(1):91–100.
Wunderink RG, Niederman MS, Kollef MH, Shorr AF, Kunkel MJ, Baruch A, et al. Linezolid in methicillin-resistant Staphylococcus aureus nosocomial pneumonia: a randomized, controlled study. Clin Infect Dis. 2012;54(5):621–9.
Wunderink RG, Mendelson MH, Somero MS, Fabian TC, May AK, Bhattacharyya H, et al. Early microbiological response to linezolid vs vancomycin in ventilator-associated pneumonia due to methicillin-resistant Staphylococcus aureus. Chest. 2008;134(6):1200–7.
Chan JD, Pham TN, Wong J, Hessel M, Cuschieri J, Neff M, et al. Clinical outcomes of linezolid vs vancomycin in methicillin-resistant Staphylococcus aureus ventilator-associated pneumonia: retrospective analysis. J Intensive Care Med. 2011;26(6):385–91.
Gonzalez RP, Rostas J, Simmons JD, Allen J, Frotan MA, Brevard SB. Improved outcome of ventilator-associated pneumonia caused by methicillin-resistant Staphylococcus aureus in a trauma population. Am J Surg. 2013;205(3):255–8. discussion 258.
Peyrani P, Wiemken TL, Kelley R, Zervos MJ, Kett DH, File Jr TM, et al. Higher clinical success in patients with ventilator-associated pneumonia due to methicillin-resistant Staphylococcus aureus treated with linezolid compared with vancomycin: results from the IMPACT-HAP study. Crit Care. 2014;18(3):R118.
Kalil AC, Murthy MH, Hermsen ED, Neto FK, Sun J, Rupp ME. Linezolid versus vancomycin or teicoplanin for nosocomial pneumonia: a systematic review and meta-analysis. Crit Care Med. 2010;38(9):1802–8. In a large metaanalysis of RCTs these authors demonstrate that there is no significant difference in linezolid compared to vancomycin for the treatment of MRSA VAP.
Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert D, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290(19):2588–98.
Dimopoulos G, Poulakou G, Pneumatikos IA, Armaganidis A, Kollef MH, Matthaiou DK. Short- vs long-duration antibiotic regimens for ventilator-associated pneumonia: a systematic review and meta-analysis. Chest. 2013;144(6):1759–67. This metaanalysis demonstrated that shorter durations of antibiotic treatment for VAP are not associated with worse outcomes as compared to longer durations of antibiotic therapy.
Garnacho-Montero J, Corcia-Palomo Y, Amaya-Villar R, Martin-Villen L. How to treat VAP due to MDR pathogens in ICU patients. BMC Infect Dis. 2014;14:135.
Compliance with Ethics Guidelines
Conflict of Interest
Braden Waters and John Muscedere have no relevant disclosures.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Sepsis and ICU
Rights and permissions
About this article
Cite this article
Waters, B., Muscedere, J. A 2015 Update on Ventilator-Associated Pneumonia: New Insights on Its Prevention, Diagnosis, and Treatment. Curr Infect Dis Rep 17, 41 (2015). https://doi.org/10.1007/s11908-015-0496-3
Published:
DOI: https://doi.org/10.1007/s11908-015-0496-3