Abstract
Introduction and Purpose
Sleeve gastrectomy (SG) is gaining ground in the field of bariatric surgery. Data are scarce on its impact on esophagogastric physiology. Our aim was to evaluate the impact of SG on esophagogastric motility with high-resolution impedance manometry (HRIM) and to assess the usefulness of HRIM in patients with upper gastrointestinal (GI) symptoms after SG.
Methods
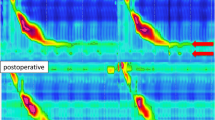
A retrospective analysis of 53 cases of HRIM performed after SG was conducted. Upper GI symptoms at the time of HRIM were scored. HRIM was analyzed according to the Chicago classification v3.0. A special attention was devoted to the occurrence of increased intragastric pressure (IIGP) after water swallows and reflux episodes as detected with impedance. A measurement of sleeve volume and diameter was performed with CT scan in a subgroup of patients.
Results
IIGP occurred very frequently in patients after SG (77 %) and was not associated with any upper GI symptoms, specific esophageal manometric profile, or impedance reflux. Impedance reflux episodes were also frequently observed after SG (52 %): they were significantly associated with gastroesophageal reflux (GER) symptoms and ineffective esophageal motility. The sleeve volume and diameters were also significantly smaller in patients with impedance reflux episodes (p < 0.01).
Conclusion
SG significantly modified esophagogastric motility. IIGP is frequent, not correlated to symptoms, and should be regarded as a HRIM marker of SG. Impedance reflux episodes were also frequent, associated with GER symptoms and esophageal dysmotility. HRIM may thus have a clinical impact on the management of patients with upper GI symptoms after SG.




Similar content being viewed by others
References
Keren D, Matter I, Rainis T. Sleeve gastrectomy in different age groups: a comparative study of 5-year outcomes. Obes Surg. 2016;26(2):289–95.
Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, roux-en-y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg 2015.
Buwen JP, Kammerer MR, Beekley AC, et al. Laparoscopic sleeve gastrectomy: The rightful gold standard weight loss surgery procedure. Surg Obes Relat Dis. 2015;11(6):1383–5.
Melissas J, Braghetto I, Molina JC, et al. Gastroesophageal reflux disease and sleeve gastrectomy. Obes Surg. 2015;25(12):2430–5.
Burgerhart JS, van de Meeberg PC, Mauritz FA, et al. Increased belching after sleeve gastrectomy. Obes Surg. 2016;26(1):132–7.
Biter LU, Gadiot RP, Grotenhuis BA, et al. The sleeve bypass trial: a multicentre randomized controlled trial comparing the long term outcome of laparoscopic sleeve gastrectomy and gastric bypass for morbid obesity in terms of excess BMI loss percentage and quality of life. BMC Obes. 2015;2:30.
Preissler C, Krieger-Grubel C, Borovicka J, et al. The contribution of intrabolus pressure to symptoms induced by gastric banding. J Gastrointestin Liver Dis. 2014;23:13–7.
Del Genio G, Tolone S, Limongelli P, et al. Sleeve gastrectomy and development of “de novo” gastroesophageal reflux. Obes Surg. 2014;24:71–7.
Burgerhart JS, Schotborgh CA, Schoon EJ, et al. Effect of sleeve gastrectomy on gastroesophageal reflux. Obes Surg. 2014;24:1436–41.
Burton PR, Brown WA, Laurie C, et al. Mechanisms of bolus clearance in patients with laparoscopic adjustable gastric bands. Obes Surg. 2010;20:1265–72.
Burton PR, Brown WA, Laurie C, et al. Pathophysiology of laparoscopic adjustable gastric bands: analysis and classification using high-resolution video manometry and a stress barium protocol. Obes Surg. 2010;20:19–29.
Lin Z, Carlson DA, Dykstra K, et al. High-resolution impedance manometry measurement of bolus flow time in achalasia and its correlation with dysphagia. Neurogastroenterol Motil. 2015;27:1232–8.
Park EJ, Lee JS, Lee TH, et al. High-resolution impedance manometry criteria in the sitting position indicative of incomplete bolus clearance. J Neurogastroenterol Motil. 2014;20:491–6.
Lin Z, Imam H, Nicodeme F, et al. Flow time through esophagogastric junction derived during high-resolution impedance-manometry studies: a novel parameter for assessing esophageal bolus transit. Am J Physiol Gastrointest Liver Physiol. 2014;307:G158–63.
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74.
do Carmo GC, Jafari J, Sifrim D, et al. Normal esophageal pressure topography metrics for data derived from the Sandhill-Unisensor high-resolution manometry assembly in supine and sitting positions. Neurogastroenterol Motil. 2015;27:285–92.
Herregods TV, Roman S, Kahrilas PJ, et al. Normative values in esophageal high-resolution manometry. Neurogastroenterol Motil. 2015;27:175–87.
Pandolfino JE, Kim H, Ghosh SK, et al. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol. 2007;102:1056–63.
Tutuian R, Castell DO. Combined multichannel intraluminal impedance and manometry clarifies esophageal function abnormalities: study in 350 patients. Am J Gastroenterol. 2004;99:1011–9.
Cansu A, Ahmetoglu A, Kul S, et al. Diagnostic performance of using effervescent powder for detection and grading of esophageal varices by multi-detector computed tomography. Eur J Radiol. 2014;83:497–502.
Vidal P, Ramon JM, Busto M, et al. Residual gastric volume estimated with a new radiological volumetric model: relationship with weight loss after laparoscopic sleeve gastrectomy. Obes Surg. 2014;24:359–63.
Cruiziat C, Roman S, Robert M, et al. High resolution esophageal manometry evaluation in symptomatic patients after gastric banding for morbid obesity. Dig Liver Dis. 2011;43:116–20.
Toro JP, Patel AD, Lytle NW, et al. Observed variability in sleeve gastrectomy volume and compliance does not correlate to postoperative outcomes. Surg Laparosc Endosc Percutan Tech. 2015;25:324–30.
Sucandy I, Chrestiana D, Bonanni F, et al. Gastroesophageal reflux symptoms after laparoscopic sleeve gastrectomy for morbid obesity. the importance of preoperative evaluation and selection. N Am J Med Sci. 2015;7:189–93.
Stenard F, Iannelli A. Laparoscopic sleeve gastrectomy and gastroesophageal reflux. World J Gastroenterol. 2015;21:10348–57.
Sheppard CE, Sadowski DC, de Gara CJ, et al. Rates of reflux before and after laparoscopic sleeve gastrectomy for severe obesity. Obes Surg. 2015;25:763–8.
Oor JE, Roks DJ, Unlu C, et al. Laparoscopic sleeve gastrectomy and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Surg. 2016;211(1):250–67.
Tolone S, Cristiano S, Savarino E, et al. Effects of omega-loop bypass on esophagogastric junction function. Surg Obes Relat Dis. 2016;12(1):62–9.
Hoshino M, Sundaram A, Mittal SK. Role of the lower esophageal sphincter on acid exposure revisited with high-resolution manometry. J Am Coll Surg. 2011;213:743–50.
Chen CL, Yi CH, Liu TT. Relevance of ineffective esophageal motility to secondary peristalsis in patients with gastroesophageal reflux disease. J Gastroenterol Hepatol. 2014;29:296–300.
Manabe N, Haruma K. Pathophysiology of gastroesophageal reflux disease from the viewpoint of esophageal motility. Nihon Shokakibyo Gakkai Zasshi. 2014;111:1923–32.
Martinucci I, de Bortoli N, Giacchino M, et al. Esophageal motility abnormalities in gastroesophageal reflux disease. World J Gastrointest Pharmacol Ther. 2014;5:86–96.
Rosenthal RJ, International Sleeve Gastrectomy Expert P, Diaz AA, et al. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8:8–19.
Author Contributions
FM, ST, and SR were responsible for the study concept and design, acquisition of the data, analysis and interpretation of the data, drafting the manuscript, and approval of the final version of the manuscript.
SM, EP, MR, GP, PJV, and AG were responsible for the acquisition of the data, analysis and interpretation of the data, drafting the manuscript, and approval of the final version of the manuscript.
ES and LD were responsible for the analysis and interpretation of the data, drafting of the manuscript, and approval of the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
FM was a consultant for Medtronic; ES and SR were consultants for Medtronic, Sandhill; and ST, LD, AG, SM, MR, GP, EP, and PJV declare no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human Rights
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Mion, F., Tolone, S., Garros, A. et al. High-resolution Impedance Manometry after Sleeve Gastrectomy: Increased Intragastric Pressure and Reflux are Frequent Events. OBES SURG 26, 2449–2456 (2016). https://doi.org/10.1007/s11695-016-2127-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2127-y



