Abstract
Background
Serum bile acids (BAs) are elevated after metabolic surgeries including Roux-en-Y gastric bypass (RYGB), ileal transposition (IT), and duodenal-jejunal bypass (DJB). Recently, BAs have emerged as a kind of signaling molecules, which can not only promote glucagon-like peptide-1 (GLP-1) secretion but can also regulate multiple enzymes involved in glucose metabolism. The aim of this study was to investigate whether expedited biliopancreatic juice flow to the distal gut contributes to the increased serum GLP-1 and BAs and benefits the diabetes control after DJB.
Methods
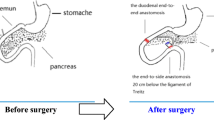
DJB, long alimentary limb DJB (LDJB), duodenal-jejunal anastomosis (DJA), and sham operation were performed in diabetic rats induced by high-fat diet (HFD) and low dose of streptozotocin (STZ). Body weight, food intake, oral glucose tolerance, insulin tolerance, glucose-stimulated insulin and GLP-1 secretion, fasting serum total bile acids (TBAs), and lipid profiles were measured at indicated time points.
Results
Compared with sham operation, DJA, DJB, and LDJB all achieved rapid and dramatic improvements in glucose tolerance and insulin sensitivity independently of food restriction and weight loss. DJB and LDJB-operated rats exhibited even better glucose tolerance, higher fasting serum TBAs, and higher glucose-stimulated GLP-1 secretion than the DJA group postoperatively. No difference was detected in insulin sensitivity and glucose-stimulated insulin secretion between DJA, DJB, and LDJB groups.
Conclusions
Expedited biliopancreatic juice flow to the distal gut was associated with augmented GLP-1 secretion and increased fasting serum TBA concentration, which may partly explain the metabolic benefits of DJB.






Similar content being viewed by others
References
Rubino F, Marescaux J. Effect of duodenal-jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg. 2004;239(1):1–11.
Jiao J, Bae EJ, Bandyopadhyay G, et al. Restoration of euglycemia after duodenal bypass surgery is reliant on central and peripheral inputs in Zucker fa/fa rats. Diabetes. 2013;62(4):1074–83.
Jurowich CF, Rikkala PR, Thalheimer A, et al. Duodenal-jejunal bypass improves glycemia and decreases SGLT1-mediated glucose absorption in rats with streptozotocin-induced type 2 diabetes. Ann Surg. 2013;258(1):89–97.
Rubino F, Forgione A, Cummings DE, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006;244(5):741–9.
Kindel TL, Yoder SM, Seeley RJ, et al. Duodenal-jejunal exclusion improves glucose tolerance in the diabetic, Goto-Kakizaki rat by a GLP-1 receptor-mediated mechanism. J Gastrointest Surg. 2009;13(10):1762–72.
Patti ME, Houten SM, Bianco AC, et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring). 2009;17(9):1671–7.
Cummings BP, Bettaieb A, Graham JL, et al. Bile-acid-mediated decrease in endoplasmic reticulum stress: a potential contributor to the metabolic benefits of ileal interposition surgery in UCD-T2DM rats. Dis Model Mech. 2013;6(2):443–56.
Han H, Hu C, Wang L, et al. Duodenal-jejunal bypass surgery suppresses hepatic de novo lipogenesis and alleviates liver fat accumulation in a diabetic rat model. Obes Surg. 2014;24(12):2152–60.
Houten SM, Watanabe M, Auwerx J. Endocrine functions of bile acids. EMBO J. 2006;25(7):1419–25.
Ma K, Saha PK, Chan L, et al. Farnesoid X receptor is essential for normal glucose homeostasis. J Clin Invest. 2006;116(4):1102–9.
Watanabe M, Houten SM, Wang L, et al. Bile acids lower triglyceride levels via a pathway involving FXR, SHP, and SREBP-1c. J Clin Invest. 2004;113(10):1408–18.
Thomas C, Gioiello A, Noriega L, et al. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab. 2009;10(3):167–77.
Schauer PR, Burguera B, Ikramuddin S, et al. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238(4):467–84. discussion 84–5.
Wang TT, Hu SY, Gao HD, et al. Ileal transposition controls diabetes as well as modified duodenal jejunal bypass with better lipid lowering in a nonobese rat model of type II diabetes by increasing GLP-1. Ann Surg. 2008;247(6):968–75.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56. 3.
Eissele R, Goke R, Willemer S, et al. Glucagon-like peptide-1 cells in the gastrointestinal tract and pancreas of rat, pig and man. Eur J Clin Investig. 1992;22(4):283–91.
Srinivasan K, Viswanad B, Asrat L, et al. Combination of high-fat diet-fed and low-dose streptozotocin-treated rat: a model for type 2 diabetes and pharmacological screening. Pharmacol Res. 2005;52(4):313–20.
Liu SZ, Sun D, Zhang GY, et al. A high-fat diet reverses improvement in glucose tolerance induced by duodenal-jejunal bypass in type 2 diabetic rats. Chin Med J. 2012;125(5):912–9.
Liu S, Zhang G, Wang L, et al. The entire small intestine mediates the changes in glucose homeostasis after intestinal surgery in Goto-Kakizaki rats. Ann Surg. 2012;256(6):1049–58.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222(3):339–50. discussion 50–2.
Thaler JP, Cummings DE. Minireview: hormonal and metabolic mechanisms of diabetes remission after gastrointestinal surgery. Endocrinology. 2009;150(6):2518–25.
Knop FK. Resolution of type 2 diabetes following gastric bypass surgery: involvement of gut-derived glucagon and glucagonotropic signalling? Diabetologia. 2009;52(11):2270–6.
Zhang SY, Sun XJ, Zheng JB, et al. Preserve common limb in duodenal-jejunal bypass surgery benefits rats with type 2-like diabetes. Obes Surg. 2014;24(3):405–11.
Baggio LL, Drucker DJ. Biology of incretins: GLP-1 and GIP. Gastroenterology. 2007;132(6):2131–57.
Drucker DJ. The role of gut hormones in glucose homeostasis. J Clin Invest. 2007;117(1):24–32.
Brubaker PL. The glucagon-like peptides: pleiotropic regulators of nutrient homeostasis. Ann N Y Acad Sci. 2006;1070:10–26.
Parker HE, Wallis K, le Roux CW, et al. Molecular mechanisms underlying bile acid-stimulated glucagon-like peptide-1 secretion. Br J Pharmacol. 2012;165(2):414–23.
Wu T, Bound MJ, Standfield SD, et al. Effects of taurocholic acid on glycemic, glucagon-like peptide-1, and insulin responses to small intestinal glucose infusion in healthy humans. J Clin Endocrinol Metab. 2013;98(4):E718–22.
Kohli R, Setchell KD, Kirby M, et al. A surgical model in male obese rats uncovers protective effects of bile acids post-bariatric surgery. Endocrinology. 2013;154(7):2341–51.
Pournaras DJ, Glicksman C, Vincent RP, et al. The role of bile after Roux-en-Y gastric bypass in promoting weight loss and improving glycaemic control. Endocrinology. 2012;153(8):3613–9.
Salinari S, le Roux CW, Bertuzzi A, et al. Duodenal-jejunal bypass and jejunectomy improve insulin sensitivity in Goto-Kakizaki diabetic rats without changes in incretins or insulin secretion. Diabetes. 2014;63(3):1069–78.
Speck M, Cho YM, Asadi A, et al. Duodenal-jejunal bypass protects GK rats from {beta}-cell loss and aggravation of hyperglycemia and increases enteroendocrine cells coexpressing GIP and GLP-1. Am J Physiol Endocrinol Metab. 2011;300(5):E923–32.
Steinert RE, Peterli R, Keller S, et al. Bile acids and gut peptide secretion after bariatric surgery: a 1-year prospective randomized pilot trial. Obesity (Silver Spring). 2013;21(12):E660–8.
Kohli R, Kirby M, Setchell KD, et al. Intestinal adaptation after ileal interposition surgery increases bile acid recycling and protects against obesity-related comorbidities. Am J Physiol Gastrointest Liver Physiol. 2010;299(3):G652–60.
Watanabe M, Houten SM, Mataki C, et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 2006;439(7075):484–9.
Kuipers F, Groen AK. FXR: the key to benefits in bariatric surgery? Nat Med. 2014;20(4):337–8.
Angelin B, Bjorkhem I, Einarsson K, et al. Hepatic uptake of bile acids in man. Fasting and postprandial concentrations of individual bile acids in portal venous and systemic blood serum. J Clin Investig. 1982;70(4):724–31.
Mencarelli A, Renga B, D’Amore C, et al. Dissociation of intestinal and hepatic activities of FXR and LXRα supports metabolic effects of terminal ileum interposition in rodents. Diabetes. 2013;62(10):3384–93.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (no. 81270888/H0713, no. 81370496/H0308, no. 81300286/H0308), Natural Science Foundation of Shandong Province grants (no. ZR2009CM051), and the Taishan Scholar Foundation.
Conflict of Interest
We declare that all authors have no conflict of interest.
Statement of Informed Consent
Does not apply.
Statement of Human and Animal Rights
All applicable institutional and national guidelines for the care and use of animals were followed.
Author information
Authors and Affiliations
Corresponding author
Additional information
Haifeng Han and Lei Wang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Han, H., Wang, L., Du, H. et al. Expedited Biliopancreatic Juice Flow to the Distal Gut Benefits the Diabetes Control After Duodenal-Jejunal Bypass. OBES SURG 25, 1802–1809 (2015). https://doi.org/10.1007/s11695-015-1633-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1633-7