Abstract
Introduction
In 2006, the Centers for Medicare and Medicaid Services (CMS) issued a national coverage decision restricting bariatric surgery to designated centers of excellence (COE). Although prior studies show mixed results on complications and reoperations, no prior studies evaluated whether this policy reduced spending for bariatric surgery. We sought to determine whether the coverage restriction to COE-designated hospitals was associated with lower payments from CMS.
Methods
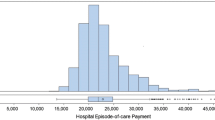
We utilized national Medicare claims data to examine 30-day episode payments for patients who underwent bariatric surgery from 2003 to 2010 (n = 72,117 patients). We performed an interrupted time series analysis, adjusting for patient factors, preexisting temporal trends, and changes in procedure type, to determine whether the 2006 coverage decision was associated with lower Medicare payments above and beyond any existing secular trends. For these analyses, we included payments for the index hospitalization, readmissions, physician services, and post-discharge ancillary care.
Results
After accounting for patient factors, preexisting temporal trends, and changes in procedure type, there were no statistically significant improvements in episode payments after (US$14,720) vs before (US$14,283) the coverage decision (+US$437, 95 % CI, −US$10 to +US$883). In a direct assessment of payments for COE-designated hospitals (US$14,481) vs non-COE-designated hospitals (US$14,756), no significant differences in episode payments were found (−US$275, 95 % CI, −US$696 to +US$145).
Conclusions
We found no significant reductions in 30-day episode payments after vs before restricting coverage to COE-designated hospitals. Center of excellence status is not a proxy for savings to the healthcare system.

Similar content being viewed by others
References
Hollenbeak CS, Rogers AM, Barrus B, et al. Surgical volume impacts bariatric surgery mortality: a case for centers of excellence. Surgery 2008; 144(5):736-43.
Nguyen NT, Paya M, Stevens CM, et al. The Relationship Between Hospital Volume and Outcome in Bariatric Surgery at Academic Medical Centers. Transactions of the … Meeting of the American Surgical Association 2004; CXXII(&NA;):184-192.
Pratt GM, McLees B, Pories WJ. The ASBS Bariatric Surgery Centers of Excellence program: a blueprint for quality improvement. Surg Obes Relat Dis 2006; 2(5):497-503; discussion 503.
National Coverage Determination (NCD) for Bariatric Surgery for Treatment of Morbid Obesity (100.1) [Centers for Medicare and Medicaid Services web site]. Available at: https://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=57&bc=AgAAgAAAAAAA&ncdver=3. Accessed March 1, 2015.
Schirmer B, Jones DB. The American College of Surgeons Bariatric Surgery Center Network: establishing standards. Bull Am Coll Surg 2007; 92(8):21-7.
Resources for Optimal Care of the Metabolic and Bariatric Surgery Patient [Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program web site]. 2014. Available at: https://www.facs.org/~/media/files/quality%20programs/bariatric/resourcesforoptimalcareofthembspatient.ashx. Accessed March 1, 2015.
Dimick JB, Nicholas LH, Ryan AM, et al. Bariatric surgery complications before vs after implementation of a national policy restricting coverage to centers of excellence. JAMA 2013; 309(8):792-9.
Dimick JB, Osborne NH, Nicholas L, et al. Identifying high-quality bariatric surgery centers: hospital volume or risk-adjusted outcomes? J Am Coll Surg 2009; 209(6):702-6.
Flum DR, Kwon S, MacLeod K, et al. The use, safety and cost of bariatric surgery before and after Medicare's national coverage decision. Ann Surg 2011; 254(6):860-5.
Kruger RS, Pricolo VE, Streeter TT, et al. A Bariatric Surgery Center of Excellence: Operative Trends and Long-Term Outcomes. J Am Coll Surg 2014.
Livingston EH. Bariatric surgery outcomes at designated centers of excellence vs nondesignated programs. Arch Surg 2009; 144(4):319-25; discussion 325.
Birkmeyer JD, Gust C, Dimick JB, et al. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg 2012; 255(1):1-5.
Eappen S, Lane BH, Rosenberg B, et al. Relationship between occurrence of surgical complications and hospital finances. JAMA 2013; 309(15):1599-606.
Scally CP, Thumma JR, Birkmeyer JD, et al. Impact of Surgical Quality Improvement on Payments in Medicare Patients. Ann Surg 2014.
Birkmeyer JD, Skinner JS, Wennberg DE. Will volume-based referral strategies reduce costs or just save lives? Health Aff (Millwood) 2002; 21(5):234-41.
Englesbe MJ, Dimick JB, Fan Z, et al. Case mix, quality and high-cost kidney transplant patients. Am J Transplant 2009; 9(5):1108-14.
Ho V, Aloia T. Hospital volume, surgeon volume, and patient costs for cancer surgery. Med Care 2008; 46(7):718-25.
Birkmeyer JD, Gust C, Baser O, et al. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res 2010; 45(6 Pt 1):1783-95.
Medicare Approved Facilities: Bariatric Surgery [Centers for Medicare and Medicaid Services web site]. Available at: https://www.cms.gov/Medicare/Medicare-General-Information/MedicareApprovedFacilitie/Bariatric-Surgery.html. Accessed February 1, 2014.
Gottlieb DJ, Zhou W, Song Y, et al. Prices don't drive regional Medicare spending variations. Health Aff (Millwood) 2010; 29(3):537-43.
Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr 2013; 13(6 Suppl):S38-44.
Campbell SM, Reeves D, Kontopantelis E, et al. Effects of pay for performance on the quality of primary care in England. N Engl J Med 2009; 361(4):368-78.
Ryan AM, Nallamothu BK, Dimick JB. Medicare's public reporting initiative on hospital quality had modest or no impact on mortality from three key conditions. Health Aff (Millwood) 2012; 31(3):585-92.
Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care 1998; 36(1):8-27.
Reames BN, Finks JF, Bacal D, et al. Changes in bariatric surgery procedure use in Michigan, 2006-2013. JAMA 2014; 312(9):959-61.
Share DA, Campbell DA, Birkmeyer N, et al. How a regional collaborative of hospitals and physicians in Michigan cut costs and improved the quality of care. Health Aff (Millwood) 2011; 30(4):636-45.
Bloor K, Freemantle N, Khadjesari Z, et al. Impact of NICE guidance on laparoscopic surgery for inguinal hernias: analysis of interrupted time series. BMJ 2003; 326(7389):578.
Serumaga B, Ross-Degnan D, Avery AJ, et al. Effect of pay for performance on the management and outcomes of hypertension in the United Kingdom: interrupted time series study. BMJ 2011; 342:d108.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Dr. Scally is supported by a grant from the National Cancer Institute (5T32CA009672-23). This study was supported by a grant to Dr. Dimick from the National Institute of Aging (R01AG039434). The views expressed herein do not necessarily represent the views of the US Government.
Conflict of interest
Dr. Dimick has no conflicts of interest. He has one disclosure: he is a consultant and has an equity interest in ArborMetrix, Inc, which provides software and analytics for measuring hospital quality and efficiency. The company had no role in the study herein. Drs. Scally and Shih and Mrs. Thumma have no relevant disclosures or conflicts of interest.
Rights and permissions
About this article
Cite this article
Scally, C.P., Shih, T., Thumma, J.R. et al. Impact of a National Bariatric Surgery Center of Excellence Program on Medicare Expenditures. J Gastrointest Surg 20, 708–714 (2016). https://doi.org/10.1007/s11605-015-3027-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-3027-5