Abstract
Purpose
The authors sought to evaluate the potential of magnetic resonance (MR) imaging with superparamagnetic iron oxide (SPIO) contrast material for identifying, characterising and differentiating dysplastic nodules (DN) and hepatocellular carcinoma (HCC) in the cirrhotic liver by correlating the results with pathological findings on the explanted liver.
Material and methods
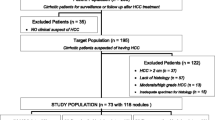
MR imaging was used to study the liver of 400 cirrhotic patients awaiting liver transplantation, 31 of whom were selected to receive a liver. Of these 31 patients, we included in the study 22 patients (mean age 53 years; range 46–57 years) who underwent liver transplantation within 12–24 h after MR examination. Patients were studied with a 1.5-T device, and scans were acquired before and after the administration of paramagnetic contrast material. For every lesion, we recorded signal intensity on unenhanced baseline T1- and T2-weighted images and enhancement pattern after SPIO administration. Histological examination of the entire liver provided the definitive diagnosis of the lesions.
Results
Histological examination identified 59 lesions: 14 HCC, 4 HCC-DN, 39 DN, and 2 cystoadenomas. Among the 14 HCC, three were well differentiated, eight were moderately differentiated and three were poorly differentiated. Of the 39 DN, 28 were low-grade and 11 high-grade lesions. Unenhanced baseline MR imaging correctly identified and characterised 20 lesions, equal to 33.90% of all lesions: 6 HCC, 12 DN and 2 DN with a subfocus of HCC. SPIO-enhanced MR imaging showed greater sensitivity detecting and characterising 45 lesions, equal to 76.27% of all lesions identified at histology: 14 HCC, 27 DN and 4 DN with subfocus of HCC. SPIO administration improved the sensitivity of MR imaging in lesion detection and characterisation by 42.37%. False negative results with SPIO-enhanced MR imaging occurred in 12 DN (31%), which histological examination revealed to be low-grade DN with a diameter <1 cm.
Conclusions
SPIO-enhanced MR imaging proved to be of value in detecting and characterising lesions in the cirrhotic liver, allowing differentiation of DN from HCC and providing an early diagnosis of neoplastic degeneration of DN.
Riassunto
Obiettivo
Obiettivo di questo studio è stato valutare le potenzialità della risonanza magnetica (RM) eseguita con mezzo di contrasto (MdC) superparamagnetico (superparamagnetic iron oxide particles, SPIO) nell’identificazione, caratterizzazione e diagnosi differenziale tra noduli displasici (ND) ed epatocarcinoma (HCC) nel fegato cirrotico, confrontando i risultati della RM con quelli dell’esame anatomo-patologico eseguito su fegato espiantato.
Materiali e metodi
Abbiamo studiato con RM il fegato di 400 pazienti cirrotici in attesa di trapianto, 31 dei quali selezionati per reperimento d’organo da trapiantare. Dei 31 pazienti selezionati per il trapianto d’organo, sono stati inclusi nello studio 22 pazienti, di età media di 53 anni (range 46–57 anni), sottoposti a trapianto di fegato a distanza di circa 12–24 ore dall’esecuzione dell’esame RM. I pazienti inclusi nello studio sono stati sottoposti ad esame RM con un apparecchio da 1,5 T. Sono state eseguite scansioni prima e dopo somministrazione endovenosa di MdC SPIO. Per ogni lesione identificata è stata indicata l’intensità di segnale nelle sequenze di base pesate in T1 e in T2 ed il comportamento dopo iniezione di MdC SPIO. La diagnosi definitiva delle lesioni è stata effettuata con l’esame istologico di tutto il fegato espiantato.
Risultati
Con l’esame istologico sono state identificate 59 lesioni: 14 HCC, 4 HCC-ND, 39 ND, 2 cistoadenomi. Dei 14 HCC, 3 sono risultati ben differenziati, 8 moderatamente differenziati, 3 scarsamente differenziati. Dei 39 ND, 28 erano a basso grado di malignità e 11 ad alto grado di malignità. Con l’esame RM di base abbiamo identificato e caratterizzato correttamente 20 lesioni, pari al 33,90% delle lesioni complessivamente individuate, di cui 6 HCC, 12 ND e 2 ND con foci di HCC. L’esame RM, eseguito dopo somministrazione di MdC SPIO, ha mostrato una maggiore sensibilità identificando e caratterizzando complessivamente 45 lesioni, pari al 76,27% delle lesioni totali individuate con l’esame istologico: 14 HCC, 27 ND e 4 ND con foci di HCC. Dopo la somministrazione di MdC SPIO la sensibilità della RM nella identificazione e caratterizzazione delle lesioni è aumentata rispetto alle immagini di base del 42,37%. I falsi negativi con la RM-SPIO sono stati 12 noduli displasici, pari al 31%, che all’esame istologico sono risultati essere ND a basso grado di malignità e con diametro inferiore al cm.
Conclusioni
La RM con utilizzo di MdC SPIO, nella nostra esperienza è risultata utile nella identificazione e caratterizzazione delle lesioni epatiche nel fegato cirrotico mostrandosi in grado di differenziare i noduli displasici dagli HCC e ha consentito una diagnosi precoce della trasformazione carcinomatosa dei noduli displasici.
Similar content being viewed by others
References/Bibliografia
Brown JJ, Naylor MJ, Yagan N (1997) Imaging of hepatic cirrhosis. Radiology 202:1–16
El-Serag HB, Mason AC (1999) Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med 340:745–750
Colombo M, de Franchis R, Del Ninno E et al (1991) Hepatocellular carcinoma in Italian patients with cirrhosis. N Engl J Med 325:675–680
Lencioni R, Bartolozzi C, Caramella D, Di Coscio G (1993) Management of adenomatous hyperplastic nodules in the cirrhotic liver: US follow-up or percutaneous alcohol ablation? Abdom Imaging 18:50–55
Figueras J, Jaurrieta E, Valls C et al (2000) Resection or transplantation for hepatocellular carcinoma in cirrhotic patients: outcomes based on indicated treatment strategy. J Am Coll Surg 190:580–587
Trojan J, Raedle J, Zeuzem S (1998) Serum tests for diagnosis and follow-up of hepatocellular carcinoma after treatment. Digestion 59(suppl):72–74
Theise ND, Fiel IM, Hytiroglou P et al (1995) Macroregenerative nodules in cirrhosis are not associated with elevated serum or stainable tissue alphafetoprotein. Liver 15:30–34
Bennett GL, Krinsky GA, Abitbol RJ et al (2002) Sonographic detection of hepatocellular carcinoma and dysplastic nodules in cirrhosis: correlation of pretransplantation sonography and liver explant pathology in 200 patients. AJR Am J Roentgenol 179:75–80
Szklaruk J, Silverman PM, Charnsangavej C (2003) Imaging in diagnosis, staging, treatment, and surveillance of hepatocellular carcinoma. AJR Am J Roentgenol 180:441–454
Lim JH, Kim CK, Lee WJ et al (2000) Detection of hepatocellular carcinomas and dysplastic nodules in cirrhotic livers: accuracy of helical CT in transplant patients. AJR Am J Roentgenol 175:693–698
Pauleit D, Textor J, Bachmann R et al (2002) Hepatocellular carcinoma: detection with gadolinium- and ferumoxides-enhanced MR imaging of the liver. Radiology 222:73–80
Krinsky GA, Lee VS (2000) MR imaging of cirrhotic nodules. Abdom Imaging 25:471–482
Hagspiel KD, Neidl KFW, Eichenberger AC et al (1995) Detection of liver metastases: comparison of superparamagnetic iron oxide-enhanced and unenhanced MR imaging at 1.5T with dynamic CT, intraoperative US and percutaneous US. Radiology 196:471–478
Seneterre E, Taourel P, Bouvier Y et al (1996) Detection of hepatic metastasis: ferumoxidesenhanced MR imaging versus unenhanced MR imaging ad CT during arterialportography. Radiology 200:785–792
Sugihara S, Suto Y, Kamba M, Ogawa T (2001) Comparison of various techniques of iron oxide-enhanced breath-hold MR imaging of hepatocellular carcinoma. Clin Imaging 25:104–109
Suto Y, Shimatani Y (1995) Dual contrast magnetic resonance imaging with combined used of positive and negative contrast agent in human hepatocellular carcinoma. BJR 68:116–120
Kim SH, Choi D, Kim SH et al (2005) Ferucarbotran-enhanced MRI versus triple phase MDCT for the peroperative detection of hepatocelular carcinoma. AJR Am J Roentgenol 184:1069–1076
Hayashi M, Matsui O, Ueda K et al (2002) Progression to hypervascular hepatocellular carcinoma: correlation with intranodular blood supply evaluated with CT during intraarterial injection of contrast material. Radiology 225:143–149
Matsui O, Ueda K, Kobayashi S et al (2002) Intra- and perinodular hemodynamics of hepatocellular carcinoma: CT observation during intra-arterial contrast injection. Abdom Imaging 27:147–156
Efremidis SC, Hytiroglou P (2002) The multistep process of hepatocarcinogenesis in cirrhosis with imaging correlation. Eur Radiol 12:753–764
International Working Party (1995) Terminology of nodular hepatocellular lesions. Hepatology 22:983–993
Liver Cancer Study Group of Japan (1992) The general rules for the clinical and pathological study of primary liver cancer. Kanehara Publishers, Tokyo
Iannaccone R, Laghi A, Catalano C et al (2004) Lesioni focali nel paziente cirrotico: valutazione con TC spirale multistrato. Radiol Med 107:304–316
Earls JP, Theise ND, Weinreb JC et al (1996) Dysplastic nodules and hepatocellular carcinoma: thin-section MR imaging of explanted cirrhotic livers with pathologic correlation. Radiology 201:207–214
Lim JH, Choi BI (2002) Dysplastic nodules in liver cirrhosis: imaging. Abdom Imaging 27:117–128
Macarini L, Marini S, Murrone M (2004) Alterazioni della captazione e della distribuzione epatica dei mezzi di contrasto superparamagnetici organospecifici per risonanza magnetica. Rilievo clinico e classificazione sulla base del meccanismo patogenetico. Radiol Med 108:159–171
Catalano O, Nunziata A, Lobianco R, Siani A (2005) Real-time harmonic contrast material-specific US of focal liver lesions. Radiographics 25:333–349
Valls C, Cos M, Figueras J et al (2004) Pretransplantation diagnosis and staging of hepatocellular carcinoma in patients with cirrhosis: value of dual-phase helical CT. AJR Am J Roentgenol 182:1011–1017
Hayashi M, Matsui O, Ueda K et al (1999) Correlation between the blood supply and grade of malignancy of hepatocellular nodules associated with liver cirrhosis: evaluation by CT during intraarterial injection of contrast medium. AJR Am J Roentgenol 172:969–976
Krinsky GA, Lee VS, Theise ND (2000) Focal lesions in the cirrhotic liver: high resolution ex vivo MRI with pathologic correlation. J Comput Assist Tomogr 24:189–196
Matsuo M, Kanematsu M, Itoh K et al (2001) Detection of malignant hepatic tumors: comparison of gadolinium and ferumoxides-enhanced MR imaging. AJR Am J Roentgenol 177:637–643
Kim MJ, Kim JH, Chung JJ et al (2003) Focal hepatic lesions: detection and characterization with combination gadolinium- and superparamagnetic iron oxide-enhanced MR imaging. Radiology 228:719–726
Krinsky G A, Lee VS, Theise ND et al (2001) Hepatocellular carcinoma and dysplastic nodules in patients with cirrhosis: prospective diagnosis with MR imaging and explantation correlation. Radiology 219:445–454
Di Cesare E, Cariello G, Barile A et al (2000) Risonanza magnetica delle lesioni focali epatiche: valutazione contrastografica dinamica con gadolinio vs mezzo di contrasto epatospecifico reticolo-endoteliale. Radiol Med 100:245–250
Paley MR, Mergo PJ, Torres GM, Ros PR (2000) Characterization of focal hepatic lesions with ferumoxides.enhanced T2-weighted MR imaging. AJR Am J Roentgenol 175:159–163
Stark DD, Weissleder R, Elizondo G et al (1988) Superparamagnetic iron oxide: clinical application as a contrast agent for MR imaging of the liver. Radiology 162:297–301
Kang BK, Lim JH, Kim SH et al (2003) Preoperative depiction of hepatocellular carcinoma: ferumoxides-enhanced MR imaging versus triple-phase helical CT. Radiology 226:79–85
Macarini L, Marini S, Milillo P et al (2006) RM epatica a doppio contrasto (RM-DC) nello studio del fegato cirrotico: utilità della somministrazione di Gd-DTPA come completamento di esami in cui siano presenti alterazioni di captazione e distribuzione epatiche (ACDE) del Mdc SPIO e nell’identificazione e caratterizzazione delle lesioni focali. Radiol Med 111:1087–1102
Tanaka M, Nakashima O, Wada Y et al (1996) Pathomorphological study of Kupffer cells inn hepatocellular carcinoma and hyperplastic nodular lesions in the liver. Hepatology 24:807–812
Lim JH, Choi D, Cho SK et al (2001) Conspicuity of hepatocellular nodular lesion in cirrhotic liver at ferumoxides-enhanced MR imaging: importance of Kupffer cell number. Radiology 669–676
Tang Y, Yaamashita Y, Arakaawa A et al (1999) Detection of hepatocellular carcinoma arising in cirrhotic livers: comparision of gadolinium and ferumoxides-enhanced MR imaging. AJR Am J Roentgenol 172:1547–1554
Clement O, Frija G, Chambon C et al (1991) Liver tumors in cirrhosis: experimental study with SPIOenhanced and irone oxide-enhanced MR imaging. Radiology 180:31–36
Yamashita Y, Yamamoto H, Hirai A et al (1996) MR imaging enhancement with superparamagnetic iron oxide in chronic liver disease: influente of the liver dysfunction and parenchymal pathology. Abdom Imaging 21:318–323
Lucidarme O, Baleston F, Caldi M et al (2002) Non-invasive detection of liver fibrosis: is superparamagnetic iron oxide particle-enhanced MR imaging a contributive technique. Eur Radiol 13:467–474
Tonan T, Fujimoto K, Azuma S et al (2007) Evaluation of small (<2 cm) dysplastic nodules and well differentiated hepatocellular carcinomas with ferucarbotran-enhanced MRI in a 1.0-T MRI unit: utility of T2*-weighted gradient echo sequences with an intermediate echo-time. Eur J Radiol 64:133–139
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Macarini, L., Milillo, P., Cascavilla, A. et al. MR characterisation of dysplastic nodules and hepatocarcinoma in the cirrhotic liver with hepatospecific superparamagnetic contrast agents: pathological correlation in explanted livers. Radiol med 114, 1267–1282 (2009). https://doi.org/10.1007/s11547-009-0464-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-009-0464-9