Abstract
Background
Fecal microbiota transplantation (FMT) is emerging as an effective therapy for the treatment of recurrent Clostridium difficile infection (RCDI). Selecting an appropriate donor is vital to the success of FMT. However, the relationship between age of donors and the efficacy of FMT has not been examined to date. The aim of this study was to examine the effect of age of healthy donors on their fecal microbiota and assess the impact of these changes on the clinical efficacy of FMT.
Materials and Methods
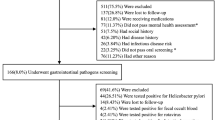
This IRB-approved prospective study enrolled donors who were deemed healthy for FMT after careful detailed screening for infectious diseases per institutional protocol. The study was conducted between January 2011 and October 2014. Fecal samples were processed and analyzed using 16S rRNA gene amplicon sequencing. Differences in relative abundance and diversity of the donor fecal microbiota were analyzed in donors above and below 60 years of age. Effect of fecal microbiota from donors of different age groups on the efficacy of FMT was also evaluated.
Results
Twenty-eight healthy human subjects from ages 20–82 years were enrolled as donors for FMT. All patients receiving FMT from their respective donors had resolution of RCDI symptoms and had a negative C. difficile toxin test 4–12 weeks after FMT. Genomic analysis showed that the relative abundance of phylum Actinobacteria and family Bifidobacteriaceae was reduced in the donors ≥60 years of age (p < 0.05). However, Bacteroidetes-to-Fermicutes ratio did not demonstrate a significant change between the two groups. Furthermore, microbial diversity did not change significantly with advancing age.
Conclusion
These observations suggest that aging in healthy donors is associated with compositional alterations in the fecal microbiome without change in the overall microbial diversity. These changes do not seem to affect the clinical efficacy of FMT in RCDI patients over 12 months.



Similar content being viewed by others
Abbreviations
- CDI:
-
Clostridium difficile infection
- FMT:
-
Fecal microbiota transplantation
- GI:
-
Gastrointestinal
- RCDI:
-
Recurrent Clostridium difficile infection
References
Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372:825–834.
Kelly CP, LaMont JT. Clostridium difficile—more difficult than ever. N Engl J Med. 2008;359:1932–1940.
McFarland LV, Elmer GW, Surawicz CM. Breaking the cycle: treatment strategies for 163 cases of recurrent Clostridium disease. Am J Gastroenterol. 2002;97:1769–1775.
Gough E, Shaikh H, Manges AR. Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection. Clin Infect. 2011;53:994–1002.
Dutta SK, Girotra M, Garg S, et al. Efficacy of combined jejunal and colonic fecal microbiota transplantation for recurrent Clostridium difficile infection. Clin Gastroenterol Hepatol. 2014;12:1572–1576. doi:10.1016/j.cgh.2013.12.032.
Brandt LJ, Borody TJ, Campbell J. Endoscopic fecal microbiota transplantation: “first-line” treatment for severe Clostridium difficile infection? J Clin Gastroenterol. 2011;45:655–657.
van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368:407–415.
Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431–455.
Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478–498; quiz 99.
Caporaso JG, Kuczynski J, Stombaugh J, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7:335–336.
Nelson MC, Morrison HG, Benjamino J, et al. Analysis, optimization and verification of Illumina-generated 16S rRNA gene amplicon surveys. PLoS One. 2014;9:e94249.
White JR, Nagarajan N, Pop M. Statistical methods for detecting differentially abundant features in clinical metagenomic samples. PLoS Comput Biol. 2009;5:e1000352.
Ventura M, O’Flaherty S, Claesson MJ, et al. Genome-scale analyses of health-promoting bacteria: probiogenomics. Nat Rev Microbiol. 2009;7:61–71.
Makivuokko H, Tiihonen K, Tynkkynen S, et al. The effect of age and non-steroidal anti-inflammatory drugs on human intestinal microbiota composition. Br J Nutr. 2010;103:227–234.
Biagi E, Nylund L, Candela M, et al. Through ageing, and beyond: gut microbiota and inflammatory status in seniors and centenarians. PLoS One. 2010;5:e10667.
Mueller S, Saunier K, Hanisch C, et al. Differences in fecal microbiota in different European study populations in relation to age, gender, and country: a cross-sectional study. Appl Environ Microbiol. 2006;72:1027–1033.
Mariat D, Firmesse O, Levenez F, et al. The firmicutes/bacteroidetes ratio of the human microbiota changes with age. BMC Microbiol. 2009;9:123.
Claesson MJ, Cusack S, O’Sullivan O, et al. Composition, variability, and temporal stability of the intestinal microbiota of the elderly. Proc Natl Acad Sci USA. 2011;108:4586–4591.
Woodmansey EJ, McMurdo ME, Macfarlane GT, et al. Comparison of compositions and metabolic activities of fecal microbiotas in young adults and in antibiotic-treated and non-antibiotic-treated elderly subjects. Appl Environ Microbiol. 2004;70:6113–6120.
Hopkins MJ, Sharp R, Macfarlane GT. Variation in human intestinal microbiota with age. Dig Liver. 2002;34:S12–S18.
Zwielehner J, Liszt K, Handschur M, et al. Combined PCR-DGGE fingerprinting and quantitative-PCR indicates shifts in fecal population sizes and diversity of Bacteroides, bifidobacteria and Clostridium cluster IV in institutionalized elderly. Exp Gerontol. 2009;44:440–446.
Ivanov D, Emonet C, Foata F, et al. A serpin from the gut bacterium Bifidobacterium longum inhibits eukaryotic elastase-like serine proteases. J Biol Chem. 2006;281:17246–17252.
Ouwehand AC, Isolauri E, Kirjavainen PV, et al. Adhesion of four Bifidobacterium strains to human intestinal mucus from subjects in different age groups. FEMS Microbiol Lett. 1999;172:61–64.
Matthew JH, Alexa RW, Michael JS, et al. Standardized frozen preparation for transplantation of fecal microbiota for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012;107:761–767. doi:10.1038/ajg.2011.482.
Acknowledgments
The authors thank the following people for their time and contribution toward our study: (1) Ms. Tami Parisi, Ms. Kristen Reuter, Ms. Kenda Koerner, and Ms. Barbara Bodner in the Department of Pathology, Sinai Hospital, Baltimore, for their assistance in preparing fecal samples into filtrate for administration during the FMT procedure; (2) Ms. Dayna Sherba in the Division of Gastroenterology, Sinai Hospital, Baltimore, for helping the study team with procedure scheduling and managing follow-up visits of our patients undergoing FMT; (3) Dr. Deepa Dutta, Director of the Department of Microbiology and Pathology, Sinai Hospital, for the patient’s personnel and resource management in preparation of fecal filtrates for administration during the present study; (4) Nursing staff at the Gastrointestinal Diagnostic Center at Sinai Hospital, especially Ms. Laura Thomson and Ms. Denni Arrup, for their excellent patient care and collection of fecal specimens.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Anand, R., Song, Y., Garg, S. et al. Effect of Aging on the Composition of Fecal Microbiota in Donors for FMT and Its Impact on Clinical Outcomes. Dig Dis Sci 62, 1002–1008 (2017). https://doi.org/10.1007/s10620-017-4449-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4449-6