Abstract
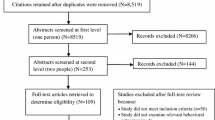
This systematic review examines the overall efficacy of HIV behavioral interventions designed to reduce HIV risk behaviors or incident sexually transmitted diseases (STDs) among Hispanics residing in the United States or Puerto Rico. Data from 20 randomized and nonrandomized trials (N = 6,173 participants) available through January 2006 were included in this review. Interventions successfully reduced the odds of unprotected sex and number of sex partners, increased the odds of condom use, and decreased the odds of acquiring new STD infections. Interventions successful in reducing the odds of any sex risk behavior used non-peer deliverers; included ≥4 intervention sessions; taught condom use or problem solving skills; or addressed barriers to condom use, sexual abstinence, or peer norms. Interventions that included the Hispanic cultural belief of machismo or those developed based on ethnographic interviews were successful in reducing the odds of sex risk behaviors among non-drug users. Interventions targeting injection drug users (IDUs; N = 3,569) significantly reduced the odds of injection drug use and the odds of sharing cotton or cookers, but did not significantly reduce the odds of engaging in risky sex behavior or needle sharing. Further development of culturally appropriate HIV prevention interventions for Hispanic populations, particularly men and persons living with HIV, are warranted.

Similar content being viewed by others
Notes
Requests were sent by e-mail to 23 principal investigators of intervention studies that focused on Hispanics identified through our search of conference abstracts and referrals from experts. Eighteen authors (78%) responded to our requests by either providing additional information about their study design (five authors), sending summary data to facilitate calculation of effect sizes (11 authors), or supplying the names of additional researchers (two authors). Four authors submitted in press intervention evaluation reports to the PRS Team for review and potential inclusion in this review (Carballo-Diéguez et al., 2005; Peragallo et al., 2005; Robles et al., 2004; Villarruel, Jemmott, & Jemmott, 2006).
References
References marked with an asterisk (*) indicate studies included in the meta-analysis.
Albarracin, D., Kumkale, G. T., & Johnson, B. T. (2004). Influences of social power and normative support on condom use decisions: a research synthesis. AIDS Care, 16, 700–723.
Amaro, H., & Raj, A. (2000). On the margin: power and women’s HIV risk reduction strategies. Sex Roles, 42(7–8), 723–749.
Anderson, R. N., & Smith, B. L. (2005). Deaths: Leading causes for 2002. National Vital Statistics Reports, 53(17), 1–90.
Arreola, S. G., Neilands, T. B., Pollack, L. M., Paul, J. P., & Catania, J. A. (2005). Higher prevalence of childhood sexual abuse among Latino men who have sex with men than non-Latino men who have sex with men: Data from the Urban Men’s Health Study. Child Abuse & Neglect, 29(3), 285–290.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall.
Bernal, G., Bonilla, J., & Bellido, C. (1995). Ecological validity and cultural sensitivity for outcome research: Issues for the cultural adaptation and development of psychosocial treatments for Hispanics. Journal of Abnormal Child Psychology, 23(1), 67–82.
Birkel, R. C., Golaszewski, T., Koman, J. J. III, Singh, B. K., Catan, V., & Souply, K. (1993). Findings from the Horizontes Acquired Immune Deficiency Syndrome Education Project: The impact of indigenous outreach workers as change agents for injection drug users. Health Education Quarterly, 20, 523–538.
Campo, R. E., Alvarez, D., Santos, G., & Latorre, J. (2005). Antiretroviral treatment considerations in Latino patients. AIDS Patient Care and STDs, 19(6), 366–374.
*Carballo-Diéguez, A., Dolezal, C., Leu, C. S., Nieves, L., Díaz, F., Decena, C., & Balan, I. (2005). A randomized controlled trial to test an HIV-prevention intervention for Latino gay and bisexual men: Lessons learned. AIDS Care, 17, 314–328.
Cargill, V. A., & Stone, V. E. (2005). HIV/AIDS: A minority health issue. Medical Clinics of North America, 89, 895–912.
*Castro, F. G., & Tafoya-Barraza, H. M. (1997). Treatment issues with Latinos addicted to cocaine and heroin. In: J. G. García, & M. C. Zea (Eds.), Psychological interventions and research with Latino populations (pp. 191–216). Boston, MA: Allyn and Bacon.
Centers for Disease Control and Prevention. (2003a). Advancing HIV prevention: New strategies for a changing epidemic-United States, 2003. Morbidity and Mortality Weekly Report, 52, 329–332.
Centers for Disease Control and Prevention. (2003b). Late versus early testing of HIV—16 sites, United States, 2000–2003. Morbidity and Mortality Weekly Report, 52(25), 581–586.
Centers for Disease Control and Prevention (2004a). Evaluation of innovative human immunodeficiency virus (HIV) prevention interventions for high-risk minority populations [Funding Opportunity Number PA 04249]. Federal Register, 69(134), 42183–42190.
Centers for Disease Control and Prevention. (2004b). HIV/AIDS surveillance report, 2003 (Vol. 15). Atlanta, GA: Centers for Disease Control and Prevention.
Centers for Disease Control and Prevention (2004c). Sexually transmitted disease surveillance, 2003. Atlanta, GA: U.S. Department of Health and Human Services.
Centers for Disease Control and Prevention. (2005). HIV/AIDS surveillance report, 2004 (Vol. 16). Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
Cervantes, R. C., Kappos, B., Duenas, N., & Arellano, D. (2003). Culturally focused HIV prevention and substance abuse treatment for Hispanic women. Addictive Disorders and their Treatment, 2, 69–77.
*Colón, H. M., Robles, R. R., Freeman, D., & Matos, T. (1993). Effects of a HIV risk reduction education program among injection drug users in Puerto Rico. Puerto Rico Health Sciences Journal, 12, 27–34.
Copenhaver, M., Johnson, B. T., Lee, I. C., Harman, J. J., Carey, M. P., & the SHARP Research Team (in press). Behavioral HIV risk reduction among people who inject drugs: meta-analytic evidence of efficacy. Journal of Substance Abuse Treatment.
Coyle, K. K., Kirby, D. B., Marin, B. V., Gomez, C. A., & Gregorich, S. E. (2004). Draw the line/respect the line: A randomized trial of a middle school intervention to reduce sexual risk behaviors. American Journal of Public Health, 94, 843–851.
Crepaz, N., Lyles, C. M., Wolitski, R. J., Passin, W. F., Rama, S. M., Herbst, J. H., Purcell, D. W., Malow, R. M., Stall, R., & the HIV/AIDS Prevention Research Synthesis Team (2006). Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS, 20, 143–157.
Darbes, L. A., Kennedy, G. E., Peersman, G., Zohrabyan, L., & Rutherford, G. W. (2002). Systematic review of HIV behavioral prevention research in Latinos. Retrieved August 4, 2005, from http://hivinsite.ucsf.edu/InSite?page=kb-07&doc=kb-07-04-11.
Deren, S., Shedlin, M., Decena, C. U., & Mino, M. (2005). Research challenges of the study of HIV/AIDS among migrant and immigrant Hispanic populations in the United States. Journal of Urban Health, 82(Suppl. 3(2)), III13–III25.
Des Jarlais, D. C., Lyles, C. M., Crepaz, N., & the TREND Group (2004). Improving the reporting quality of nonrandomized evaluation of behavioral and public health interventions: the TREND statement. American Journal of Public Health, 94, 361–366.
Díaz, R. M. (1998a). Hermanos de luna y sol: A model for HIV prevention with Latino gay men. In: R. M. Díaz (Ed.), Latino gay men and HIV: Culture, sexuality and risk behavior (pp. 151–175). New York: Routledge.
Díaz, R. M. (1998b). Latino gay men and HIV: Culture, sexuality, and risk behavior. New York: Routledge.
Díaz, R. M., Ayala, G., & Bein, E. (2004). Sexual risk as an outcome of social oppression: Data from a probability sample of Latino gay men in three U.S. cities. Cultural Diversity and Ethnic Minority Psychology, 10(3), 255–267.
Díaz, R. M., Morales, E. S., Bein, E., Dilan, E., & Rodriguez, R. A. (1999). Predictors of sexual risk in Latino gay/bisexual men: The role of demographic, developmental, social cognitive and behavioral variables. Hispanic Journal of Behavioral Sciences, 21, 480–501.
Diaz, T., Buehler, J. W., Castro, K. G., & Ward, J. W. (1993). AIDS trends among Hispanics in the United States. American Journal of Public Health, 83, 504–509.
Diaz, T., & Klevens, R. M. (1997). Differences by ancestry in sociodemographics and risk behaviors among Latinos with AIDS. The Supplement to HIV and AIDS Surveillance Project Group. Ethnicity and Disease, 7, 200–206.
Dolezal, C., & Carballo-Diéguez, A. (2002). Childhood sexual experiences and the perception of abuse among Latino men who have sex with men. Journal of Sex Research, 39(3), 165–173.
Drummond, M. F., & Jefferson, T. O. (1996). Guidelines for authors and peer reviewers of economic submissions to the Br Med J. The Br Med J Economic Evaluation Working Party. British Medical Journal, 313, 275–283.
*Dushay, R. A., Singer, M., Weeks, M. R., Rohena, L., & Gruber, R. (2001). Lowering HIV risk among ethnic minority drug users: Comparing culturally targeted intervention to a standard intervention. American Journal of Drug and Alcohol Abuse, 27, 501–524.
Durantini, M. R., Albarracin, D., Mitchell, A. L., Earl, A. N., & Gillette, J. C. (2006). Conceptualizing the influence of social agents of behavior change: A meta-analysis of the effectiveness of HIV-prevention interventionists for different groups. Psychological Bulletin, 132, 212–248.
Ebrahim, S. H., Anderson, J. E., Weidle, P., & Purcell, D. W. (2004). Race/ethnic disparities in HIV testing and knowledge about treatment for HIV/AIDS: United States, 2001. AIDS Patient Care and STDs, 18, 27–33.
Fisher, D. G., Reynolds, G. L., Moreno-Branson, C. M., Jaffe, A., Wood, M. M., Klahn, J. A., & Muniz, J. F. (2004). Drug treatment needs of Hispanic drug users in Long Beach, California. Journal of Drug Issues, 34(4), 879–894.
Flaskerud, J. H., Nyamathi, A. M., & Uman G. C. (1997). Longitudinal effects of an HIV testing and counseling programme for low-income Latina women. Ethnicity and Health, 2, 89–103.
Flores, S. A., & Crepaz, N. (2004). Quality of study methods in individual- and group-level HIV intervention research: Critical reporting elements. AIDS Education and Prevention, 16, 341–352.
Galanti, G. A. (2003). The Hispanic family and male–female relationships: An overview. Journal of Transcultural Nursing, 14(3), 180–185.
Gómez, C., & Marín, B. V. (1996). Gender, culture and power: Barriers to HIV prevention strategies. Journal of Sex Research, 33, 355–362.
Gómez, C. A., Hernandez, M., & Faigeles, B. (1999). Sex in the new world: An empowerment model for HIV prevention in Latina immigrant women. Health Education and Behavior, 26, 200–212.
González, G. M., Muñoz, R. F., Pérez-Arce, P., & Batki, S. L. (1993). Depression and HIV disease in injection drug users: A Spanish language feasibility study. Psychology of Addictive Behaviors, 7, 149–154.
Goodyear, R. K., Newcomb, M. D., & Allison, R. D. (2000). Predictors of Latino men’s paternity in teen pregnancy: Test of a mediational model of childhood experiences, gender role attitudes, and behaviors. Journal of Counseling Psychology, 47(1), 116–128.
Grella, C. E., Annon, J. J., & Anglin, M. D. (1995). Ethnic differences in HIV risk behaviors, self-perceptions, and treatment outcomes among women in methadone maintenance treatment. Journal of Psychoactive Drugs, 27, 421–433.
*Harvey, S. M., Henderson, J. T., Thorburn, S., Beckman, L. J., Casillas, A., Mendez, L., Cervantes, R. (2004). A randomized study of a pregnancy and disease prevention intervention for Hispanic couples. Perspectives on Sexual and Reproductive Health, 36, 162–169.
Hasselblad, V., & Hedges, L. V. (1995). Meta-analysis of screening and diagnostic tests. Psychological Bulletin, 117, 167–178.
Hedges, L. V., & Vevea, J. L. (1998). Fixed and random effects models in meta-analysis. Psychological Methods, 3, 486–504.
Herbst, J. H., Sherba, R. T., Crepaz, N., DeLuca, J. B., Zohrabyan, L., Stall, R., Lyles, C. M., & the HIV/AIDS Prevention Research Synthesis Team (2005). A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 39(2), 228–241.
Holtgrave, D. R. (2002). Estimating the effectiveness and efficiency of US HIV prevention efforts using scenario and cost-effectiveness analysis. AIDS, 16, 2347–2349.
Jarama, S. L., Kennamer, J. D., Poppen, P. J., Hendricks, M., & Bradford, J. (2005). Psychosocial, behavioral, and cultural predictors of sexual risk for HIV infection among Latino men who have sex with men. AIDS and Behavior, 9, 513–523.
Jemmott, J. B. III, Jemmott, L. S., Braverman, P. K., & Fong, G. T. (2005). HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: A randomized controlled trial. Archives of Pediatrics and Adolescent Medicine, 159, 440–449.
Johnson, A. M., Copas, A. J., Erens, B., Mandalia, S., Fenton, K., & Korovessis, C. (2002). Effect of computer-assisted self-interviews on reporting of sexual HIV risk behaviors in a general population sample: a methodological experiment. AIDS, 15, 111–115.
Johnson, B. T., Carey, M. P., Chaudoir, S. R., & Reid, A. E. (2006). Sexual risk reduction for persons living with HIV: Research synthesis of randomized controlled trials, 1993 to 2004. Journal of Acquired Immune Deficiency Syndromes, 41, 642–650.
Johnson, W. D., Semaan, S., Hedges, L. V., Ramirez, G., Mullen, P. D., & Sogolow, E. (2002). A protocol for the analytical aspects of a systematic review of HIV prevention research. Journal of Acquired Immune Deficiency Syndromes, 30(Suppl. 1), S62–S72.
Juni, P., Altman, D. G., & Egger, M. (2001). Assessing the quality of randomized controlled trials. In: M. Egger, G. D. Smith, & D. G. Altman (Eds.), Systematic reviews in health care: meta-analysis in context. London: BMJ.
Kahn, J. G., & Sanstad, K. C. (1997). The role of cost-effectiveness analysis in assessing HIV-prevention interventions. AIDS Public Policy Journal, 12, 21–30.
Kipke, M. D., Boyer, C., & Hein, K. (1993). An evaluation of an AIDS Risk Reduction Education and Skills Training (ARREST) program. Journal of Adolescent Health, 14, 533–539.
*Koniak-Griffin, D., Lesser, J., Nyamathi, A., Uman, G., Stein, J. A., & Cumberland, W. G. (2003). Project CHARM: An HIV prevention program for adolescent mothers. Family & Community Health, 26, 94–107.
Korte, J. E., Shain, R., Holden, A. E., Piper, J. M., Perdue, S. T., Champion, J. D., Sterneckert, K. (2004). Reduction in sexual risk behaviors and infection rates among African Americans and Mexican Americans. Sexually Transmitted Diseases, 31, 166–173.
Ksobiech, K. (2003). A meta-analysis of needle sharing, lending, and borrowing behaviors of needle exchange program attenders. AIDS Education and Prevention, 15(3), 257–268.
Lesser, J., Verdugo, R. L., Koniak-Griffin, D., Tello, J., Kappos, B., & Cumberland, W. G. (2005). Respecting and protecting our relationships: A community research HIV prevention program for teen fathers and mothers. AIDS Education and Prevention, 17, 347–360.
Levy, V., Page-Shafer, K., Evans, J., Ruiz, J., Morrow, S., Reardon, J., Lynch, M., Raymond, H. F., Klausner, J. D., Facer, M., Molitor, F., Allen, B., Ajufo, B. G., Ferrero, D., Sanford, G. B., McFarland, W., & The HeyMan Study Team (2005). HIV-related risk behavior among Hispanic immigrant men in a population-based household survey in low-income neighborhoods of northern California. Sexually Transmitted Diseases, 32(8), 487–490.
Lipsey, M. W., & Wilson, D. B. (2001). Practical meta-analysis. Thousand Oaks, CA: SAGE Publications.
Lyles, C. M., Crepaz, N., Herbst, J. H., & Kay, L. S. (2006). Evidence-based HIV behavioral prevention from the perspective of CDC’s HIV/AIDS Prevention Research Synthesis Team. AIDS Education and Prevention, 18(Suppl. A), 20–31.
Marín, B. V. (1995). Analysis of AIDS prevention among African Americans and Latinos in the United States. Washington, DC: Office of Technology Assessment, U.S. Congress.
Marín, B. V. (2003). HIV prevention in the Hispanic community: Sex, culture, and empowerment. Journal of Transcultural Nursing, 14(3), 186–192.
Marín, B. V., & Gómez, C. A. (1994). Latinos, HIV disease, and culture: Strategies for HIV prevention. In: P. T. Cohen, M. A. Sande, & P. A. Volberding (Eds.), The AIDS knowledge base (pp. 108–113). Boston, MA: Little, Brown & Co.
Marín, B. V., & Gómez, C. A. (1997). Latino culture and sex: Implications for HIV prevention. In: J. G. Garcia, & M. C. Zea (Eds.), Psychological interventions and research with Latino populations (pp. 73–93). Boston, MA: Allyn & Bacon.
Marín, B. V., Gómez, C., Tschann, J., & Gregorich, S. (1997). Condom use in unmarried Latino men: A test of cultural constructs. Health Psychology, 16, 458–467.
Marín, B. V., Tschann, J. M., Gómez, C. A., & Kegeles, S. M. (1993). Acculturation and gender differences in sexual attitudes and behaviors: Hispanic vs. non-Hispanic white unmarried adults. American Journal of Public Health, 83, 1759–1761.
Marín, G., & Marín, B. V. (1991). Research with Hispanic populations. Newbury Park, CA: Sage.
Maxwell, A. E., Bastani, R., & Warda, U. S. (2002). Pilot test of a single-session AIDS workshop for young Hispanic U.S. immigrants. Journal of Immigrant Health, 4, 73–79.
McGraw, S. A., Smith, K. W., Crawford, S. L., Costa, L. A., McKinlay, J. B., & Bullock, K. (2002). The effectiveness of Poder Latino: A community-based HIV prevention program for inner-city Latino youth(Unpublished manuscript).
*Mishra, S. I., & Conner, R. F. (1996). Evaluation of an HIV prevention program among Latino farmworkers. In: S. I. Mishra, R. F. Conner, & J. R. Magaña (Eds.), Crossing borders: The spread of HIV among migrant Latinos (pp. 157–181). Boulder, CO: Westview Press.
*Mishra, S. I., Sanudo, F., & Conner, R. F. (2004). Collaborative research toward HIV prevention among migrant farmworkers. In: B. P. Bowser, S. I. Mishra, C. J. Reback, & G. F. Lemp (Eds.), Preventing AIDS: Community-science collaborations (pp. 69–95). New York, NY: Haworth Press.
Moher, D., Schulz, K. F., & Altman, D. G. (2001). The CONSORT statement: Revised recommendations for improving the quality of reports of parallel group randomised trials. The Lancet, 357, 1191–1194.
Newman, J. C., Des Jarlais, D. C., Turner, C. F., Gribble, J., Cooley, P., & Paone, D. (2002). The differential effects of face-to-face and computer interview methods. American Journal of Public Health, 92(2), 294–297.
*Nyamathi, A. M., Flaskerud, J., Bennett, C., Leake, B., & Lewis, C. (1994). Evaluation of two AIDS education programs for impoverished Latina women. AIDS Education and Prevention, 6, 296–309.
Nyamathi, A., & Vasquez, R. (1995). Impact of poverty, homelessness, and drugs on Hispanic women at risk for HIV infection. In: A. M. Padilla (Ed.), Hispanic psychology: Critical issues in theory and research (pp. 213–227). Thousand Oaks, CA: Sage Publications.
*O’Donnell, L., San Doval, A., Duran, R., & O’Donnell, C. R. (1995). The effectiveness of video-based interventions in promoting condom acquisition among STD clinic patients. Sexually Transmitted Diseases, 22, 97–103.
O’Donnell, C. R., O’Donnell, L., San Doval, A., Duran, R., & Labes, K. (1998). Reductions in STD infections subsequent to an STD clinic visit: Using video-based patient education to supplement provider interactions. Sexually Transmitted Diseases, 25, 161–168.
Office of the Surgeon General. (2000). Evidence-based findings on the efficacy of syringe exchange programs: An analysis from the Assistant Secretary for Health and Surgeon General of the scientific research completed since April 1998. Retrieved November 29, 2005, from http://www.harmreduction.org/research/surgeongenrev/surgreview.html.
Organista, K. C., Alvarado, N., Balblutin-Burnham, A., Worby, P., & Martinez, S. (2004a). HIV prevention with Mexican/Latino migrant day laborers: Pilot study findings and description of a university-community collaboration (unpublished manuscript).
Organista, K. C., Carrillo, M., & Ayala, G. (2004b). HIV prevention with Mexican migrants—Review, critique, and recommendations. Journal of Acquired Immune Deficiency Syndromes, 37(Suppl. 4), S227–S239.
Page, J. B. (2005). The concept of culture: A core issue in health disparities. Journal of Urban Health, 82(Suppl. 3), III35–III43.
Pan American Health Organization. (2000). Update on HIV/AIDS surveillance in the Americas. Epidemiological Bulletin, 21(3), 10–11.
Parrado, E. A., Flippen, C. A., & McQuiston, C. (2004). Use of commercial sex workers among Hispanic migrants in North Carolina: Implications for the spread of HIV. Perspectives on Sexual and Reproductive Health, 36(4), 150–156.
*Peragallo, N., DeForge, B., O’Campo, P., Lee, S. M., Kim, Y. J., Cianelli, R., & Ferrer, L. (2005). A randomized clinical trial of an HIV-risk-reduction intervention among low-income Latina women. Nursing Research, 54, 108–118.
Peragallo, N., DeForge, B. R., Khoury, Z., Rivero, R., & Talashek, M. (2002). Latinas’ perspectives on HIV/AIDS: Cultural issues to consider in prevention. Hispanic Health Care International, 1, 11–22.
Pew Research Center. (2005). Hispanics: A people in motion. Washington, DC: Pew Research Center.
*Raj, A., Amaro, H., Cranston, K., Martin, B., Cabral, H., Navarro, A., & Conron, K. (2001). Is a general women’s health promotion program as effective as an HIV-intensive prevention program in reducing HIV risk among Hispanic women?. Public Health Reports, 116, 599–607.
Raj, A., Silverman, J. G., & Amaro, H. (2004). Abused women report greater male partner risk and gender-based risk for HIV: Findings from a community-based study with Hispanic women. AIDS Care, 16(4), 519–529.
Resnicow, K., Baranowski, T., Ahluwalia, J. S., & Braithwaite, R. L. (1999). Cultural sensitivity in public health: Defined and demystified. Ethnicity and Disease, 9, 10–21.
Reyes, J. C., Robles, R. R., Colón, H. M., Matos, T. D., Finlinson, H. A., & Marrero, C. A., et al. (2005). Homelessness and HIV risk behaviors among drug injectors in Puerto Rico. Journal of Urban Health, 83(2), 446–455.
*Robles, R. R., Reyes, J. C., Colón, H. M., Sahai, H., Marrero, C. A., Matos, T. D., Calderón, J. M., & Shepard, E. W. (2004). Effects of combined counseling and case management to reduce HIV risk behaviors among Hispanic drug injectors in Puerto Rico. Journal of Substance Abuse Treatment, 27(2), 145–152.
Romo, L. F., Berenson, A. B., & Segars, A. (2004). Sociocultural and religious influences on the normative contraceptive practices of Latino women in the United States. Contraception, 69(3), 219–225.
Rotheram-Borus, M. J., Reid, H., & Rosario, M. (1994). Factors mediating changes in sexual HIV risk behaviors among gay and bisexual male adolescents. American Journal of Public Health, 84, 1938–1946.
Russell, L. D., Alexander, M. K., & Corbo, K. F. (2000). Developing culture-specific interventions for Latinas to reduce HIV high-risk behaviors. Journal of Associated Nurses AIDS Care, 11(3), 70–76.
*Schilling, R. F., El-Bassel, N., Schinke, S. P., Gordon, K., & Nichols, S. (1991). Building skills of recovering women drug users to reduce heterosexual AIDS transmission. Public Health Reports, 106, 297–304.
*Schilling, R. F., Fernando, D., Fontdevila, J., & El-Bassel, N. (2000). HIV risk reduction among injection drug users: Explaining the lack of anticipated outcomes in a community-level controlled comparison study. Evaluation and Program Planning, 23, 301–313.
Schroeder, K. E., Carey, M. P., & Vanable, P. A. (2003). Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Annals of Behavioral Medicine, 26, 104–123.
*Sellers, D. E., McGraw, S. A., & McKinlay, J. B. (1994). Does the promotion and distribution of condoms increase teen sexual activity? Evidence from an HIV prevention program for Latino youth. American Journal of Public Health, 84, 1952–1959.
Semaan, S., Des Jarlais, D. C., Sogolow, E., Johnson, W. D., Hedges, L. V., Ramirez, G., Flores, S. A., Norman, L., Sweat, M. D., & Needle, R. (2002). A meta-analysis of the effect of HIV prevention interventions on the sex behaviors of drug users in the United States. Journal of Acquired Immune Deficiency Syndromes, 30(Suppl. 1), S73–S93.
Shadish, W. R., Cook, T. D., & Campbell, D. T. (2002). Experimental and quasi-experimental designs for generalized causal inference. Boston: Houghton Mifflin.
*Shain, R. N., Piper, J. M., Newton, E. R., Perdue, S. T., Ramos, R., Champion, J. D., & Guerra, F. A. (1999). A randomized, controlled trial of a behavioral intervention to prevent sexually transmitted disease among minority women. New England Journal of Medicine, 340, 93–100.
*Shain, R. N., Piper, J. M., Holden, A. E., Champion, J. D., Perdue, S. T., Korte, J. E., & Guerra, F. A. (2004). Prevention of gonorrhea and chlamydia through behavioral intervention: Results of a two-year controlled randomized trial in minority women. Sexually Transmitted Diseases, 31, 401–408.
Shedlin, M. G., Decena, C. U., & Oliver-Velez, D. (2005). Initial acculturation and HIV risk among new Hispanic immigrants. Journal of the National Medical Association, 97(7), 32S–37S.
Sogolow, E., Peersman, G., Semaan, S., Strouse, D., & Lyles, C. M. (2002). The HIV/AIDS Prevention Research Synthesis Project: Scope, methods, and study classification results. Journal of Acquired Immune Deficiency Syndromes, 30(Suppl. 1), S15–S29.
Strathdee, S. A. (2003). Sexual HIV transmission in the context of injection drug use: Implications for interventions. International Journal on Drug Policy, 14, 79–81.
Strathdee, S. A., & Vlahav, D. (2001). The effectiveness of needle exchange programs: A review of the science and policy. AIDScience, 1, 1–31.
*Suarez-Al-Adam, M., Raffaelli, M., & O’Leary, A. (2000). Influence of abuse and partner hypermasculinity on the sexual behavior of Latinas. AIDS Education and Prevention, 12, 263–274.
Sumartojo, E. (2000). Structural factors in HIV prevention: Concepts, examples, and implications for research. AIDS, 14(Suppl. 1), S3–S10.
Toro-Alfonso, J., Varas-Díaz, N., & Andujar-Bello, I. (2002). Evaluation of an HIV/AIDS prevention intervention targeting Latino gay men and men who have sex with men in Puerto Rico. AIDS Education and Prevention, 14, 445–456.
U.S. Census Bureau. (2004). Annual estimates of the population by race alone and Hispanic or Latino origin for the United States: July 1, 2003. Retrieved July 26, 2005, from http://www.census.gov/popest/states/asrh/tables/SC-EST2003–04.pdf.
U.S. Census Bureau. (2005). Hispanic population passes 40 million, Census Bureau reports. Retrieved June 9, 2005, 2005, from www.census.gov/Press-Release/www/releases/archives/population/005164.html.
van Servellen, G., Brown, J. S., Lombardi, E., & Herrera, G. (2003). Health literacy in low-income Latino men and women receiving antiretroviral therapy in community-based treatment centers. AIDS Patient Care and STDs, 17, 283–298.
*Villarruel, A. M., Jemmott, J. B., & Jemmott, L. S. (2006). A randomized controlled trial testing an HIV prevention intervention for Latino youth. Archives of Pediatrics and Adolescent Medicine, 160, 772–777.
Villarruel, A. M., Jemmott, L. S., & Jemmott, J. B. (2005). Designing a culturally based intervention to reduce HIV sexual risk for Latino adolescents. The Journal of the Association of Nurses in AIDS Care, 16, 23–31.
Wong, W., Tambis, J. A., Hernandez, M. T., Chaw, J. K., & Klausner, J. D. (2003). Prevalence of sexually transmitted diseases among Latino immigrant day laborers in an urban setting—San Francisco. Sexually Transmitted Diseases, 30(8), 661–663.
Zea, M. C., Reisen, C. A., & Díaz, R. M. (2003). Methodological issues in research on sexual behavior with Latino gay and bisexual men. American Journal of Community Psychology, 31(3–4), 281–291.
Acknowledgements
The following current and former PRS team members contributed to this review (listed alphabetically): Julia B. DeLuca, Angela B. Hutchinson, Angela Kim, Paola Marrero-Gonzales, Mary Mullins, Sima Rama, R. Thomas Sherba, and Sekhar Thadiparthi. The authors also extend special thanks to the following researchers for providing additional information or outcome data regarding their interventions: Alex Carballo-Diéguez, Felipe Castro, Marie Harvey, Deborah Koniak-Griffin, Sarah McGraw, Carl O’Donnell, Anita Raj, Rafaela Robles, Robert Schilling, Merrill Singer, and Antonia Villarruel. The authors also thank Mary Spink Neumann, Carolyn G. Beeker, and three anonymous reviewers for providing insightful comments.
This work was supported by the Prevention Research Branch, Division of HIV/AIDS Prevention and was not funded by any other organization. Preliminary findings of this review were presented at the 111th Annual Convention of the American Public Health Association in Washington, DC (November, 2004), and at the 2005 National HIV Prevention Conference in Atlanta, GA (June, 2005).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the U.S. Centers for Disease Control and Prevention.
Rights and permissions
About this article
Cite this article
Herbst, J.H., Kay, L.S., Passin, W.F. et al. A Systematic Review and Meta-Analysis of Behavioral Interventions to Reduce HIV Risk Behaviors of Hispanics in the United States and Puerto Rico. AIDS Behav 11, 25–47 (2007). https://doi.org/10.1007/s10461-006-9151-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-006-9151-1