Abstract
Background
In addition to cost-effectiveness, national guidelines often include other factors in reimbursement decisions. However, weights attached to these are rarely quantified, thus decisions can depend strongly on decision-maker preferences.
Objective
To explore the preferences of policymakers and healthcare professionals involved in the decision-making process for different efficiency and equity attributes of interventions and to analyse cross-country differences.
Method
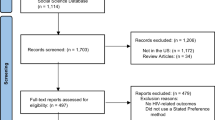
Discrete choice experiments (DCEs) were carried out in Austria, Hungary, and Norway with policymakers and other professionals working in the health industry (N = 153 respondents). Interventions were described in terms of different efficiency and equity attributes (severity of disease, target age of the population and willingness to subsidise others, potential number of beneficiaries, individual health benefit, and cost-effectiveness). Parameter estimates from the DCE were used to calculate the probability of choosing a healthcare intervention with different characteristics, and to rank different equity and efficiency attributes according to their importance.
Results
In all three countries, cost-effectiveness, individual health benefit and severity of the disease were significant and equally important determinants of decisions. All countries show preferences for interventions targeting young and middle aged populations compared to those targeting populations over 60. However, decision-makers in Austria and Hungary show preferences more oriented to efficiency than equity, while those in Norway show equal preferences for equity and efficiency attributes.
Conclusion
We find that factors other than cost-effectiveness seem to play an equally important role in decision-making. We also find evidence of cross-country differences in the weight of efficiency and equity attributes.
Similar content being viewed by others
Notes
The Main Association of Austrian Social Security Institutions) based on the recommendations of the Pharmaceutical Evaluation Board classify the drugs into three different reimbursement categories: red, green and yellow boxes.
(1) Priorities of the health care system, (2) severity of the disease, (3) equity (size of the target population, accessibility), (4) cost-effectiveness and quality of life (ICER, health gain per patient), (5) budget impact, and (6) opinions from Hungary and abroad.
e.g. National Health Insurance Fund, Ministry of Human Resources, National Institute for Quality and Organisational Development in Healthcare and Medicines.
Purely equitable and purely efficient interventions are those where all equity attributes are set to 1 (with all efficiency attributes to 0) and those where all efficiency attributes are set to 1 (with all equity attributes to 0), respectively.
Results are available from the authors upon request.
Results are available from the authors upon request.
References
Dakin, H., Devlin, N., Feng, Y., Rice, N., O’Neill, P., Parkin, D.: The influence of cost-effectiveness and other factors on nice decisions. Health Econ. (2014). doi: 10.1002/hec.3086
Sabik, L.M., Lie, R.K.: Priority setting in health care: lessons from the experiences of eight countries. Int. J. Equity Health 7, 4 (2008)
Gulacsi, L., Rotar, A.M., Niewada, M., Loblova, O., Rencz, F., Petrova, G., Boncz, I., Klazinga, N.S.: Health technology assessment in Poland, the Czech Republic, Hungary, Romania and Bulgaria. Eur. J. Health Econ. 15(Suppl 1), S13–S25 (2014)
Norheim, O.F., Baltussen, R., Johri, M., Chisholm, D., Nord, E., Brock, D., Carlsson, P., Cookson, R., Daniels, N., Danis, M., Fleurbaey, M., Johansson, K.A., Kapiriri, L., Littlejohns, P., Mbeeli, T., Rao, K.D., Edejer, T.T., Wikler, D.: Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost Eff. Resour. Alloc. 12, 18 (2014)
Rawlins, M., Barnett, D., Stevens, A.: Pharmacoeconomics: NICE’s approach to decision-making. Br. J. Clin. Pharmacol. 70(3), 346–349 (2010)
Green, C., Gerard, K.: Exploring the social value of health-care interventions: a stated preference discrete choice experiment. Health Econ. 18(8), 951–976 (2009)
Baltussen, R., Niessen, L.: Priority setting of health interventions: the need for multi-criteria decision analysis. Cost Eff. Resour. Alloc. 4, 14 (2006)
Baltussen, R., Stolk, E., Chisholm, D., Aikins, M.: Towards a multi-criteria approach for priority setting: an application to Ghana. Health Econ. 15(7), 689–696 (2006)
Marsh, K., Lanitis, T., Neasham, D., Orfanos, P., Caro, J.: Assessing the value of healthcare interventions using multi-criteria decision analysis: a review of the literature. Pharmacoeconomics 32(4), 345–365 (2014)
Defechereux, T., Paolucci, F., Mirelman, A., Youngkong, S., Botten, G., Hagen, T.P., Niessen, L.W.: Health care priority setting in Norway a multicriteria decision analysis. BMC Health Serv. Res. 12, 39 (2012)
Koopmanschap, M.A., Stolk, E.A., Koolman, X.: Dear policy maker: have you made up your mind? A discrete choice experiment among policy makers and other health professionals. Int. J. Technol. Assess Health Care 26(2), 198–204 (2010)
Mentzakis, E., Paolucci, F., Rubicko, G.: Priority setting in the Austrian healthcare system: results from a discrete choice experiment and implications for mental health. J. Ment. Health Policy Econ. 17(2), 61–73 (2014)
Watson, V., Carnon, A., Ryan, M., Cox, D.: Involving the public in priority setting: a case study using discrete choice experiments. J. Public Health (Oxf) 34(2), 253–260 (2012)
Ratcliffe, J., Bekker, H.L., Dolan, P., Edlin, R.: Examining the attitudes and preferences of health care decision-makers in relation to access, equity and cost-effectiveness: a discrete choice experiment. Health Policy 90(1), 45–57 (2008)
Lim, M.K., Bae, E.Y.: Eliciting stated preferences for drugs reimbursement decision criteria in South Korea. Korean J. Health Policy Adm. 19(4), 98–120 (2009)
Buchholz, P.: ISPOR Global Health Systems Road Map. http://www.ispor.org/htaroadmaps/Austria.asp (2009). Accessed 15 October 2014
Räpple, T.: Pricing and Reimbursement Handbook. Baker & McKenzie. http://www.bakermckenzie.com/files/Uploads/Documents/Germany/LifeSciences/EuropeanPricingReimbursement.pdf (2011) Accessed 15 October 2014
Endrei, D., Molics, B., Agoston, I.: Multicriteria decision analysis in the reimbursement of new medical technologies: real-world experiences from Hungary. Value Health 17(4), 487–489 (2014)
Dankó, D.: Health technology assessment in middle-income countries: recommendations for a balanced assessment system. J. Market Access Health Policy 2(23181), 1–10 (2014)
Gulacsi, L., Orlewska, E., Pentek, M.: Health economics and health technology assessment in Central and Eastern Europe: a dose of reality. Eur. J. Health Econ. 13(5), 525–531 (2012)
Ringard, A., Morland, B., Larsen, B.I.: Quality and priorities in the health services. Tidsskr. Nor. Laegeforen. 132(3), 312–314 (2012)
Ryan, M., Gerard, K.: Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl. Health Econ. Health Policy 2(1), 55–64 (2003)
Baltussen, R., ten Asbroek, A.H., Koolman, X., Shrestha, N., Bhattarai, P., Niessen, L.W.: Priority setting using multiple criteria: should a lung health programme be implemented in Nepal? Health Policy Plan 22(3), 178–185 (2007)
Mirelman, A., Mentzakis, E., Kinter, E., Paolucci, F., Fordham, R., Ozawa, S., Ferraz, M., Baltussen, R., Niessen, L.W.: Decision-making criteria among national policymakers in five countries: a discrete choice experiment eliciting relative preferences for equity and efficiency. Value Health 15(3), 534–539 (2012)
Noorani, H.Z., Husereau, D.R., Boudreau, R., Skidmore, B.: Priority setting for health technology assessments: a systematic review of current practical approaches. Int. J. Technol. Assess Health Care 23(3), 310–315 (2007)
Youngkong, S., Kapiriri, L., Baltussen, R.: Setting priorities for health interventions in developing countries: a review of empirical studies. Trop. Med. Int. Health 14(8), 930–939 (2009)
Hensher, D.A., Rose, J.M., Greene, W.H.: Applied choice analysis: a primer. Cambridge University Press, Cambridge (2005)
McFadden, D.: Conditional logit analysis of qualitative choice behavior. In: Zarembka, P. (ed.) Frontiers in econometrics. pp. 105–142. Academic, New York (1974)
DeShazo, J.R., Fermo, G.: Designing choice sets for stated preference methods: the effects of complexity on choice consistency. J. Environ. Econ. Manag. 44(1), 123–143 (2002)
Hensher, D., Greene, W.: The Mixed Logit model: the state of practice. Transportation 30(2), 133–176 (2003)
Lancsar, E., Louviere, J., Flynn, T.: Several methods to investigate relative attribute impact in stated preference experiments. Soc. Sci. Med. 64(8), 1738–1753 (2007)
Shillcutt, S.D., Walker, D.G., Goodman, C.A., Mills, A.J.: Cost effectiveness in low- and middle-income countries: a review of the debates surrounding decision rules. Pharmacoeconomics 27(11), 903–917 (2009)
Whitty, J.A., Lancsar, E., Rixon, K., Golenko, X., Ratcliffe, J.: A systematic review of stated preference studies reporting public preferences for healthcare priority setting. Patient 7(4):365–386 (2014)
Whitty, J.A., Scuffham, P.A., Rundle-Thielsee, S.: Public and decision maker stated preferences for pharmaceutical subsidy decisions. Appl. Health Econ. Health Policy 9(2), 73–79 (2009)
Acknowledgments
The authors are grateful for Georg Rubiko, University of Innsbruck, Austria, Prof. Terje P. Hagen, Department of Health Management and Health Economics, University of Oslo, Norway, Dr. Márta Péntek, Department of Health Economics, Corvinus University of Budapest, Hungary, Dr. Valentin Brodszky, Department of Health Economics, Corvinus University of Budapest, Hungary for their assistance in the data collection. Petra Baji was supported by the Hungarian Scientific Research Fund OTKA (PD 112499). Manuel García-Goñi’s research was supported by the research project Evaluating Preferences for Equity and Efficiency among National/Regional Health Policy Makers” financed by the Spanish Instituto de Estudios Fiscales.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baji, P., García-Goñi, M., Gulácsi, L. et al. Comparative analysis of decision maker preferences for equity/efficiency attributes in reimbursement decisions in three European countries. Eur J Health Econ 17, 791–799 (2016). https://doi.org/10.1007/s10198-015-0721-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-015-0721-x