Abstract
In 2009, the National Institute for Health and Clinical Excellence (NICE) issued supplementary advice to its Appraisal Committees to be taken into account when appraising life-extending, ‘end-of-life’ treatments. This indicated that if certain criteria are met, it may be appropriate to recommend the use of such treatments even if they would not normally be considered cost-effective. However, NICE’s public consultation revealed concerns that there is little scientific evidence to support such a policy. This study examines whether there is public support for giving higher priority to life-extending, end-of-life treatments than to other types of treatment. In face-to-face interviews, respondents answered six questions asking them to choose which of two hypothetical patients they would prefer to treat, assuming that the health service has enough funds to treat one but not both of them. The various scenarios were designed so as to control for age- and time-related preferences. Fifty members of the general public in England were interviewed in July 2011. We find some evidence of support for giving priority to the patient with shorter remaining life expectancy, but note that a nontrivial minority of respondents expressed the opposite preference. Substantial preference for quality-of-life improvement over life extension was observed. Very few respondents expressed indifference or unwillingness to choose between the patients. Whilst there cannot be described to be a single ‘consensus’ set of preferences, we conclude that there are ways in which the results suggest that the current NICE policy may be insufficient.
Similar content being viewed by others
References
Weinstein, M.C., Stason, W.B.: Foundations of cost-effectiveness analysis for health and medical practices. N. Engl. J. Med. 296, 716–721 (1997)
NICE: Guide to the Methods of Technology Appraisal. NICE, London (2008)
NICE: Social Value Judgements: Principles for the Development of NICE Guidance, 2nd edn. NICE, London (2008)
NICE: Appraising life-extending, end of life treatments. NICE, London (2009)
Rawlins, M.D., Culyer, A.J.: National Institute for Clinical Excellence and its value judgments. BMJ 329, 224–227 (2004)
NICE: End of Life Treatments: Summary Response to Consultation. NICE, London (2009)
NICE: Appraising Life-Extending, End of Life Treatments. NICE, London (2009). Revised in July 2009
Department of Health: The New NHS: Modern, Dependable. Department of Health, London (1997)
Department of Health: Involving Patients and the Public in Healthcare: A Discussion Document. Department of Health, London (2001)
Ryan, M., Scott, D.A., Reeves, C., Bate, A., van Teijlingen, E.R., Russell, E.M., et al.: Eliciting public preferences for healthcare: a systematic review of techniques. Health Technol. Assess. 5(5), 1–185 (2001)
Richardson, J., McKie, J.: Empiricism, ethics and orthodox economic theory: what is the appropriate basis for decision-making in the health sector? Soc. Sci. Med. 60, 265–275 (2005)
Shah, K.K.: Severity of illness and priority setting in healthcare: a review of the literature. Health Policy 93, 77–84 (2009)
Department of Health: Impact Assessment of Proposal for a Cancer Drug Fund. Department of Health, London (2010)
Donaldson, C. (project co-ordinator) et al.: European value of a quality adjusted life year: final publishable report. (2011) Available at: http://research.ncl.ac.uk/eurovaq/ Accessed 27 Dec 2012
Baker, R., McHugh, N., Mason, H., Currie, G., Donaldson, C.: Valuing end of life technologies, investigating the existence of a ‘cancer premium’ and methodological questions for health economics virtuous. Paper presented at the Health Economists’ Study Group meeting, Bangor (2011)
Pinto-Prades, J.L., Sanchez-Martinez, F.I., Corbacho, B.: Valuing QALYs at the end of life. Working paper 11.15. Universidad Pablo de Olavide, Seville (2011)
Linley, W.G., Hughes, D.G.: Societal views on NICE, Cancer Drugs Fund and value-based pricing criteria for prioritising medicines: a cross-sectional survey of 4118 adults in Great Britain. Health Economics (early view), doi:10.1002/hec.2872
Dolan, P., Shaw, R., Tsuchiya, A., Williams, A.: QALY maximisation and people’s preferences: a methodological review of the literature. Health Econ. 14, 197–208 (2005)
Treasury, H.M.: The Green Book: Appraisal and Evaluation in Central Government. TSO, London (2003)
Shah, K.K., Tsuchiya, A., Wailoo, A.J.: Valuing health at the end of life: an exploratory preference elicitation study. OHE Research Paper 11/06. Office of Health Economics, London (2011)
ONS: 2001 Census: standard area statistics (England and Wales). http://www.neighbourhood.statistics.gov.uk/dissemination/ (2001). Accessed 1 June 2012
Baker, R., Bateman, I., Donaldson, C., Jones-Lee, M., Lancsar, E., Loomes, G., et al.: Weighting and valuing quality-adjusted life-years using stated preference methods: preliminary results from the Social Value of a QALY Project. Health Technol. Assess. 14, 1–162 (2010)
Wailoo, A., Tsuchiya, A., McCabe, C.: Weighting must wait: incorporating equity concerns into cost-effectiveness analysis may take longer than expected. Pharmacoeconomics 27, 983–989 (2009)
Lancsar, E., Louvriere, J.: Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics 26, 661–677 (2008)
Longson, C., Littlejohns, P.: Update Report on the Application of the ‘End-of-Life’ Supplementary Advice in Health Technology Appraisals. NICE, London (2009)
Acknowledgments
This article is based on work funded by the National Institute for Health and Clinical Excellence through its Decision Support Unit. The views, and any errors or omissions, expressed in this article are of the authors only. We are grateful for the contributions of Meindert Boysen, John Brazier, Bérengère Davin, Simon Dixon, Jenny Dunn, Karen Gerard, Arne Risa Hole, Jonathan Michaels, Bhash Naidoo, Janet Robertson, Andrew Stevens, Aurélia Tison and Rebecca Trowman. We would also like to thank all of the respondents who took part in the study.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Excerpt from interviewer script (description for scenario S1)
Consider two patients, patient A and patient B. Both patients are adults, and are the same age as each other. Suppose that both patient A and patient B have just been diagnosed with illnesses. The illnesses are asymptomatic – that is, they have no effect on the patient’s health-related quality of life.
Patient A will live for 10 years, from today, before dying. Patient B will live for 1 year, from today, before dying.
There is a treatment, which, if taken today, would extend the life of either patient A or patient B by 6 months. Treatment would not affect either patient’s health-related quality of life. However, the health service has only enough funds to treat one of the two patients, and there are no alternative treatments available. Furthermore, the nature of the illnesses is such that further treatment will not be possible if either patient is not treated today–this is the only opportunity for treatment.
Please complete the questions for Scenario 1.
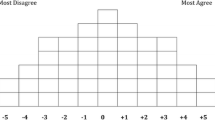
Excerpt from participant booklet (diagram and table for scenario S1)
See Fig. 1.
-
1.
If the health service has only enough funds to treat one of the two patients, which of the following statements best describes your view? (tick one box only)
-
□ I would prefer the health service to treat patient A
-
□ I have no preference
-
□ I would prefer the health service to treat patient B
-
-
2.
Which of the following statements reflect the reason(s) for your answer to question 1? (tick all boxes that apply)
-
□ My choice delivers the largest benefit
-
□ My choice is the most fair
-
□ My choice delivers the benefit today rather than far away in the future
-
□ My choice benefits the patient who is closest to death
-
□ My choice benefits the patient who has longer left to live
-
□ My choice benefits the patient with less time to prepare for death
-
□ My choice benefits the patient who can make the most out of their remaining time
-
□ My choice benefits the patient who is worse off
-
□ My choice benefits the patient who is younger today
-
□ My choice benefits the patient who is older today
-
□ My choice benefits the patient who will die at a younger age
-
□ My choice benefits the patient who will die at an older age
-
□ I think that it is better to improve health than to extend life in this situation
-
□ I think that it is better to extend life than to improve health in this situation
-
□ I think that both patients are equally deserving of treatment
-
□ I think that it is unfair to choose between the patients
-
□ I am unwilling to choose between the patients
-
□ None of the above.
-
Rights and permissions
About this article
Cite this article
Shah, K.K., Tsuchiya, A. & Wailoo, A.J. Valuing health at the end of life: an empirical study of public preferences. Eur J Health Econ 15, 389–399 (2014). https://doi.org/10.1007/s10198-013-0482-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-013-0482-3