Abstract
Purpose
Transanal irrigation is increasingly used against chronic constipation and fecal incontinence in selected patients. The aims were to estimate the incidence of irrigation-related bowel perforation in patients using the Peristeen Anal Irrigation® system, and to explore patient- and procedure-related factors associated with perforation.
Methods
External independent expert audit on the complete set of global vigilance data related to Peristeen Anal Irrigation from 2005 to 2013.
Results
In total, 49 reports of bowel perforation had been recorded. Based on sales figures, this corresponds to an average risk of bowel perforation of 6 per million procedures. The latest two-year data indicate a risk of 2 per million procedures. In 29 out of 43 evaluable cases (67 %), perforation happened within the first 8 weeks since start of treatment. After 8 weeks, long-term use has an estimated risk of less than 2 per million procedures. Among patients with non-neurogenic bowel dysfunction, 11 out of 15 (73 %) had a history of pelvic organ surgery compared to 5 out of 26 (19 %) in neurogenic bowel dysfunction. In 11 of 46 (24 %) evaluable cases, burst of the rectal balloon was reported.
Conclusion
Enema-induced perforation is a rare complication to transanal irrigation with Peristeen Anal Irrigation, which increases the benefit risk ratio in support of the further use of transanal irrigation. Increased risk is present during treatment initiation and in patients with prior pelvic organ surgery. Careful patient selection, patient evaluation and proper training of patients are critical to safe practice of this technique.
Similar content being viewed by others
Introduction
In recent years, transanal irrigation (TAI) has become a well-established treatment for chronic constipation and fecal incontinence in selected patients [1–3]. The procedure provides sufficient evacuation of the left colon to relieve constipation and reduce fecal incontinence in symptomatic individuals [4]. While initially reserved for spinal cord injured individuals, it is now increasingly used in idiopathic patients with functional constipation and fecal incontinence, and in patients suffering from functional bowel problems after rectal surgery [5–7].
As discussed in a recent Consensus Review [3], TAI procedures are routinely performed on a daily or almost daily basis. With instruction, the treatment is easy to learn, self-administered and well accepted by most patients. Treatment is regarded as a safe procedure, although mild and transient side effects may occur during or after irrigation. Nevertheless, inserting a catheter into rectum, inflating a rectal balloon and administration of an enema under pressure carry the risk of a potentially lethal bowel perforation. A single previous study yielded an estimated risk of irrigation-induced bowel perforation of 20 perforations per million procedures, regardless of irrigation system used [5]. Since the occurrence is rare, reports of perforations have been sporadic, and the true incidence is unknown.
To evaluate the guidance given in the Consensus Review [3] and to obtain global information about incidence rates as well as the patient- and procedure-related factors associated with TAI-induced bowel perforations, the manufacturer of a TAI system (Peristeen Anal Irrigation® (Coloplast A/S, Humlebæk, Denmark) was approached and agreed to give the authors full unrestricted access to all case information received with reports of bowel perforations related to Peristeen Anal Irrigation since launch in 2005. This provides a unique insight into the rare events of bowel perforation associated with TAI on a global level, which would not be otherwise possible. The objectives were to estimate the incidence rate of irrigation-related bowel perforation, exemplified by the Peristeen system, to explore patient- and procedure-related factors associated with perforation, and thereby to provide information that can help to reduce the risk for perforation even further in future.
Method
Vigilance procedures within Coloplast
Collection, processing and reporting of incidents occurring with medical devices are regulated procedures given by the European Community, US Food and Drug Association (FDA) or other National Competent Authorities. The Coloplast Vigilance Department assures that these requirements are met and implemented throughout the company. This implies that any information of a bowel perforation received (e.g., verbally, by mail or literature) is immediately registered in a complaint tracking system. Reports are received either directly from patients, or indirectly from healthcare personnel or national authorities. To improve data completeness, the information sources were approached with a structured questionnaire to obtain further information regarding the event and factors related to it. In cases with information of catheter lot numbers, quality assessment of the affected lot is performed to evaluate potential product failures.
To meet reporting requirements, an initial report is submitted to relevant health authorities and followed up by a final report normally after 6 weeks. Reports are essentially restricted to the initial outcome of the incident since the company has neither the duty nor the access to pursue long-term follow-up on the patients.
Each reported case is medically assessed in Coloplast and reported to the relevant Competent Authority. On an annual basis, all cases have been assessed by an independent, external medical specialist and data presented to the Coloplast Medical Advisory Board.
The Peristeen Anal Irrigation® system, including an Instruction for Use (IFU) and various training programs for nurses, has been available since 2005. In 2012, a redesigned softer rectal catheter with a new balloon was introduced, the IFU was revised and the nurse training programs considerably intensified.
Material
All reports of Peristeen-related bowel perforations submitted to Coloplast since launch 2005 to the end of 2013 were evaluated. The authors were allowed full and uncensored access to all company information related to the bowel perforation including reports, annexes, emails, correspondences, publications, and legal issues. An agreement between the principal author and Coloplast was signed to allow for publication of the results but not of business sensitive data (e.g., sales data).
Each case was subjected to review by two independent reviewers (coauthors) who were randomly assigned to cases. For each case, the reviewers completed a questionnaire to allow for a structured analysis of data regarding the information source (complainant), end user, etiology, concomitant factors, pretreatment evaluation, training and prior practical problems with the irrigation procedure, circumstances for the incident, localization of the perforation, in-hospital treatment, outcomes and causal relationship. Consensus on each case was reached at a joint conference with all reviewers represented. The Coloplast coauthor (BPJ) was not involved in the review process or in the data analysis.
Causality
To define causality between the reported perforation and the use of Peristeen Anal Irrigation®, the WHO system was applied using six categories [8] Certain—‘cannot be explained otherwise,’ Probably/Likely—‘unlikely to be attributed to other factors,’ Possible—‘could also be explained by other factors,’ Unlikely—‘relationship improbable but not impossible, other factors provide plausible explanation,’ Conditional—‘more data needed’ or ‘data under examination,’ Un-assessable—‘report suggest a relationship, data is insufficient.’
Statistical analysis
To explore special patient characteristics and procedure-related factors, cases were subdivided into neurogenic bowel dysfunction, non-neurogenic bowel dysfunction and ‘unknown.’ An early case was defined as an incident within 8 weeks of treatment initiation. Data were entered and analyzed using SPSS 21.0. Data analysis was descriptive.
Results
From 2005 until ultimo 2013, Coloplast received 49 reports of bowel perforation in connection with use of Peristeen Anal Irrigation® (20 males, 27 females, 2 no gender information, median age 60 years, range 9–84 years). Reports were received from ten countries (Germany 15, UK 14, France 8, The Netherlands 3, Italy 3, Finland 2, Sweden 1, Norway 1, Australia 1, Denmark 1). Based on the yearly sales of catheters, the overall average risk of perforation was 6 per million procedures. In the last 2-year period, the incidence had fallen to less than 2 per million procedures.
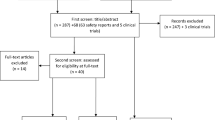
The flow sheet of the global audit and the assessed causal relationship between the incident and the use of Peristeen Anal Irrigation® system is displayed in Fig. 1. Forty-nine reports were evaluated. In three cases, the data quality was too low to make any assessment and they were therefore categorized as ‘un-assessable’ and not included in the subsequent analysis.
For the remaining 46 evaluable cases, data regarding bowel dysfunction etiology, location of the perforation, complainant, pretreatment evaluation and training are presented in Table 1. Neurogenic bowel dysfunction was the indication for commencing irrigation in 26 (57 %) cases, and 15 (33 %) were treated for non-neurogenic bowel symptoms. In five (15 %) cases, no information about etiology was available.
The location of the perforation, surgical treatment and the outcome at follow-up are presented in Table 2. Rectal perforation was reported in 21 (46 %) cases, rectosigmoid or sigmoid perforation in 13 (28 %) cases, and in 12 (26 %) cases no precise information was available. Eighteen cases were considered intraperitoneal, 14 cases extraperitoneal and in 14 cases no precise information was available. In 38 (83 %) cases, an emergency operation was performed. Six (13 %) cases were treated conservatively, and in two (4 %) cases, there was no information. At follow-up, 30 (65 %) cases had an enterostoma, while 9 (20 %) had recovered without a permanent stoma. Outcome was unknown in four (9 %) cases. Three (7 %) patients died in hospital. In two of these fatal cases, severe comorbidity and off-label use were contributing factors to both the incident and the fatal outcome. In the third fatal case, detailed medical history and hospital records were not available.
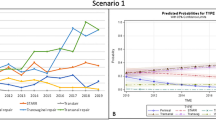
The yearly number of reported bowel perforations since 2005 is shown in Fig. 2. Reports received as from January 2012 represent the redesigned catheter, introduced together with a revised IFU and intensified training programs.
Table 3 and Fig. 3 show that in 29 out of 43 (67 %) cases with relevant information available, the perforation occurred during the first 8 weeks after treatment initiation. Table 3 further presents possible contributing factors that include previous pelvic organ surgery (15 cases) and rectal balloon burst (11 cases).
Discussion and conclusions
The present study describes the profile of reported bowel perforations related to transanal irrigation. The medical device manufacturer Coloplast, who has marketed the Peristeen Anal Irrigation® system since 2005, has given the authors uncensored access to all available information concerning the perforation cases reported to their Vigilance Department. This provided unique and original global data to examine bowel perforations related to transanal irrigation, as exemplified by the Peristeen system.
Facing a collection of 49 cases of bowel perforation, it is important to emphasize the global context of the data collection, the time span of 9 years and the millions of irrigation procedures performed worldwide since the introduction of the system. The weighted average risk of a bowel perforation was 6 per million (1:167.000) irrigation procedures. The incidence of reported event per country reflects the overall sales of Peristeen Anal Irrigation®, with Germany, UK and France being the largest markets.
During the whole investigational period, two out of three perforations occurred within the first 8 weeks of treatment. The overrepresentation of early cases illustrates that the risk is not cumulative. This is highly relevant, given that most indications for irrigation require life-long treatment. For comparison, the standard quoted risk of perforation is 20 per million irrigation procedures (all irrigation systems) [5], 1:40.000 during flexible sigmoidoscopy [9], 1:1.000 during colonoscopy [10] and 1:10.000 during barium enema procedures [11]. In a substantial proportion of patients scheduled for transanal irrigation, the treatment alternative is a colostomy. For comparison, elective colorectal surgery carries a 30-day mortality risk of approximately 2 % [12, 13].
From a clinical point of view, it is important to distinguish between bowel perforation below the peritoneal reflection, retroperitoneal perforation and intraperitoneal perforation, because symptoms, treatment and prognosis differ substantially. The most serious condition is intraperitoneal perforation with generalized peritonitis and fecal contamination A resection of the lacerated segment is required [11, 14, 15], and in most such cases, a primary anastomosis is avoided for safety reasons, and a sigmoid colostomy has to be performed.
In the present paper, 18 cases were classified as intraperitoneal perforations, 14 were sub- or retroperitoneal, while 14 remain undetermined from the available records. In 34 out of 46 cases (74 %), a sigmoid resection was performed and a colostomy or ileostomy was created. As acute colorectal surgery is a life-threatening condition with 30-day mortality of 22 % [16], fatal cases must be expected (7 %) as illustrated by the three presented in the present paper. However, in two of the fatal cases, both severe comorbidity and off-label use of the irrigation system contributed to the incident and the fatal outcome.
Perforation into the retroperitoneal space or into the extraperitoneal perirectal space may be limited and pass unrecognized. If recognized and if symptoms are mild, the condition may be treated with intravenous broad-spectrum antibiotics, close observation and drainage if necessary [17, 18]. In more severe cases of retroperitoneal perforation, the treatment regimen is the same as for intraperitoneal perforation. In the present paper, 14 out of 46 cases (30 %) were retroperitoneal or extraperitoneal perirectal perforation. In 6 out of 14 (43 %) cases with retroperitoneal/extraperitoneal perforation, treatment was with antibiotics and drainage only without further surgery, and patients recovered uneventfully.
In theory, an impaling trauma following catheter insertion will be located in the rectum. A possible concomitant factor using an irrigation system with a rectal balloon is perforation due to balloon distension or rupture of the balloon. Rupture of the balloon could induce a high-pressure wave transmitted to the bowel wall, which could contribute to a perforation. However, the exact mechanism remains unclear.
In 2012, Coloplast introduced a redesigned softer rectal catheter with a new balloon. Together with these product adjustments, the IFU was through revision, the list of absolute and relative contraindications was sharpened, and intensified company-based nurse education was strengthened with a focus on safety. In Fig. 3, there is a drop in the reported incidence of perforation in 2012–2013 with a yearly perforation rate less than 2 per million procedures. The exact reason is unclear, but is likely to represent a reduced risk with use of the Peristeen system.
Two-thirds of perforations happened within the first 8 weeks. This could be due to the mechanical properties of the bowel. If the patient has a fragile bowel wall due to scarring from prior rectal surgery or even a rectal anastomosis, irradiation or diverticular disease, this would put the patient at risk. In patients with their initial bowel problems categorized as of non-neurogenic origin, 11 out of 15 had had surgery to the pelvic organs sometime before the start of treatment. Residual functional problems after rectal surgery are common. Following rectal resection for treatment rectal cancer, more than 80 % report some kind of change in bowel habits, and 45 % have bowel problems with severe impact on quality of life, termed as low anterior resection syndrome [19]. Transanal irrigation is an efficient treatment for this syndrome [7], but the neorectum and the surroundings of the anastomose have abnormal biomechanical properties compared to a non-operated rectum making the bowel wall more fragile. The same is probably true for other types of rectal surgery such as the stapled transanal rectal resection or ventral mesh rectopexy for obstructed defecation [15], and any kind of surgery for rectal prolapse. While it is possible that the observed perforation rate in this cohort could be due to selection bias, the apparent increased risk in patients with prior rectal surgery emphasizes that pretreatment endoscopic evaluation of the rectum is mandatory in such patients [3]. Furthermore, patients should be informed of the increased risk. In such cases, the balloon should only be inflated to a minimum if at all necessary.
Based on common sense, a set of absolute and relative contraindications has been listed [3]. Diverticular disease was present in five of our cases (11 %), and this is not more than expected from the prevalence in the general population. The same accounts for the few cases reported treated with corticosteroids and anticoagulants.
It is well accepted that it takes 6–8 weeks after initial training before the patient becomes familiar with all practical issues related to self-administration of irrigation treatment [3]. An important step toward successful treatment is training with an experienced and suitably trained nurse before initiation of the treatment. Furthermore, close contact with the training unit is recommended in the initial phase not only to adjust the efficacy but also of safety concern since forceful administration put the patient at risk. In the present data, the majority of patients had had some kind of nurse-led training before treatment initiation, but the precise level of training was unknown in most cases.
Since bowel perforation is such a rare event, each institution treating patients with transanal irrigation will very seldom face an incidence if at all. The National Health Authorities will only have few cases accumulated through years without possibility to draw conclusion regarding the safety profile. No information on systematic survey of other manufactures of systems for transanal irrigation could be found. Some information can be found within the public lists of device-related events [www.patientsville.com (assessed Nov 26, 2014)] or [www.fda.gov/MedicalDevices (assessed Nov 29, 2014)], but these may suffer from underreporting from device companies and institutions not willing to expose their failures. Moreover, most medical journals have abandoned publication of case reports. Those few reports available in the literature of bowel perforations due to transanal irrigation report use of rigid rectal tube [14, 17] and other rectal balloon catheters [5, 11], and two reports are on Peristeen Anal Irrigation [15, 18].
In a clinical audit in a hospital setting or an audit initiated from the health authorities, the investigators will have full access to hospital records with no legal barriers. This is in sharp contrast to the conditions for the present study, where data have been collected by the company without any direct contact to the data source. In the majority of cases, data had been reported from a nurse or doctor (complainant) involved in training or treatment of the patient. In only a few cases, the company had been given access to the hospital files. Furthermore, both the Coloplast subsidiaries and the Vigilance Department had to rely on the willingness of the information source to provide the information. The complainant could have been involved in the case, and the degree of underreporting is unknown. The authors therefore had to accept missing data within cases and some inconsistency of data over time. The data therefore suffer from substantial selection bias and information bias, which limits the conclusions that can be drawn. However, the present data reveal useful patterns and trends, strong enough to generate hypotheses to advise clinical practice for treatment with transanal irrigation, and provide important clinical insight into patient-related factors. The advice generated fully supports those described in a recent Consensus Review [3].
In summary, transanal irrigation is a simple therapeutic method for management of fecal incontinence and constipation in selected patient groups. It improves quality of life and socialization and carries a low risk of irrigation-induced bowel perforation. Previously, the incidence of bowel perforation has been estimated to 20 per million irrigation procedures (all irrigation systems) [5]. This study on Peristeen data indicates a much lower risk of bowel perforation, with the latest two-year data indicating an incidence of 2 per million procedures. This per se increases the benefit risk ratio considerable and is supportive for the use of transanal irrigation. Moreover, the present data indicate that further improving the safety of the technique is dependent on careful patient selection, early patient motivation and respect of the absolute and relative contraindications. Healthcare professionals experienced in the field of transanal irrigation should instruct patients to ensure proper handling of the catheter, and advise on how to achieve best results as well as provide information about side effects and the potential risk of perforation. Early cases of perforations account for two out of three reports. These early cases could be considered ‘avoidable’ cases if patient selection and training were optimal. In contrast, perforations during long-term use occur in less than 2 per million procedures which may reflect the innate risk of inserting a semirigid catheter in the rectum, inflating a balloon and installing water. The number of cases should of course be reduced to a minimum, but some kind of acceptance of the low risk of occurrence must be realized and incorporated into patient counseling.
References
Shandling B, Gilmour RF (1987) The enema continence catheter in spina bifida: successful bowel management. J Pediatr Surg 22:271–273
Christensen P, Bazzocchi G, Coggrave M et al (2006) A randomized, controlled trial of transanal irrigation versus conservative bowel management in spinal cord-injured patients. Gastroenterology 131:738–747
Emmanuel AV, Krogh K, Bazzocchi G et al (2013) Consensus review of best practice of transanal irrigation in adults. Spinal Cord 51:732–738
Christensen P, Olsen N, Krogh K, Bacher T, Laurberg S (2003) Scintigraphic assessment of retrograde colonic washout in fecal incontinence and constipation. Dis Colon Rectum 46:68–76
Christensen P, Krogh K, Buntzen S, Payandeh F, Laurberg S (2009) Long-term outcome and safety of transanal irrigation for constipation and fecal incontinence. Dis Colon Rectum 52:286–292
Preziosi G, Gosling J, Raeburn A, Storrie J, Panicker J, Emmanuel A (2012) Transanal irrigation for bowel symptoms in patients with multiple sclerosis. Dis Colon Rectum 55:1066–1073
Rosen H, Robert-Yap J, Tentschert G, Lechner M, Roche B (2011) Transanal irrigation improves quality of life in patients with low anterior resection syndrome. Colorectal Dis 13:e335–e338
Meyboom RH, Hekster YA, Egberts AC, Gribnau FW, Edwards IR (1997) Causal or casual? The role of causality assessment in pharmacovigilance. Drug Saf 17:374–389
Atkin WS, Cook CF, Cuzick J, Edwards R, Northover JM, Wardle J (2002) Single flexible sigmoidoscopy screening to prevent colorectal cancer: baseline findings of a UK multicentre randomised trial. Lancet 359:1291–1300
Loffeld RJ, Engel A, Dekkers PE (2011) Incidence and causes of colonoscopic perforations: a single-center case series. Endoscopy 43:240–242
Gedebou TM, Wong RA, Rappaport WD, Jaffe P, Kahsai D, Hunter GC (1996) Clinical presentation and management of iatrogenic colon perforations. Am J Surg 172:454–457
Iversen LH, Ingeholm P, Gogenur I, Laurberg S (2014) Major reduction in 30-day mortality after elective colorectal cancer surgery: a nationwide population-based study in Denmark 2001–2011. Ann Surg Oncol 21:2267–2273
Billeter AT, Polk HC Jr, Hohmann SF et al (2012) Mortality after elective colon resection: the search for outcomes that define quality in surgical practice. J Am Coll Surg 214:436–443 (discussion 43-44)
Gayer G, Zissin R, Apter S, Oscadchy A, Hertz M (2002) Perforations of the rectosigmoid colon induced by cleansing enema: CT findings in 14 patients. Abdom Imaging 27:453–457
Memon S, Bissett IP (2014) Rectal perforation following transanal irrigation. ANZ J Surg. doi:10.1111/ans.12761
Iversen LH, Bulow S, Christensen IJ, Laurberg S, Harling H (2008) Postoperative medical complications are the main cause of early death after emergency surgery for colonic cancer. Br J Surg 95:1012–1049
Paran H, Butnaru G, Neufeld D, Magen A, Freund U (1999) Enema-induced perforation of the rectum in chronically constipated patients. Dis Colon Rectum 42:1609–1612
Biering-Sorensen F, Bing J, Berggreen P, Olesen GM (2009) Rectum perforation during transanal irrigation: a case story. Spinal Cord 47:266–267
Emmertsen KJ, Laurberg S (2012) Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg 255:922–928
Funding
The study has not been financially supported.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Peter Christensen has served as a consultant and an advisory board member for Coloplast, and as an advisory board member for Wellspect Health Care. Klaus Krogh has served as an advisory board member for Coloplast and Wellspect Health Care. Brigitte Perrouin-Verbe has served as an advisory board member for Coloplast. Dietrich Leder has served as an advisory board member for Coloplast and Wellspect Health Care. Gabriele Bazzocchi has served as an advisory board member for Coloplast and Wellspect Health Care. Birte Petersen Jakobsen is an employee of Coloplast. Anton Emmanuel has served as a speaker, a consultant and an advisory board member for Coloplast, Hollister and Wellspect Health Care.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Christensen, P., Krogh, K., Perrouin-Verbe, B. et al. Global audit on bowel perforations related to transanal irrigation. Tech Coloproctol 20, 109–115 (2016). https://doi.org/10.1007/s10151-015-1400-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-015-1400-8