Abstract
Objective
To evaluate masticatory function in individuals with Parkinson’s disease (PD) during levodopa “on” period using new removable dental prosthesis.
Materials and methods
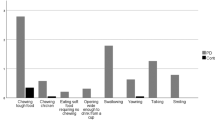
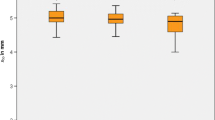
A total of 34 elderly individuals with PD (n = 17, mean age = 69.41 ± 4.65 years) or without PD (n = 17, mean age = 70.71 ± 4.65 years) were recruited for this study. Participants received new complete dentures and/or removable partial dentures. Two months after the subjects were free of any prostheses discomfort, masticatory function was assessed. A kinesiographic device was used to measure the range of jaw motion and jaw movements while chewing a silicone test material (Optocal). Masticatory performance was determined by median particle size (X50) of the Optocal after 40 masticatory cycles. Maximum bite force was assessed by a strain sensor placed in the bilateral first molars region. Data were analyzed by t test (P < 0.05).
Results
The PD group showed a decreased range of jaw motion, longer duration and slower velocity of the masticatory cycle (P < 0.05), higher X50 value, and lower maximum bite force (P < 0.05).
Conclusion
PD patients have impaired masticatory function during levodopa “on” periods compared to controls.
Clinical relevance
Knowledge that PD is associated with impaired masticatory function is important to dental professionals in decision making related to prosthetics and general dental treatment.

Similar content being viewed by others
References
Westberg K-G, Kolta A (2011) The trigeminal circuits responsible for chewing. Int Rev Neurobiol 97:77–98
van der Bilt A (2011) Assessment of mastication with implications for oral rehabilitation: a review. J Oral Rehabil 38(10):754–780
Avivi-Arber L, Lee JC, Sessle BJ (2011) Face sensorimotor cortex neuroplasticity associated with intraoral alterations. Prog Brain Res 188:135–150
Lin C-S, Wu S-Y, Wu C-Y, Ko H-W (2016) Gray matter volume and resting-state functional connectivity of the motor cortex-cerebellum network reflect the individual variation in masticatory performance in healthy elderly people. Front Aging Neurosci 7(5):828–831
Quintero A, Ichesco E, Schutt R, Myers C, Peltier S, Gerstner GE (2013) Functional connectivity of human chewing: an fcMRI study. J Dent Res 92(3):272–278
Avivi-Arber L, Martin R, Lee JC, Sessle BJ (2011) Face sensorimotor cortex and its neuroplasticity related to orofacial sensorimotor functions. Arch Oral Biol 56(12):1440–1465
Friedlander AH, Mahler M, Norman KM, Ettinger RL (2009) Parkinson disease: systemic and orofacial manifestations, medical and dental management. J Am Dent Assoc 140(6):658–669
Robertson LT, Hammerstad JP (1996) Jaw movement dysfunction related to Parkinson’s disease and partially modified by levodopa. J Neurol Neurosurg Psychiatry 60(1):41–50
Gazewood JD, Richards DR, Clebak K (2013) Parkinson disease: an update. Am Fam Physician 87(4):267–273
Karlsson S, Persson M, Johnels B (1992) Levodopa induced ON-OFF motor fluctuations in Parkinson ’ s disease related to rhythmical masticatory aw movements. J Neurol Neurosurg Psychiatry 55:304–307
Hatch JP, Shinkai RS, Sakai S, Rugh JD, Paunovich ED (2001) Determinants of masticatory performance in dentate adults. Arch Oral Biol 46(7):641–648
Ikebe K, Matsuda K, Kagawa R, Enoki K, Okada T, Yoshida M, et al. (2012) Masticatory performance in older subjects with varying degrees of tooth loss. J Dent 40(1):71–76. doi:10.1016/j.jdent.2011.10.007
Bakke M, Larsen SL, Lautrup C, Karlsborg M (2011) Orofacial function and oral health in patients with Parkinson’s disease. Eur J Oral Sci 119(1):27–32. doi:10.1111/j.1600-0722.2010.00802.x
Liedberg B, Norlén P, Owall B, Stoltze K (2004) Masticatory and nutritional aspects on fixed and removable partial dentures. Clin Oral Investig 8(1):11–17
Clifford T, Finnerty J (1995) The dental awareness and needs of a Parkinson’s disease population. Gerodontology 12(2):99–103
Nakayama Y, Washio M, Mori M (2004) Oral health conditions in patients with Parkinson’s disease. J Epidemiol 14(5):143–150
Lorefält B, Granérus AK, Unosson M (2006) Avoidance of solid food in weight losing older patients with Parkinson’s disease. J Clin Nurs 15(11):1404–1412
van der Bilt A, Olthoff LW, Bosman F, Oosterhaven SP (1994) Chewing performance before and after rehabilitation of post-canine teeth in man. J Dent Res 73(11):1677–1683
Vigild M (1987) Denture status and need for prosthodontic treatment among institutionalized elderly in Denmark. Community Dent Oral Epidemiol 15:128–133
Folstein MF, Folstein SE, McHugh PR (1975) “mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Bertolucci PH, Brucki SM, Campacci SR, Juliano Y (1994) O mini-Exame do Estado mental em uma população geral. Impacto da escolaridade. Arq Neuropsiquiatr 52(1):1–7
Rompré PH, Daigle-Landry D, Guitard F, Montplaisir JY, Lavigne GJ (2007) Identification of a sleep bruxism subgroup with a higher risk of pain. J Dent Res 86(9):837–842
Dworkin SF, LeResche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 6(4):301–355
Slagter AP, Olthoff LW, Steen WH, Bosman F (1992) Comminution of food by complete-denture wearers. J Dent Res 71(2):380–386
Reichmann H (2010) Clinical criteria for the diagnosis of Parkinson’s disease. Neurodegener Dis 7(5):284–290
Zarb GA, Hobkirk J, Eckert S, Jacob R (2013) Prosthodontic treatment for edentulous patients. Mosby, St Louis
Carr A, Brown D (2011) McCracken’s removable partial prosthodontics. Mosby, St Louis
Pocztaruk RDL, Frasca LCDF, Rivaldo EG, Fernandes EDL, Gavião MBD (2008) Protocol for production of a chewable material for masticatory function tests (Optocal - Brazilian version). Braz Oral Res 22(4):305–310
Slagter AP, Bosman F, Van der Bilt A (1993) Comminution of two artificial test foods by dentate and edentulous subjects. J Oral Rehabil 20(2):159–176
Slagter AP, van der Glas HW, Bosman F, Olthoff LW (1992) Force-deformation properties of artificial and natural foods for testing chewing efficiency. J Prosthet Dent 68(5):790–799
Gonçalves TMSV, Campos CH, Rodrigues Garcia RCM (2014) Mastication and jaw motion of partially edentulous patients are affected by different implant-based prostheses. J Oral Rehabil 41(7):507–514. doi:10.1111/joor.12176
Lepley C, Throckmorton G, Parker S, Buschang PH (2010) Masticatory performance and chewing cycle kinematics-are they related? Angle Orthod 80(2):295–301. doi:10.2319/061109-333.1
Custodio W, Gomes SGF, Faot F, Garcia RCMR, Del Bel Cury AA (2011) Occlusal force, electromyographic activity of masticatory muscles and mandibular flexure of subjects with different facial types. J Appl Oral Sci 19(4):343–349
Gonçalves TMSV, Campos CH, Gonçalves GM, de Moraes M, Rodrigues Garcia RCM (2013) Mastication improvement after partial implant-supported prosthesis use. J Dent Res 92(12 Suppl):189S–194S. doi:10.1177/0022034513508556
van Der Bilt A, Tekamp A, van Der Glas H, Abbink J (2008) Bite force and electromyograpy during maximum unilateral and bilateral clenching. Eur J Oral Sci 116(3):217–222. doi:10.1111/j.1600-0722.2008.00531.x
McGrath C, Bedi R (1999) The importance of oral health to older people’s quality of life. Gerodontology 16(1):59–63
Heckmann SM, Heckmann JG, Weber HP (2000) Clinical outcomes of three Parkinson’s disease patients treated with mandibular implant overdentures. Clin Oral Implants Res 11(6):566–571
Woda A, Foster K, Mishellany A, Peyron MA (2006) Adaptation of healthy mastication to factors pertaining to the individual or to the food. Physiol Behav 89(1):28–35
Trulsson M (2006) Sensory-motor function of human periodontal mechanoreceptors. J Oral Rehabil 33(4):262–273
Adachi K, Kobayashi M, Kawasaki T, Yokoyama C, Waddington JL, Sakagami H, et al. (2012) Disruption of programmed masticatory movements in unilateral MPTP-treated monkeys as a model of jaw movement abnormality in Parkinson’s disease. J Neural Transm 119(8):933–941. doi:10.1007/s00702-012-0768-0
Potulska A, Friedman A, Królicki L, Spychala A (2003) Swallowing disorders in Parkinson’s disease. Parkinsonism Relat Disord 9(6):349–353
van der Bilt A, Burgers M, van Kampen FMC, Cune MS (2010) Mandibular implant-supported overdentures and oral function. Clin Oral Implants Res 21(11):1209–1213. doi:10.1111/j.1600-0501.2010.01915.x
Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, Van ’T Hof MA, Witter DJ, Kalk W, et al. (2000) Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res 79(7):1519–1524
Olthoff LW, Van Der Glas HW, Van Der Bilt A (2007) Influence of occlusal vertical dimension on the masticatory performance during chewing with maxillary splints. J Oral Rehabil 34(8):560–565
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17(5):427–442
Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease (2003) The Unified Parkinson’s Disease Rating Scale (UPDRS): status and recommendations. Mov Disord 18(7):738–750
Acknowledgments
This study was supported by the National Council of Technological and Scientific Development (CNPq, grant number 48.090.3/2013-1) and São Paulo Research Foundation (FAPESP, grant number 2012/15223-2), Brazil. The authors thank Felipe Nogueira Anacleto and Guilherme Henrique Costa Oliveira from the Piracicaba Dental School, University of Campinas, São Paulo, Brazil, for their assistance with endodontic and periodontal treatments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the National Council of Technological and Scientific Development (CNPq, grant number 48.090.3/2013–1) and São Paulo Research Foundation (FAPESP, grant number 2012/15223–2), Brazil.
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures in this research were performed in accordance with the ethical standards of the Ethics Committee of Piracicaba dental School, University of Campinas and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ribeiro, G.R., Campos, C.H. & Rodrigues Garcia, R.C.M. Parkinson’s disease impairs masticatory function. Clin Oral Invest 21, 1149–1156 (2017). https://doi.org/10.1007/s00784-016-1879-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1879-z