Abstract
Background
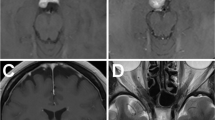
Cerebellopontine angle tumor resection and cranial nerve microvascular decompression are usually performed with the aid of the surgical microscope. The endoscope is commonly used as an adjuvant.
Method
A retrosigmoid craniectomy is done. Upon dural opening, the endoscope is inserted into the operative field along the petrotentorial junction. Cerebrospinal fluid drainage provides a wider space for introduction of the endoscope and surgical instruments. Traditional microsurgical techniques are used during the entire procedure.
Conclusion
A fully endoscopic retrosigmoid approach is a safe and effective procedure for cerebellopontine angle tumor resection and cranial nerve microvascular decompression.
Key points
• Careful examination of preoperative studies is needed to identify anatomical peculiarities.
• Patient positioning: the head must be gently flexed and its vertex gently tilted toward the floor.
• Neurophysiologic monitoring and intraoperative navigation.
• Craniectomy: partial exposure of the transverse and sigmoid sinuses.
• Curvilinear dural incision reflected laterally to minimize the risk of sinus injury.
• Opening the cerebellomedullary cistern for CSF drainage and cerebellar relaxation.
• Dynamic endoscopy enhances depth perception and must be performed by a team with experience in endoscopic intracranial surgery.
• Traditional microsurgical techniques have to be applied during the entire operation.
• Multilayer reconstruction, including watertight dural closure.
• Meningiomas causing brainstem shift are not suitable for endoscopic resection.





Similar content being viewed by others
References
Ribas GC, Rhoton AL Jr, Cruz OR, Peace D (2005) Suboccipital burr holes and craniectomies. Neurosurg Focus 19(2):E1
Rhoton AL Jr (2000) The cerebellopontine angle and posterior fossa cranial nerves by the retrosigmoid approach. Neurosurgery 47:93–129
Rhoton A Jr (2003) Operative techniques and instrumentation for neurosurgery. Neurosurgery 53(4):907–934
McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, Resnick DK (1999) Microvascular decompression of cranial nerves: lessons learned after 4400 operations. J Neurosurg 90:1–8
Matsushima K, Matsushima T, Kuga Y, Kodama Y, Inoue K, Ohnishi H, Rhoton AL Jr (2014) Classification of the superior petrosal veins and sinus based on drainage pattern. Neurosurgery 10(Suppl 2):357–367
Shulev Y, Trashin A, Gordienko K (2011) Secondary trigeminal neuralgia in cerebellopontine angle tumors. Skull Base 21(5):287–294
Conflict of interest
All authors certify that they have NO affiliations or involvement with any organization or entity with any financial interest (such as honoraria; educational grants; participation in speaker’s bureau; membership, employment, consultancies, stock ownership or other equity interest; and expert testimony of patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
The content of this manuscript and attached video illustrates the modularity of full endoscopic techniques in the field of skull base lesions. We see here how the structures can be exposed and how the endoscope can help to look around the corners. Does it mean that operating in this way will allow the achievement of better resection with less morbidity and smaller exposure of posterior petrous bone meningiomas? Those who master the regular microsurgical techniques will only be convinced by additional clinical studies; moreover, the next generation of skull base surgeons will still need to learn the regular techniques before launching their own practice with the endoscope. We have to congratulate the authors for this excellent contribution.
Pierre-Hugues Roche
Marseille,France
This work has not been presented at any medical conference.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video 1: Fully endoscopic retrosigmoid approach for posterior petrous meningioma and trigeminal microvascular decompression (MOV 235179 kb)
Rights and permissions
About this article
Cite this article
Vaz-Guimaraes, F., Gardner, P.A. & Fernandez-Miranda, J.C. Fully endoscopic retrosigmoid approach for posterior petrous meningioma and trigeminal microvascular decompression. Acta Neurochir 157, 611–615 (2015). https://doi.org/10.1007/s00701-014-2332-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2332-1