Abstract
Purpose
Neurocognitive impairment is frequently observed among acute lymphoblastic leukemia (ALL) survivors within the domains of intelligence, attention, processing speed, working memory, learning, and memory. However, few have investigated treatment-induced changes in neurocognitive function during the first months of treatment. Additionally, dysfunction during treatment may be preceded by changes in biomarkers measured within cerebrospinal fluid (CSF). Identification of acute declines in neurocognitive function, as well as predictive genotypes or biomarkers, could guide therapeutic trials of protective interventions.
Methods
This study collects CSF while prospectively assessing neurocognitive functioning (working memory, executive function, learning, processing speed, and attention) of ALL patients using the Cogstate computerized battery at six time points during and after the 2 years of leukemia treatment on a Dana-Farber Cancer Institute ALL Consortium trial.
Results
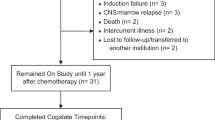
Baseline data collected during the first 3 weeks of induction chemotherapy indicate reliable data as all subjects (N = 34) completed Cogstate baseline testing, while completion and performance checks indicate that 100 % of subjects completed testing and complied with test requirements. The majority (85 %) exhibited normal function compared with age peers. Preliminary analysis of CSF biomarkers (folate, homocysteine, 8-isoprostane, and myelin basic protein) similarly reveals values at baseline within expected normal ranges.
Conclusions
The first month of induction therapy for ALL is a reliable baseline for detecting treatment-induced changes in neurocognitive functioning. Consequently, serial data collection might identify subgroups of ALL patients at increased risk for neurocognitive decline, warranting proactive interventions to improve their level of functioning both during treatment and into survivorship.



Similar content being viewed by others
References
Peterson CC, Johnson CE, Ramirez LY, Huestis S, Pai ALH, Demaree HA et al (2008) A meta-analysis of the neuropsychological sequelae of chemotherapy-only treatment for pediatric acute lymphoblastic leukemia. Pediatr Blood Cancer 51:99–104
Conklin HM, Krull KR, Reddick WE, Pei D, Cheng C, Pui CH (2012) Cognitive outcomes following contemporary treatment without cranial irradiation for childhood acute lymphoblastic leukemia. J Natl Cancer Inst 104:1386–1395
Wefel J, Schagen S (2012) Chemotherapy-related cognitive dysfunction. Curr Neurol Neurosci Rep 12:267–275
Waber DP, Queally JT, Catania L, Robaey P, Romero I, Adams H et al (2011) Neuropsychological outcomes of standard risk and high risk patients treated for acute lymphoblastic leukemia on Dana-Farber ALL consortium protocol 95-01 at 5 years post-diagnosis. Pediatr Blood Cancer. doi:10.1002/pbc.23234
Kadan-Lottick NS, Zeltzer LK, Liu Q, Yasui Y, Ellenberg L, Gioia G et al (2010) Neurocognitive functioning in adult survivors of childhood non-central nervous system cancers. J Natl Cancer Inst 102:881–893
Buizer AI, de Sonneville LM, Veerman AJ, Buizer AI, de Sonneville LMJ, Veerman AJP (2009) Effects of chemotherapy on neurocognitive function in children with acute lymphoblastic leukemia: a critical review of the literature. Pediatr Blood Cancer 52:447–454
Lofstad GE, Reinfjell T, Hestad K, Diseth TH, Lofstad GE, Reinfjell T et al (2009) Cognitive outcome in children and adolescents treated for acute lymphoblastic leukaemia with chemotherapy only. Acta Paediatr 98:180–186
Krull KR, Hockenberry MJ, Miketova P, Carey M, Moore IM (2013) Chemotherapy-related changes in central nervous system phospholipids and neurocognitive function in childhood acute lymphoblastic leukemia. Leuk Lymphoma 54:535–540
Ficek K, Blamek S, Sygula D, Miszczyk L, Sonta-Jakimczyk D, Tarnawski R (2010) Evaluation of the late effects of CNS prophylactic treatment in childhood acute lymphoblastic leukemia (ALL) using magnetic resonance spectroscopy. Acta Neurochir Suppl 106:195–197
Krull KR, Bhojwani D, Conklin HM, Pei D, Cheng C, Reddick WE et al (2013) Genetic mediators of neurocognitive outcomes in survivors of childhood acute lymphoblastic leukemia. J Clin Oncol 31:2182–2188
Jankovic M, Brouwers P, Valsecchi MG et al (1994) International Study Group on Psychosocial Aspects of Childhood Cancer: association of 1800 cGy cranial irradiation with intellectual function in children with acute lymphoblastic leukaemia. ISPACC Lancet 344:224–227
Langer T, Martus P, Ottensmeier H et al (2002) CNS late effects after ALL therapy in childhood. Part III: neuropsychological performance in long-term survivors of childhood ALL: impairments of concentration, attention and memory. Med Pediatr Oncol 38:320–328
Cheung YT, Krull KR (2015) Neurocognitive outcomes in long term survivors of childhood acute lymphoblastic leukemia treated on contemporary treatment protocols: a systematic review. Neurosci Biobehav Rev 53:108–120
Iyer NS, Balsamo LM, Bracken MB et al (2015) Chemotherapy-only treatment effects on long-term neurocognitive functioning in childhood ALL survivors: a review and meta-analysis. Blood 126:346–353
Buizer AI, de Sonneville LM, van den Heuvel-Eibrink MM et al (2006) Behavioral and educational limitations after chemotherapy for childhood acute lymphoblastic leukemia or Wilms tumor. Cancer 106:2067–2075
Kunin-Batson A, Kadan-Lottick N, Neglia JP (2014) The contribution of neurocognitive functioning to quality of life after childhood acute lymphoblastic leukemia. Psychooncology 23:692–699
Campbell LK, Scaduto M, Van Slyke D, Niarhos F, Whitlock JA, Compas BE et al (2009) Executive function, coping, and behavior in survivors of childhood acute lymphocytic leukemia. J Pediatr Oncol 34:317–327
Kadan-Lottick NS, Brouwers P, Breiger D, Kaleita T, Dziura J, Northrup V et al (2009) Comparison of neurocognitive functioning in children previously randomly assigned to intrathecal methotrexate compared with triple intrathecal therapy for the treatment of childhood acute lymphoblastic leukemia. J Clin Oncol 27:5986–5992
Ashford J, Schoffstall C, Reddick WE, Leone C, Laningham FH, Glass JO et al (2010) Attention and working memory abilities in children treated for acute lymphoblastic leukemia. Cancer 116:4638–4645
Hodgson KD, Hutchinson AD, Wilson CJ, Nettelbeck T (2013) A meta-analysis of the effects of chemotherapy on cognition in patients with cancer. Cancer Treat Rev 39:297–304
Buizer AI, de Sonneville LM, van den Heuvel-Eibrink MM et al (2005) Chemotherapy and attentional dysfunction in survivors of childhood acute lymphoblastic leukemia: effects of treatment intensity. Pediatr Blood Cancer 45:281–290
Conklin HM, Krull KR, Reddick WE et al (2012) Cognitive outcomes following chemotherapy treatment without cranial irradiation for childhood acute lymphoblastic leukemia. J Natl Cancer Inst 104:1386–1395
Buizer AI, de Sonneville LM, van de Heuevel-Eibrink MM et al (2005) Visoumotor control in survivors of acute lymphoblastic leukemia treated with chemotherapy only. J Int Neuropsychol Soc 11:554–565
Kingma A, van Dommelen RI, Mooyaart EL et al (2001) Slight cognitive impairment and magnetic resonance imaging abnormalities but normal school levels in children treated for acute lymphoblastic leukemia with chemotherapy only. J Pediatr 139:413–420
von der Weid N, Mosimann I, Hirt A et al (2003) Intellectual outcome in children and adolescents with acute lymphoblastic leukemia treated with chemotherapy along: age- and sex-related differences. Eur J Cancer 39:359–365
Jain N, Brouwers P, Okcu MF et al (2009) Sex-specific attention problems in long-term survivors of pediatric acute lymphoblastic leukemia. Cancer 115:4238–4245
Harila MJ, Winqvist S, Lanning M, Bloigu R, Harila-Saari AH, Harila MJ et al (2009) Progressive neurocognitive impairment in young adult survivors of childhood acute lymphoblastic leukemia. Pediatr Blood Cancer 53:156–161
Waber DP, McCabe M, Sebree M, Forbes PW, Adams H, Alyman C (2013) et al. Neuropsychological outcomes of a randomized trial of prednisone versus dexamethasone in acute lymphoblastic leukemia: Findings from Dana-Farber Cancer Institute All Consortium Protocol 00-01. Pediatr Blood Cancer
Jacola LM, Krull KR, Pui C-H, Pei D, Cheng C, Reddick WE et al (2016) Longitudinal assessment of neurocognitive outcomes in survivors of childhood acute lymphoblastic leukemia treated on a contemporary chemotherapy protocol. J Clin Oncol 34:1239–1247
Cole PD, Vijayanathan V, Ali NF, Wagshul ME, Tanenbaum EJ, Price J et al (2013) Memantine protects rats treated with intrathecal methotrexate from developing spatial memory deficits. Clin Cancer Res 19:4446–4454
Li Y, Vijayanathan V, Gulinello M, Cole PD (2010) Intrathecal methotrexate induces focal cognitive deficits and increases cerebrospinal fluid homocysteine. Pharmacol Biochem Behav 95:428–433
Li Y, Vijayanathan V, Gulinello ME, Cole PD (2010) Systemic methotrexate induces spatial memory deficits and depletes cerebrospinal fluid folate in rats. Pharmacol Biochem Behav 94:454–463
Vijayanathan V, Ali N, Gulinello M, Cole PD (2011) Persistent cognitive deficits, induced by intrathecal methotrexate, are associated with elevated CSF concentrations of excitotoxic glutamate analogs and can be reversed by an NMDA antagonist. Behav Brain Res 225:491–497
Cole PD, Beckwith KA, Vijayanathan V, Roychowdhury S, Smith AK, Kamen BA (2009) Folate homeostasis in cerebrospinal fluid during therapy for acute lymphoblastic leukemia. Pediatr Neurol 40:34–41
Cole PD, Finkelstein Y, Stevenson KE, Blonquist TM, Vijayanathan V, Silverman LB et al (2015) Polymorphisms in genes related to oxidative stress are associated with inferior cognitive function after therapy for childhood acute lymphoblastic leukemia. J Clin Oncol 33:2205–2211
Boivin MJ, Busman RA, Parikh SM, Bangirana P, Page CF, Opoka RO et al (2010) A pilot study of the neuropsychological benefits of computerized cognitive rehabilitation in Ugandan children with HIV. Neuropsychology 24:667
Cairney S, Clough A, Jaragba M, Maruff P (2007) Cognitive impairment in aboriginal people with heavy episodic patterns of alcohol use. Addiction 102:909–915
Dingwall KM, Cairney S (2010) Psychological and cognitive assessment of indigenous Australians. Aust N Z J Psychiatry 44:20–30
Lewis MS, Dingwall KM, Berkhout N, Sayers S, Maruff P, Cairney S (2010) Assessment of cognition in an adolescent indigenous population. Aust Psychol 45:123–131
Maruff P, Thomas E, Cysique L, Brew B, Collie A, Snyder P et al (2009) Validity of the CogState brief battery: relationship to standardized tests and sensitivity to cognitive impairment in mild traumatic brain injury, schizophrenia, and AIDS dementia complex. Arch Clin Neuropsychol 24:165–178
Pietrzak RH, Olver J, Norman T, Piskulic D, Maruff P, Snyder PJ (2009) A comparison of the CogState schizophrenia battery and the measurement and treatment research to improve cognition in schizophrenia (MATRICS) battery in assessing cognitive impairment in chronic schizophrenia. J Clin Exp Neuropsychol 31:848–859
Kral TV, Heo M, Whiteford LM, Faith MS (2012) Effects on cognitive performance of eating compared with omitting breakfast in elementary schoolchildren. J Dev Behav Pediatr 33:9–16
Mollica CM, Maruff P, Collie A, Vance A (2005) Repeated assessment of cognition in children and the measurement of performance change. Child Neuropsychol 11:303–310
Falleti MG, Maruff P, Collie A, Darby DG (2006) Practice effects associated with the repeated assessment of cognitive function using the CogState battery at 10-minute, one week and one month test-retest intervals. J Clin Exp Neuropsychol 28:1095–1112
Snyder AM, Maruff P, Pietrzak RH, Cromer JR, Snyder PJ (2008) Effect of treatment with stimulant medication on nonverbal executive function and visuomotor speed in children with attention deficit/hyperactivity disorder (ADHD). Child Neuropsychol 14:211–226
Acknowledgments
Patients were enrolled at the following sites: Columbia University Medical Center, New York, NY; The Children’s Hospital at Montefiore, Bronx, NY; Dana-Farber Cancer Institute/Boston Children’s Hospital, Boston, NY; and Hasbro Children’s Hospital, Providence, RI. This work was supported in part by NIH/NCI R21-CA187226.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest, with the exception of Brian Harel who was an employee and a stockholder of Cogstate until February 2016.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Sands, S.A., Harel, B.T., Savone, M. et al. Feasibility of baseline neurocognitive assessment using Cogstate during the first month of therapy for childhood leukemia. Support Care Cancer 25, 449–457 (2017). https://doi.org/10.1007/s00520-016-3422-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3422-9