Abstract
Purpose
This study aims to clarify the length of home hospice care, family-perceived timing of referrals, and their effects on the family-perceived quality of care and quality of death and dying of terminally ill cancer patients who died at home and identify the determinants of perceived late referrals.
Methods
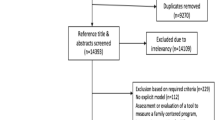
A multicenter questionnaire survey was conducted involving 1,052 family members of cancer patients who died at home supported by 15 home-based hospice services throughout Japan.
Results
A total of 693 responses were analyzed (effective response rate, 66 %). Patients received home-based hospice care for a median of 35.0 days, and 8.0 % received home hospice care for less than 1 week. While 1.5 % of the families reported the timing of referrals as early, 42 % reported the timing as late or too late. The families of patients with a length of care of less than 4 weeks were more likely to regard the timing of referrals as late or too late. The patients of family members who regarded the timing of referrals as late or too late had a significantly lower perceived quality of care (effect size, 0.18; P = 0.039) and lower quality of death and dying (effect size, 0.15, P = 0.063). Independent determinants of higher likelihoods of perceived late referrals included: frequent visits to emergency departments, patient being unprepared for worsening condition, and patient having concerns about relationship with new doctor. Discharge nurse availability was independently associated with lower likelihoods of perceived late referrals.
Conclusions
A significant number of bereaved families regarded the timing of referrals to home hospices as late, and the perceived timing was associated with the family-perceived quality of care and quality of death and dying. Systematic strategies to overcome the barriers related to perceived late referrals are necessary.

Similar content being viewed by others
References
Finlay IG, Higginson IJ, Goodwin DM et al (2002) Palliative care in hospital, hospice, at home: results from a systematic review. Ann Oncol 4:257–264
Brumley R, Enguidanos S, Jamison P et al (2007) Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc 55:993–1000
Drieskens K, Bilsen J, Van Den Block L et al (2008) Characteristics of referral to a multidisciplinary palliative home care team. J Palliat Care 24:162–166
Poulose JV, Do YK, Neo PS et al (2013) Association between referral-to-death interval and location of death of patients referred to a hospital-based specialist palliative care service. J Pain Symptom Manag 46(2):173–181
Morita T, Akechi T, Ikenaga M et al (2005) Late referrals to specialized palliative care service in Japan. J Clin Oncol 23(12):2637–2644
Teno JM, Shu JE, Casarett D et al (2007) Timing of referral to hospice and quality of care: length of stay and bereaved family members' perceptions of the timing of hospice referral. J Pain Symptom Manag 34(2):120–125
Schockett ER, Teno JM, Miller SC et al (2005) Late referral to hospice and bereaved family member perception of quality of end-of-life care. J Pain Symptom Manag 30(5):400–407
Morita T, Miyashita M, Tsuneto S et al (2009) Late referrals to palliative care units in Japan: nationwide follow-up survey and effects of palliative care team involvement after the Cancer Control Act. J Pain Symptom Manag 38(2):191–196
Stillman MJ, Syrjala KL (1999) Differences in physician access patterns to hospice care. J Pain Symptom Manag 17:157–163
Costantini M, Toscani F, Gallucci M et al (1999) Terminal cancer patients and timing of referral to palliative care: a multicenter prospective cohort study. J Pain Symptom Manag 18:243–252
Morita T, Chihara S, Kashiwagi T (2002) Family satisfaction with inpatient palliative care in Japan. Palliat Med 16:185–193
Kris AE, Cherlin EJ, Prigerson H et al (2006) Length of hospice enrollment and subsequent depression in family caregivers: 13-month follow-up study. Am J Geriatr Psychiatr 14(3):264–269
Bradley EH, Prigerson H, Carlson MD et al (2004) Depression among surviving caregivers: does length of hospice enrollment matter? Am J Psychiatry 161(12):2257–2262
Lamont EB, Christakis NA (2002) Physician factors in the timing of cancer patient referral to hospice palliative care. Cancer 94:2733–2737
Medicare: more beneficiaries use hospice but for fewer days of care. Washington, DC, United States General Accounting Office 2000
Christakis NA, Escarce JJ (1996) Survival of medicare patients after enrollment in hospice programs. N Engl J Med 335:172–178
Wright AA, Zhang B, Ray A et al (2008) Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300(14):1665–1673
Ashbury FD, Findlay H, Reynolds B, McKerracher K (1998) A Canadian survey of cancer patients’ experiences: are their needs being met? J Pain Symptom Manag 16:298–306
Casarett D, Abrahm JL (2001) Patients with cancer referred to hospice versus a bridge program: patient characteristics, needs for care, and survival. J Clin Oncol 19:2057–2063
Dudgeon DJ, Raubertas RF, Doerner K et al (1995) When does palliative care begin? A needs assessment of cancer patients with recurrent disease. J Palliat Care 11:5–9
Emanuel LL, Alpert HR, Emanuel EE (2001) Concise screening questions for clinical assessments of terminal care: the needs near the end-of-life care screening tool. J Palliat Med 4:465–474
Temel JS, Greer JA, Muzikansky A et al (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363(8):733–742
Temel JS, Greer JA, Admane S et al (2011) Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 29(17):2319–2326
Casarett DJ, Marenberg ME, Karlawish JH (2001) Predictors of withdrawal from hospice. J Palliat Med 4:491–497
Friedman BT, Harwood MK, Shields M (2002) Barriers and enablers to hospice referrals: an expert overview. J Palliat Med 5:73–84
Ogle KS, Mavis B, Wyatt GK (2002) Physicians and hospice care: attitudes, knowledge, and referrals. J Palliat Med 5:85–92
Pugh EM (1996) An investigation of general practitioner referrals to palliative care services. Palliat Med 10:251–257
Weggel JM (1999) Barriers to the physician decision to offer hospice as an option for terminal care. WMJ 98:49–53
Teno JM, Casarett D, Spence C et al (2012) It is "too late" or is it? Bereaved family member perceptions of hospice referral when their family member was on hospice for seven days or less. J Pain Symptom Manag 43(4):732–738
Morita T, Kizawa Y (2013) Palliative care in Japan: a review focusing on care delivery system. Curr Opin Support Palliat Care 7(2):207–215
Miyashita M, Morita T, Hirai K et al (2008) Evaluation of end-of-life cancer care from the perspective of bereaved family members: the Japanese experience. J Clin Oncol 26(23):3845–3852
Shinjo T, Morita T, Hirai K et al (2010) Care for imminently dying cancer patients: family members' experiences and recommendations. J Clin Oncol 28(1):142–148
Yamagishi A, Morita T, Miyashita M et al (2010) The care strategy for families of terminally ill cancer patients who become unable to take nourishment orally: recommendations from a nationwide survey of bereaved family members' experiences. J Pain Symptom Manag 40(5):671–683
Morita T, Akechi T, Ikenaga M et al (2004) Communication about the ending of anticancer treatment and transition to palliative care. Ann Oncol 15(10):1551–1557
Yamagishi A, Morita T, Miyashita M et al (2012) Preferred place of care and place of death of the general public and cancer patients in Japan. Support Care Cancer 20(10):2575–2582
Morita T, Hirai K, Sakaguchi Y et al (2004) Measuring the quality of structure and process in end-of-life care from the bereaved family perspective. J Pain Symptom Manag 27:492–501
Miyashita M, Morita T, Sato K et al (2008) Good death inventory: a measure for evaluating good death from the bereaved family member's perspective. J Pain Symptom Manag 35:486–498
Hedges LV, Olkin I (1985) Statistical methods for meta-analysis. Academic Press, Orlando
Cohen J (1992) A power primer. Psychol Bull 112:155–159
Morita T, Miyashita M, Yamagishi A et al (2013) Effects of a programme of interventions on regional comprehensive palliative care for patients with cancer: a mixed-methods study. Lancet Oncol 14(7):638–646
Yamagishi A, Morita T, Kawagoe S et al Communication about home hospice referral for patients and families of terminally ill cancerpatients: recommendations from a nationwide survey of bereaved family members’ experiences. Gan to kagaku ryoho (in press, abstract is available in PUBMED in English)
Wilkinson S (2000) Fulfilling patients’ wishes: palliative care at home. Int J Palliat Nurs 6:212
Bowles KH, McCorkle R, Nuamah IF (2008) Homecare referrals and 12-week outcomes following surgery for cancer. Oncol Nurs Forum 35:377–383
Hirabayashi Y, Miyashita M, Kawa M et al (2007) Factors relating to terminally ill cancer patients’ willingness to continue living at home during the early phase of home care after discharge from clinical cancer centers in Japan. Palliat Support Care 5:19–30
Conflict of interest
This study was funded by the Japan Hospice Palliative Care Foundation in Japan. The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamagishi, A., Morita, T., Kawagoe, S. et al. Length of home hospice care, family-perceived timing of referrals, perceived quality of care, and quality of death and dying in terminally ill cancer patients who died at home. Support Care Cancer 23, 491–499 (2015). https://doi.org/10.1007/s00520-014-2397-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2397-7