Abstract
Background
The incidence of bile duct injuries (BDI) after cholecystectomy, which is a life-threatening condition that has several medical and legal implications, currently stands at about 0.6 %. The aim of this study is to describe our experience as the first center to use a laparoscopic approach for BDI repair.
Methods
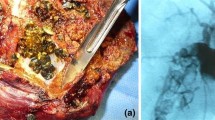
A prospective study between June 2012 and September 2014 was developed. Twenty-nine consecutive patients with BDI secondary to cholecystectomy were included. Demographics, comorbidities, presenting symptoms, details of index surgery, type of lesion, preoperative and postoperative diagnostic work-up, and therapeutic interventions were registered. Videos and details of laparoscopic hepaticojejunostomy (LHJ) were recorded. Injuries were staged using Strasberg classification. A side-to-side anastomosis with Roux-en-Y reconstruction was always used. In patients with E4 and some E3 injuries, a segment 4b or 5 section was done to build a wide anastomosis. In E4 injuries, a neo-confluence was performed. Complications, mortality, and long-term evolution were recorded.
Results
Twenty-nine patients with BDI were operated. Women represented 82.7 % of the cases. The median age was 42 years (range 21–74). Injuries at or above the confluence occurred in 62 %, and primary repair at our institution was performed at 93.1 % of the cases. Eight neo-confluences were performed in all E4 injuries (27.5 %). The median operative time was 240 min (range 120–585) and bleeding 200 mL (range 50–1100). Oral intake was started in the first 48 h. Bile leak occurred in 5 cases (17.2 %). Two patients required re-intervention (6.8 %). No mortality was recorded. The maximum follow-up was 36 months (range 2–36). One patient with E4 injury developed a hepaticojejunostomy (HJ) stenosis after 15 months. This was solved with endoscopic dilatation.
Conclusions
The benefits of minimally invasive approaches in BDI seem to be feasible and safe, even when this is a complex and catastrophic scenario.




Similar content being viewed by others
References
De Santibañes E, Palavecino M, Ardiles V, Pekolj J (2006) Bile duct injuries: management of late complications. Surg Endosc 20:1648–1653
Mercado MA, Franssen B, Domínguez I, Arriola-Cabrera JC, Ramírez-del Val F, Elnecavé-Olaiz A, Arámburo-Garcia R, García A (2011) Transition from a low-to a high-volume centre bile duct repair: changes in technique and improved outcome. HPB 13:767–773
Liu Y, Yao X, Li S, Liu W, Liu L, Liu J (2014) Comparison of therapeutic effects of laparoscopic and open operation for congenital choledochal cysts in adults. Gastroenterol Res Pract. doi:10.1155/2014/670260
Ng JL, Salim MT, Low Y (2014) Mid-term outcomes of laparoscopic versus open choledochal cyst excision in a tertiary paediatric hospital. Ann Acad Med Singapore 43:220–224
Aguirre-Olmedo I, Cuendis-Velázquez A, Morales-Chávez CE, Torres-Ruiz MF, Rojano-Rodríguez ME, Cárdenas-Lailson LE (2013) Laparoscopic choledochoduodenostomy as an optional treatment choledocholithiasis. Cir Cir 81:118–124
Chander J, Mangla V, Vindal A, Lal P, Ramteke VK (2012) Laparoscopic choledochoduodenostomy for biliary stone disease: a single-center 10-year experience. J Laparoendosc Adv Surg Tech A. doi:10.1089/lap.2011.0366
Kondratiuk OP, Khil’ko IuO, Kondratiuk VA, Kravchenko DA (2014) Laparoscopic hepaticojejunostomy in patients with inoperable tumour of pancreatic head. Klin Khir 4:64–65
Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180:101–125
Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM (2009) “Sideways”: result of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg 249:426–434
Mercado MA, Orozco H, de la Garza L, Lopez-Martinez LM, Contreras A, Guillen-Navarro E (1999) Biliary duct injury: partial segment IV resection for intrahepatic reconstruction of biliary lesions. Arch Surg 134:1008–1010
Strasberg SM, Picus DD, Ja Drebin (2001) Results of a new strategy for reconstruction of biliary injuries having an isolated right-sided component. J Gastrointest Surg 5:266–274
Holte K, Bardram L, Wettergren A, Rasmussen A (2010) Reconstruction of major bile duct injuries after laparoscopic cholecystectomy. Dan Med Bull 57:A4135
Al-Ghnaniem R, Benjamin IS (2002) Long-term outcome of hepaticojejunostomy with routine access loop formation following iatrogenic bile duct injury. Br J Surg 89:1118–1124
Jayasundara JA, de Silva WM, Pathirana AA (2011) Changing clinical profile, management strategies and outcome of patients with biliary tract injuries at a tertiary care center in Sri Lanka. Hepatobiliary Pancreat Dis Int 10:526–532
Strasberg SM, Linehan DC, Hawkins WG (2009) The accordion severity grading system of surgical complications. Ann Surg. doi:10.1097/SLA.0b013e3181afde41
Hepp J, Couinaud C (1956) Approach to and use of the left hepatic duct in reparation of the common bile duct. Presse Med 64:947–948
Mercado MA, Chan C, Orozco H, Tielve M, Hinojosa CA (2003) Acute bile duct injury. The need for a high repair. Surg Endosc 17:1351–1355
Schwenk W, Hasse O, Neudecker J, Müller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev 20:CD003145
Zhang Y, Chen XM, Sun DL (2014) Laparoscopic versus open distal pancreatectomy: a single-institution comparative study. World J Surg Oncol. doi:10.1186/1477-7819-12-327
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA (2014) Meta-analysis of laparoscopic vs open cholecystectomy in elderly patients. W J Gastroenterol 20:17626–17634
Bablekos GD, Michaelides SA, Analitis A, Charalabopoulos KA (2014) Effects of laparoscopic cholecystectomy on lung function: a systematic review. World J Gastroenterol. doi:10.3748/wjg.v20.i46.17603
Mercado MA, Chan C, Orozco H, Cano-Gutiérrez G, Chaparro JM, Galindo E, Vilatobá M, Samaniego-Arvizu G (2002) To stent or not to stent bilioenteric anastomosis after iatrogenic injury: a dilemma not answered? Arch Surg 137:60–63
Tocchi A, Costa G, Lepre L, Liotta G, Mazzoni G, Sita A (1996) The long-term outcome of hepaticojejunostomy in the treatment of benign bile duct strictures. Ann Surg 224:162–167
Stewart L, Way L (1995) Bile duct injuries during laparoscopic cholecystectomy. Arch Surg 130:1123–1129
Palermo M, Trelles N, Gagner M (2011) Laparoscopic revisional hepaticojejunostomy for biliary stricture after open repair following common bile duct injury: a case report. Surg Innov. doi:10.1177/1553350610395033
Prasad A, De S, Mishra P, Tiwari A (2015) Robotic assisted Roux-en-Y hepaticojejunostomy in a post-cholecystectomy type E2 bile duct injury. World J Gastroenterol 21:1703–1706
Toumi Z, Aljarabah M, Ammori BJ (2011) Role of the laparoscopic approach to biliary bypass for benign and malignant biliary diseases: a systematic review. Surg Endosc 25:2105–2116
Liem NT (2013) Laparoscopic surgery for choledochal cysts. J Hepatobiliary Pancreat Sci 20:487–491
Lee JH, Kim SH, Kim HY, Choi YH, Jung SE, Park KW (2013) Early experience of laparoscopic choledochal cyst excision in children. J Korean Surg Soc 85:225–229
Liem NT, Pham HD, le Dung A, Son TN, Vu HM (2012) Early and intermediate outcomes of laparoscopic surgery for choledochal cysts with 400 patients. Laparoendosc Adv Surg Tech A 22:599–603
Duan X, Mao X, Jiang B, Wu J (2014) Totally laparoscopic cyst excision and Roux-en-Y hepaticojejunostomy for choledochal cyst in adults: a single-institute experience of 5 years. Surg Laparosc Endosc Percutan Tech 00:001–004
Acknowledgments
We thank Dr. Florencio de la Concha Bermejillo, who helped in the edition of this paper, as well as all the referring surgeons who trusted our team for the treatment of their patients.
Disclosures
Drs. Adolfo Cuendis-Velázquez, Carlos Morales-Chávez, Itzé Aguirre-Olmedo, Fernanda Torres-Ruiz, Martín Rojano-Rodríguez, Luis Fernández-Álvarez, Eduardo Cárdenas-Lailson, and Mucio Moreno-Portillo have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuendis-Velázquez, A., Morales-Chávez, C., Aguirre-Olmedo, I. et al. Laparoscopic hepaticojejunostomy after bile duct injury. Surg Endosc 30, 876–882 (2016). https://doi.org/10.1007/s00464-015-4282-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4282-y