Abstract
Objectives
Surgeon case volume has been utilized in the credentialing process as a surrogate for surgeon skill. The purpose of this study was to compare objective outcome measures of laparoscopic partial colectomies performed by laparoscopically skilled surgeons with varying annual case census.
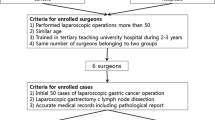
Methods
We performed a retrospective cohort review of all patients (n = 255) undergoing elective laparoscopic partial colectomy. Patients were grouped according to surgeon’s annual case volume as low annual case volume (LV; n = 48) and high annual case volume (HV; n = 207). HV is defined as performing >20 total cases and >25 cases per year. All demographic and clinical variables were evaluated with univariate logistic regression followed by a multivariate logistic regression model for variables approaching significance.
Results
Demographic variables were found to be similar between groups. Only median estimated blood loss (100 vs. 150 mL for HV; p = 0.040) was found to be significantly different between groups. However, this was clinically insignificant, as it did not lead to an increased rate of blood transfusions (0.0 vs. 3.9 % for HV surgeons; p = 0.184). All other variables were similar in both univariate and multivariate logistic regression models.
Conclusions
Among surgeons with advanced laparoscopic training, the data suggest that LV surgeons are able to achieve similar outcomes as those who perform the operation routinely. Annual case volume should not be given undue emphasis when deciding whether to award privileges for laparoscopic partial colectomy.
Similar content being viewed by others
References
Bouchard A, Martel G, Sabri E, Schlachta CM, Poulin EC, Mamazza J, Boushey RP (2009) Does experience with laparoscopic colorectal surgery influence intraoperative outcomes? Surg Endosc 23:862–868
Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW Jr (1997) The learning curve for laparoscopic colorectal surgery. Preliminary results from a prospective analysis of 1194 laparoscopic-assisted colectomies. Arch Surg 132:41–45 Erratum in: Arch Surg 1997 Jul;132(7):781
Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC (2001) Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum 44:217–222
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, Choi HS, Nam BH, Chang HJ, Jeong SY (2009) Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc 23:622–628
Park IJ, Choi GS, Lim KH, Kang BM, Jun SH (2009) Multidimensional analysis of the learning curve for laparoscopic colorectal surgery: lessons from 1,000 cases of laparoscopic colorectal surgery. Surg Endosc 23:839–846
Pendlimari R, Holubar SD, Dozois EJ, Larson DW, Pemberton JH, Cima RR (2012) Technical proficiency in hand-assisted laparoscopic colon and rectal surgery: determining how many cases are required to achieve mastery. Arch Surg 147:317–322
Reichenbach DJ, Tackett AD, Harris J, Camacho D, Graviss EA, Dewan B, Vavra A, Stiles A, Fisher WE, Brunicardi FC, Sweeney JF (2006) Laparoscopic colon resection early in the learning curve: what is the appropriate setting? Ann Surg 243:730–737
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
American Society of Colon and Rectal Surgeons. ASCRS position statement on Laparoscopic Colectomy for Curable Cancer. http://www.fascrs.org/physicians/position_statements/laparoscopic_colectomy/. Accessed 1 July 2013
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL (2003) Surgeon volume and operative mortality in the United States. N Engl J Med 349:2117–2127
Rogers SO Jr, Wolf RE, Zaslavsky AM, Wright WE, Ayanian JZ (2006) Relation of surgeon and hospital volume to processes and outcomes of colorectal cancer surgery. Ann Surg 244:1003–1011
Billingsley KG, Morris AM, Dominitz JA, Matthews B, Dobie S, Barlow W, Wright GE, Baldwin LM (2007) Surgeon and hospital characteristics as predictors of major adverse outcomes following colon cancer surgery: understanding the volume-outcome relationship. Arch Surg 142:23–32
Karanicolas PJ, Dubois L, Colquhoun PH, Swallow CJ, Walter SD, Guyatt GH (2009) The more the better? The impact of surgeon and hospital volume on in-hospital mortality following colorectal resection. Ann Surg 249:954–959
Archampong D, Borowski D, Wille-Jørgensen P, Iversen LH (2012) Workload and surgeon’s specialty for outcome after colorectal cancer surgery. Cochrane Database Syst Rev 3:CD005391
Society of American Gastrointestinal and Endoscopic Surgeons. SAGES guidelines for institutions granting privileges utilizing laparoscopic and/or thoracoscopic techniques. http://www.sages.org/publication/id/14/ Accessed 1 July 2013
Hyman N, Borrazzo E, Trevisani G, Osler T, Shackford S (2007) Credentialing for laparoscopic bowel operation: there is no substitute for knowing the outcomes. J Am Coll Surg 205:576–580
Larson DW, Marcello PW, Larach SW, Wexner SD, Park A, Marks J, Senagore AJ, Thorson AG, Young-Fadok TM, Green E, Sargent DJ, Nelson H (2008) Surgeon volume does not predict outcomes in the setting of technical credentialing: results from a randomized trial in colon cancer. Ann Surg 248:746–750
Singh R, Omiccioli A, Hegge SG, McKinley CA (2009) Can community surgeons perform laparoscopic colorectal surgery with outcomes equivalent to tertiary care centers? Surg Endosc 23:283–288
Kuhry E, Bonjer HJ, Haglind E, Hop WC, Veldkamp R, Cuesta MA, Jeekel J, Påhlman L, Morino M, Lacy A, Delgado S (2005) COLOR Study Group. Impact of hospital case volume on short-term outcome after laparoscopic operation for colonic cancer. Surg Endosc 19:687–692
Disclosure
Shaun C. Daly, Mathew Klairmont, Amanda Francescatti, Jonathan A, Myers, Daniel J. Deziel, and Minh B. Luu have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Daly, S.C., Klairmont, M.M., Francescatti, A.B. et al. Annual case volume has no impact on patient outcomes in laparoscopic partial colectomy. Surg Endosc 28, 1648–1652 (2014). https://doi.org/10.1007/s00464-013-3365-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3365-x