Abstract
Renal transplant recipients (RTR) are considered at high risk for influenza-associated complications due to immunosuppression. The efficacy of standard influenza vaccination in RTRs is unclear. Hence, we evaluated activation of the adaptive immunity by the pandemic influenza A(H1N1) 2009 (A(H1N1)pdm09) vaccine in RTRs as compared to healthy controls. To determine cross-reactivity and/or bystander activation, seasonal trivalent influenza vaccine and tetanus/diphteria toxoid (TT/DT) vaccine-specific T cells along with allospecific T cells were quantified before and after A(H1N1)pdm09 vaccination. Vaccination-induced alloimmunity was additionally determined by quantifying serum creatinine and proinflammatory protein IP-10. Contrary to healthy controls, RTRs required a booster vaccination to achieve seroconversion (13.3 % day 21; 90 % day 90). In contrast to humoral immunity, sufficient A(H1N1)pdm09-specific T-cell responses were mounted in RTRs already after the first immunization with a magnitude comparable with healthy controls. Interestingly, vaccination simultaneously boosted T cells reacting to seasonal flu but not to TT/DT, suggesting cross-activation. No alloimmune effects were recorded. In conclusion, protective antibody responses required booster vaccination. However, sufficient cellular immunity is established already after the first vaccination, demonstrating differential kinetics of humoral and cellular immunity.
Similar content being viewed by others
Introduction
Solid-organ transplant recipients (SOTs) have been considered at high risk for influenza infection-associated complications owing to immunosuppressive regimens [1, 2]; virus encounter can lead to substantial morbidity in those patients [2, 3]. Therefore, prevention of infection in recipients of SOTs is a crucial issue. In line with this, administration of the vaccine against the novel influenza A(H1N1) has been recommended for individuals that are at a high risk of infection [4].
Vaccination efficacy of immunosuppressed individuals is controversial as antibody responses to influenza vaccines were found to be diminished in kidney transplant patients compared to healthy donors in most published data [5–8]. However, a comparable efficacy was also described [9, 10]. A recent report suggests that rates of both positive postvaccination humoral and cellular responses to A(H1N1) are significantly lower in immunosuppressed kidney transplant recipients than those in healthy controls [11].
Accordingly, the frequency of hospitalizations due to pandemic influenza A(H1N1) 2009 virus (A(H1N1)pdm09) infection was found to be substantially higher in kidney transplant patients (53.8 %) as compared to the general population (1–5 %) [12] with most severe complications including acute kidney allograft rejection [13–15]. Despite these dramatic consequences of infection, vaccination against influenza in SOT recipients is a two-edged sword due to the potential promotion of alloreactive T-cell responses [16], also leading to transplant injury or allograft rejection [17, 18]. Thus, there is an urgent need for vaccination recommendations on the basis of efficacy and safety in these at-risk populations.
In the present study, we evaluated kinetics of humoral and cellular responses to the A/California/7/2009 (A(H1N1)pdm09) v-like strain vaccine in renal transplant patients compared to healthy individuals and addressed the issue of cross-reactivity with the seasonal flu vaccine. Considering the concerns of adverse effects, another main focus of this study was to investigate the safety of the vaccine by examining the concentrations of serum creatinine and inflammation-associated protein IP-10 as surrogate markers for graft function [19, 20] as well as alloreactive T-cell responses pre- and postvaccination [18, 21].
Materials and methods
Study population
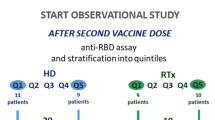
Sixteen renal transplant recipients (RTRs, transplant outpatient units of the University Hospital Charité, Campus Virchow, Berlin) were enrolled in the study. Seventeen healthy volunteers (HV) who were matched for age and gender were included as controls. Patients and controls were excluded for having symptoms of influenza before the vaccination. The immunosuppressive regimens after transplantation are listed in Table 1. Both groups were vaccinated between October and November 2009 (day 0) with single AS03 adjuvant-containing A/California/7/2009 (A(H1N1)pdm09) v-like strain vaccine Pandemrix® (GlaxoSmithKline, Berlin, Germany), for the first time. Additionally, RTRs received a booster vaccination on day 21. None of the participants received a seasonal vaccination by Mutagrip in parallel. Blood samples for FACS analysis were collected at days 0, 21, and 28 for all participants. Vaccine safety was assessed by adverse event report, graft function, and serum creatinine measurements at days 0, 21, and 28 and at a later time points at 2, 3, and 6 months. Antibody responses were determined at days 0 and 21 and additionally at day 90 for RTRs only. Detailed patient control characteristics are shown in Table 1. The study was initiated after obtaining an approval by the local ethics committee, and the study was carried out upon obtaining a signed informed consent from all the participants.
Isolation and in vitro stimulation of peripheral blood mononuclear cells
Peripheral blood mononuclear cells (PBMCs) were isolated from heparinized whole blood by density gradient centrifugation using Ficoll-Paque (Amersham Pharmacia Biotech AB, Sweden) and cultured in RPMI 1640 media containing 0.3 mg/mL glutamine, 100 U/mL penicillin, 0.1 mg/mL streptomycin (Invitrogen), and 10 % human AB serum (PAA Laboratories, Coelbe, Germany). To assess cross-reactivity seasonal flu vaccine (MUTAGRIP®, Sanofi Pasteur MSD, Leimen, Germany) containing antigens of inactivated virus strains, A/Brisbane/59/2007 (H1N1), A/Brisbane/10/2007 (H3N2), and B/Brisbane/60/2008 were applied. Cells were stimulated for 16 h with A/California/7/2009 (A(H1N1)pdm09) v-like strain vaccine (Pandemrix®), seasonal flu vaccine (MUTAGRIP®), combined tetanus/diphteria toxoid vaccine (TT/DT), or staphylococcal enterotoxin B (SEB; Sigma, positive control) at a final concentration of 2 μg/ml, respectively, or left unstimulated (negative control). Secretion inhibitor Brefeldin A (Sigma) was added for the last 14 h of culture.
Phenotyping, intracellular cytokine staining, and FACS data analysis
After antigen stimulation, PBMCs were surface-stained using a panel of fluorochrome-conjugated mAbs including CD3 (BD Biosciences, San Diego, USA), CD4 (BD Biosciences Pharmingen, San Diego, USA), CD69 (BD Biosciences, San Diego, USA), and CD40L (Miltenyi Biotec, Bergisch Gladbach, Germany). Intracellular cytokine staining for IFN-γ (eBiosciences, Frankfurt, Germany) and IL-2 (BD Biosciences, San Diego, USA) was performed using the BD Cytofix/Cytoperm Fixation/Permeabilization Kit according to manufacturer’s instructions (BD Biosciences, San Diego, USA). Approximately 2 × 105 CD3 + T cells per sample were acquired using a LSRII flow cytometer (BD); analysis was performed with FlowJo software (Treestar, Ashland, USA).
Antibody titers
Influenza-specific serum antibody titers were measured by a standard hemagglutination inhibition (HI) assay, using the 2009 H1N1 reference strain A/California/07/2009 and erythrocytes from turkey hens as previously described [22]. Pre- (day 0) and postvaccination (at days 21 and 90) sera were tested simultaneously. An international A(H1N1)pdm09 serum standard (National Institute for Biological Standards and Control, London, UK) served as positive control.
Alloreactive T-cell detection
Alloantigen-specific cellular immune responses were determined by IFN-γ ELISPOT as previously described [23]. Briefly, 96-well multiscreen filter plates (Millipore, MAIPS 4510) were coated with a primary IFN-γ monoclonal antibody (a-human IFN-γ, Endogen M700A) at a concentration of 3 μg/ml. Responder PBMC (3 × 105) were tested in triplicate against a panel of 3 HLA-typed allostimulator B cells at a ratio of 1:1 (3 × 105) or 2.5 μg/ml of Staphylococcus Enterotoxin B (SEB; Sigma, positive control) or medium alone (negative control). After developing and visualizing, the resulting spots were counted using a computer-assisted ELISPOT reader (Immunospot, Cellular Technologies, Ltd., Cleveland, OH, USA). The number of SFU/106 PBMC per well was calculated from triplicates after subtractions of the negative control. Positive ELISPOT signals were predefined as containing at least 10 SFU per well after subtraction of the negative control.
IP-10 ELISA
IP-10 level was measured for assessing the risk of graft rejection as described previously [20]. IP-10 was measured in urine from renal transplant patients and healthy donors at days 0 and 21 by an IP-10 ELISA kit (Hycult Biotech) using the manufacturer’s protocol. The IP-10 cut-off level of 200 pg/ml was determined in our previous study to be predictive for allograft rejection [20].
Statistical analysis
Statistical analysis was conducted using SPSS software version 16 (SPSS Inc., Chicago, IL). Results were presented as median (range). To compare frequencies of cytokine-producing T cells at days 0, 21, and 28, the Mann–Whitney U test and two-sided Wilcoxon signed rank sum test for nonparametric dependent samples were run to determine statistical significance, as appropriate.
Results
Demographic characteristics and safety data of study population
Sixteen renal transplant recipients (median age 47; range 19–65) and 17 healthy controls (median age 42; range 24–59) were enrolled in the study. Detailed characteristics of the patients are shown in Table 1. Two out of 16 patients were excluded during the course of the study due to vaccination-unrelated illness and refusal of further participation, respectively. All RTRs received a second vaccination on day 21. The vaccine was well tolerated by all study participants. No adverse events or influenza infections occurred after vaccination in all patients and controls. No cases of acute rejection occurred during 12 months following vaccination.
Induction of H1N1-specific T cells after primary A(H1N1)pdm09 vaccination
Influenza-specific cellular immunity before and after vaccination was analyzed by flow cytometric enumeration of activated CD154+CD4+ T cells and the respective cytokine expression regarding IFN-γ and IL-2 after in vitro stimulation for 16 h with A(H1N1)pdm09 vaccine (Pandemrix®). The data show that the frequencies of A(H1N1)pdm09-specific CD154+CD4+ T cells in 14 out of 16 RTRs and all healthy controls were increased 3 weeks after the vaccination compared to baseline (baseline: median 0.000 %, range 0.000–0.066 % and day 21: 0.909 %; 0.000–1,870 %, p = 0.0092).
Correspondingly, the percentage of activated CD4+ T cells producing IFN-γ and IL-2 also significantly increased in 14 out of 16 RTRs (baseline: median 0.000 %, range 0.000–0.057 % vs. day 21: median 0.135 %, range 0.015–0.510 %, p = 0.0104 for IFN-γ and baseline: median 0.000 %, range 0.000–0.170 % vs. day 21: median 0.228 %, range 0.013–0.967 %, p = 0.0226 for IL-2), and all controls (baseline: median 0.075 %, range 0.027–0.488 % vs. day 21: median 0.242 %, range 0.016–0.810 %, p = 0.0029 for IFN-γ and baseline: median 0.092 %, range 0.014–0.553 % vs. day 21: median 0.336 %, range 0.020–0.793 %, p = 0.0046 for IL-2), respectively (Fig. 1).
Kinetics of A(H1N1)pdm09 vaccination-induced cellular immunity in renal transplant patients and healthy controls. The figure represents frequencies of H1N1-specific (a, c, d) und seasonal flu-specific (b) T cells following vaccination with A(H1N1)pdm09. Activation marker CD40L+ (a, b) and cytokines IFN-γ (c) and IL-2 (d) were used, respectively, to identify A(H1N1)pdm09-specific (a, c, d) and seasonal flu-specific T cells. *p < 0.05, ** p < 0.01. Renal transplant patients were able to establish vaccination-specific T-cell response already after the first vaccination. The kinetics analysis of T-cell frequencies (days 0, 21, and 28) was performed using two-sided Wilcoxon signed rank sum test for nonparametric dependent samples. To compare the T-cell frequencies between the groups, the Mann–Whitney U test was applied. Data are presented as the median frequencies with interquartile range
With regard to the further kinetics of T-cell response, we observed a peak of the H1N1-specific T-cell response on day 21 in RTRs and controls for CD154+IFN-γ+ populations and IL-2+ population of RTRs. These cells showed a plateau until day 28. In contrast, IL-2+CD4+ T cells in the control group were increasing up to day 28 (day 21: median 0.336 %, range 0.020–0.793 % vs. day 28: median 0.468 %, range 0.017–1.163 %, p = 0.0046; Fig. 1).
Of interest, 33 % RTRs and 100 % controls had detectable H1N1-specific IFN-γ and/or IL-2 CD4 + T cells already before vaccination.
Immunosuppressed patients mount a sufficient cellular immunity already after the first A(H1N1)pdm09 vaccination
In order to assess the impact of immunosuppressive treatment on the vaccine-induced cellular immunity, we compared the magnitude of A(H1N1)pdm09-specific T-cell response between RTRs and healthy controls. Although the frequencies of IFN-γ-producing T cells at day 21 were slightly reduced in RTRs as compared to healthy individuals (0.135 and 0.242 %, p = 0.046), we did not observe differences for IL-2-producing T helper cells (0.228 % in RTRs vs. 0.336 % in HV, p > 0.05) (Fig. 2a). Moreover, analyses of A(H1N1)pdm09-specific T cells simultaneously producing IFN-γ and IL-2 in transplant patients identified the frequencies that were comparable to healthy controls (Fig. 2b).
Distribution of distinct T-cell subsets within vaccination-specific T cells between transplant patients and healthy controls on day 21. a Presented are frequencies of all A(H1N1)pdm09-specific T cell producing IFN-γ or IL-2, respectively, independently from their subset origin (single or double cytokine producers). There were no significant differences in the frequencies of IL-2 or double producers between healthy individuals and transplant patients. Although transplant patients mounted a sufficient number of IFN-γ+ T cells, the magnitude of response for this cell subset was significantly higher in healthy controls. b Presented are A(H1N1)pdm09-specific T-cell frequencies producing single IFN-γ, single IL-2, or simultaneously IFN-γ and IL-2. While no differences were found for single IL-2 producers between healthy population and transplant patients, the magnitude of response for single IFN-γ+ T-cell subset was significantly higher in healthy controls. Statistical comparison of the T-cell frequencies between the groups was performed by the Mann–Whitney U test. Data in the figures are presented as the median frequencies with interquartile range. *p < 0.05
Impact of A(H1N1)pdm09 vaccination on seasonal flu-specific T cells
To examine whether A(H1N1)pdm09 vaccination is also able to concomitantly induce cross-activation of T cells with other influenza specificities, we analyzed T-cell immunity against trivalent seasonal influenza vaccine (MUTAGRIP®) before and after A(H1N1)pdm09 vaccination. In parallel, TT/DT vaccine-specific T-cell responses were analyzed, in order to exclude that the observed seasonal flu-specific response are not due to bystander activation. Interestingly, we detected increase in seasonal flu-specific T cells upon A(H1N1)pdm09 vaccination. Thus, there were significantly higher frequencies of seasonal flu-specific T helper cells on day 21 vs day 0 that produced IL-2 (baseline: median 0.051 %, range 0.000–0.497 % vs. day 21: median 0.258 %, range 0.086–0.686 %, p = 0.033) and IFN-γ (baseline: median 0.038 %, range 0.000–0.430 % vs. day 21: median 0.205 %, range 0.041–1.040 %, p = 0.029) in RTRs. The control group exhibited a similar increase that was also significant regarding both IFN-γ (baseline: median 0.218 %, range 0.032–0.4297 % vs. day 21: median 0.452 %, range 0.110–0.740 %, p = 0.002)- and IL-2 (baseline: median 0.223 %, range 0.023–0.486 % vs. day 21: median 0.372 %, range 0.074–0.996 %, p = 0.023)-producing T cells.
Comparison of seasonal flu-specific T-cell immunity after A(H1N1)pdm09 vaccination between transplant patients and healthy controls identified similar frequency differences obtained for pandemic flu-specific T cells. Thus, on day 21, the seasonal flu-induced IFN-γ-producing CD4+ T cells were detected in lower frequency in RTRs compared to healthy controls (0.205 and 0.452 %, p = 0.046), Fig. 3a. No statistical differences were observed for IL-2-producing seasonal flu-specific T cells between RTRs and controls, Fig. 3b.
A(H1N1)pdm09 vaccination induces cross-reactivity but no bystander activation in renal transplant patients and healthy controls. The figure illustrates the kinetics of seasonal flu-specific (a, b) and TT/DT vaccine (tetanus/diphteria toxoid)-specific (c, d) T cells following vaccination with A(H1N1)pdm09. There were an increase in the frequencies of seasonal flu-specific T cells in follow-up (cross-reactivity), but no significant changes with regard to the frequencies of TT/DT-specific T cells (bystander activation). Two-sided Wilcoxon signed rank sum test for nonparametric dependent samples was performed to evaluate statistical differences of the data measured at different time points (days 0, day 21, and day 28). Comparison of the T-cell frequencies between the groups was performed by the Mann–Whitney U test. Data are presented as the median frequencies with interquartile range. *p < 0.05
Bystander T-cell activation was investigated by comparing the frequencies of TT/DT-specific T cells at day 0 and day 21 after vaccination. Herein, we did not observe any significant increases of TT/DT-specific T cells after A(H1N1)pdm09 vaccination in RTRs and controls, respectively (p > 0.05), Fig. 3c. Together, this suggests that A(H1N1)pdm09 vaccination boosts seasonal flu-specific immunity due to cross-reactivity rather than general bystander activation that would equally have affected the tetanus/diphteria response.
Protective antibody response requires an additional booster dose of A(H1N1)pdm09 vaccine in RTRs
Humoral response to vaccination was measured by assessing seroconversion (antibody titer increase pre/post vaccination ≥ fourfold) and seroprotection (postvaccination HI titer of 1:40 or more) rates. For this purpose, HI titers against A(H1N1)pdm09 were analyzed pre- (day 0) and postvaccination (day 21) in RTR and healthy controls. According to recommendation of the Advisory Committee, all RTRs were boosted with pandemic flu vaccine on day 21 and additionally investigated at day 90.
While preimmunization HI titers, absent in RTRs, 12.5 % healthy individuals exhibited serum titers higher than 1:40, indicating previous immunization or infection (Fig. 4). Postvaccination, seroprotection, and seroconversion rates of 93.33 % were present in healthy individuals until day 21 (1:960 median, range 1:60–1280; Fig. 4). In contrast, only 13.3 % of RTRs developed protective HI antibody titers until day 21 (1:40 median, range 1:40–160). Interestingly, 90 % of the patients developed seroconversion/seroprotection on day 90 with rates comparable with the percentage rate of the control group on day 21 (93.33 %). Interestingly, the median HI titers were significantly higher in the control group compared to RTRs postvaccination (1:160, range 1:10–1:1280 for RTRs and 1:960, range 1:30–1:1280 for controls; p < 0.05). These data suggest that immunosuppressive therapy reduces the vaccine-specific serum Ig induction and indicate that an additional booster vaccination is required in immunocompromised patients to achieve protective humoral immunity.
Efficient protective antibody induction after A(H1N1)pdm09 booster vaccination. All individuals were pandemic flu vaccinated (day 0), and the renal transplant recipients (RTRs) received a booster vaccination (day 21). Pandemic flu-specific antibody serum concentrations were determined. Data show the rate of seroprotected individuals (transplant n = 14, healthy n = 17). No seroprotection was found in RTRs prior vaccination. In contrast, 12.5 % of controls showed titers of 1:40 or more at day 0. Arrow illustrates the low rate of seroprotection in RTRs at day 21
Safety of A(H1N1)pdm09 vaccination in renal transplant patients
For assessing the safety of A(H1N1)pdm09 vaccination with regard to an induction of allospecific immunity as a vaccination side effect, we analyzed urine IP-10 concentrations (days 0 and 21) that were previously identified as a predictive marker of graft rejection [20]. Postvaccination IP-10 concentrations were below the cut-off level of 200 pg/ml in both groups, except for one patient (Table 1). This patient showed an increased IP-10 level of 1073.9 pg/ml on day 21. Analysis of serum creatinine at days 0, 21, and 28 and the follow-up at months 2, 3, and 6 showed, however, no graft function deterioration. There were also no significant changes in creatinine concentration in other RTRs at all time points, indicating unaltered graft function (Table 1). In addition, we assessed frequencies of alloreactive T cells before (day 0) and after (day 21) vaccination in four patients by IFN-γ ELISPOT, respectively.
Allospecific immunity was analyzed by stimulating patient PBMCs with B cells HLA matched to the transplant donor as previously published by us [23]. No alloantigen-specific IFN-γ-producing T cells were detectable pre- and postvaccination in all investigated RTRs including the patient with the highly elevated IP-10 level presented above. These data imply stable graft function upon A(H1N1)pdm09 vaccination.
Discussion
Influenza is the seventh leading cause of death in the USA, with immune-compromised populations accounting for >90 % of influenza-related deaths [24]. Being immunologically different from other influenza strains, the A(H1N1)pdm09 virus infection caused about 256000 hospitalization cases with unusual high frequency of severe diseases in younger and otherwise healthy patients [24]. While data on humoral response in immune-compromised patients such as transplant populations have been published in some previous studies [8–10, 25], no comprehensive data on induction of both humoral and cellular immunity after vaccination with A(H1N1)pdm09 in transplant patients are available. In this study, we demonstrate that despite immunosuppression, protective antibody titers can be induced in the majority of kidney transplant patients. In contrast to healthy individuals, however, an additional booster vaccination is required to establish seroprotection/seroconversion. In contrast to humoral response, sufficient cellular immunity was evident already after the first/single vaccination in renal transplant patients with, frequencies and quality of A(H1N1)pdm09-specific T cells mostly comparable to that of healthy individuals. To our knowledge, this is the first study demonstrating the kinetics of cellular immunity preceding the humoral response and establishes already after the first vaccination shot. Most importantly, our results indicate that A(H1N1)pdm09 vaccination was safe and well tolerated by all patients.
Overall, studies are available regarding the immunogenicity and safety of the pandemic influenza vaccine in immunosuppressed hosts with most authors focusing on humoral immunity [25–30]. De Lavallade also addressed cellular immune responses by detecting A(H1N1)pdm09-specific T cells in a cohort of stem cell transplant patients [31]; however, no data on cellular immunity kinetics in particular with regard to the first/booster vaccination have been obtained. Here, we provide evidence that despite the absence of protective antibody titers at day 21 after a single vaccination, a robust T-cell response could be mounted in all kidney transplant patients. The percentage of activated CD4 + T cells producing IL-2 and/or IFN-γ was significantly increased compared to baseline with the frequencies exceeding previously published data on CMV-, and BKV-specific T-cell immunity in transplant patients of our center [32, 33].
Of special interest are the data on cytokine-producing cells. Previous studies by some groups including our own demonstrated an important role of so-called multifunctional CD4 + T cells simultaneously producing different cytokines for the clearance of viral infections [32, 34]. Using the advantages of multicolor flow cytometry, we analyzed the frequencies of IL-2/IFN-γ double CD4 + T cells producers. Surprisingly, the frequencies were at comparable levels in patients and healthy controls, demonstrating neglectable effect of immunosuppression on the quality of cellular immunity in studied renal transplant patients.
Although vaccinations are generally safe and well tolerated in transplant populations, there were some concerns about allosensitization that might be provoked by influenza immunization [35]. Therefore, we were wondering whether A(H1N1)pdm09 vaccination can trigger immune response against antigenic specificities other than A(H1N1)pdm09. For this purpose, we analyzed T cells specific for TT/DT toxoid vaccine and allospecific B cell bank—which reflect the level of unspecific/bystander activation. We did not observe increase in TT/DT-specific or allospecific T cells following vaccination with A(H1N1)pdm09 vaccine, suggesting lack of unspecific/bystander activation. On the other hand, we analyzed cross-reactivity of T cells specific for seasonal flu vaccine containing antigens of inactivated influenza A/Brisbane/59/2007 (H1N1) strain with 79 % homology of hemagglutinin and 81 % homology of neuraminidase antigens to the A(H1N1)pdm09 strain. We found a clear frequency rise in seasonal flu-specific CD4 + T cells after vaccination with A(H1N1)pdm09 vaccine. This finding suggests that preexisting memory T cells against seasonal flu have been cross-activated by A(H1N1)pdm09 vaccination due to the close relation or more specifically shared epitopes between circulating seasonal influenza viruses and the A(H1N1)pdm09 virus [36–39]. In fact, a bioinformatic study on influenza epitope prediction revealed highly conserved cross-reactive CD4 + T-cell epitopes in the hemagglutinin antigen (95–100 %) for seasonal H1N1 and A(H1N1)pdm09 strains [38].
Of interest, previous data on A(H1N1)pdm09 humoral immunity published by Allwinn et al. demonstrated preexisting neutralizing antibodies in 19 out of 145 tested individuals [40, 41]. In line with these data, we also showed preexisting seasonal influenza-specific T cells and A(H1N1)pdm09-specific T cells in control group already before vaccination. Therefore, we wondered whether the previous vaccinations might be responsible for the maintained cellular immunity. The detailed evaluation of vaccination history revealed a low incidence with annual flu vaccination in 8 %, once in 5 years in 16 %, a single vaccination 10 years ago in 33 %, and no flu vaccination in 50 %, suggesting that the preexisting cellular immunity can be rather explained by the history of clinically unapparent influenza infections. Similarly, on the other hand, despite the low vaccination history, no previous cases of clinically apparent influenza infections were reported by study participants. It is well known that CD4 + T cells provide indirect help in viral clearance by secreting cytokines to activated CD8 + T cells and inducing antibodies that neutralize the virus [42, 43]. More recently, a direct role for CD4 T cells has been suggested in chronic virus infection [44] to induce differentiated cytotoxic CD4 + T cells [45]. Interestingly, multifunctional CD4 + T cells expressing IFN-γ and perforin directly promoted protection against lethal influenza virus infection in mice [46]. A recent human experimental study on influenza-infected healthy controls demonstrated that preexisting CD4 + T cells respond to influenza-conserved epitopes, limiting viral shedding and severity of infection independent of the antibody titers [47]. Taken together, these data might indicate the protective role of IL-2/IFN-γ-producing memory T cells detected in our study and explain the lack of clinically apparent influenza infection reported in the study population.
In line with our finding regarding the dichotomy of cellular and humoral responses, Ballet et al. [48] showed that cellular responses against seasonal influenza vaccine did not differ between healthy volunteers and immunosuppressed kidney-transplanted patients, despite reduced humoral responses in the latter group. Interestingly, in contrast to RTRs under immunosupression, operationally tolerant patients showed similar titers as control individuals, thereby directly demonstrating the effect of medication on vaccination-induced humoral immunity.
The quality of anti-infectious defense is dependent on the interplay of cellular and humoral immunity [49]. While T-cell responses are essential for viral clearance, protective antibodies are important for host defense of an acquired influenza infection [50–52]. In our study, RTRs were assessed for the presence of protective antibody titers against A(H1N1)pdm09 on days 0, 21, and 90. Only 13.33 % of the renal transplant recipients developed humoral protection until day 21 after the first A(H1N1)pdm09 vaccination. Nevertheless, after application of an additional booster dose of A(H1N1)pdm09 vaccine on day 21, 90 % of RTRs developed seroprotective antibody titers of 1:40 or more. A beneficial effect with a higher antibody response after a booster dose was also observed in studies with children [53, 54]. In line with that, an enhanced immune response with seroconversion rate increase from 41.2 % after the first vaccination to 81.8 % after the second vaccination was observed in patients with hematopoietic stem cell transplantation [41]. In addition, influenza A(H1N1)pdm09 vaccination elicited weaker antibody responses in solid-organ transplant patients compared to healthy controls or HIV patients in a recent publication [28]. However, in the same study, several healthy individuals who were seronegative at day 21 still seroconverted until day 49, suggesting slower kinetics in this subgroup. On this background, one could speculate that some of our patients might have reached sufficient antibody titers at later time points even without revaccination. Otherwise, the data by Bickel et al. [55] showed a significantly higher seroconversion rate in HIV patients repeatedly vaccinated by adjuvanted H1N1 vaccine during two seasons as compared to one-dose vaccination schedule, indicating the importance of a booster vaccination in immunocompromised patients.
The use of adjuvant-containing vaccines in immunosuppressed hosts is controversially discussed [56, 57]. As a consequence, most of the past large studies applied influenza vaccines without adjuvants for immunization of SOTs in which no increase in rejection rates or adverse effects after vaccination were shown [10, 11, 26]. In contrast, one study indicated that alloresponses in SOT recipients could be potentially triggered by influenza vaccination [16]. In our study, adverse events of AS03-adjuvanted influenza A(H1N1)pdm09 vaccination were determined by quantifying urine concentrations of the proinflammatory cytokine IP-10 along with serum creatinine levels and alloantigen-specific IFN-γ T cells. Most importantly, we did not observe rejection episodes; in addition, all vaccinated patients exhibited stable serum creatinine concentrations. Furthermore, IP-10-levels were elevated in only one patient, in whom no organ dysfunction/rejection episode and no increase in alloantigen-specific IFN-γ T cells after A(H1N1)pdm09 vaccination were observed, indicating independent reasons for IP-10 upregulation.
Our study has also some limitations. They include the single-center nature of the study as well as relatively small number of patients and healthy volunteers. Due to logistic reasons (high work load associated with cell stimulations and measurements and vaccination-determined limited patient recruitment time), we were able to analyze only a limited number of patients. Nevertheless, our study has a pilot character with robust statistical results. Although our results convincingly indicate that A(H1N1)pdm09 vaccination was effective, safe, and well tolerated by all patients, a large-scale multicenter trial is required to validate these findings.
In conclusion, we demonstrate that in immunosuppressed patients, a prime-boost regimen is required for the induction of humoral immunity against A(H1N1)pdm09. In contrast, cellular immunity appears to be not altered under immunosuppressive therapy and is established already after the first vaccination. These data suggest that sufficient cellular immune response might enable viral clearance and resolution of H1N1 infection transplant patients already after the first immunization. However, to establish seroprotection preventing infection with influenza virus, second vaccination is required. In addition, due to the lack of adverse events including alloimmunity, adjuvant-containing boost vaccination appears to be an appropriate regimen for immunosuppressed patients.
References
Ljungman P, Andersson J, Aschan J, Barkholt L, Ehrnst A, Johansson M, Weiland O (1993) Influenza A in immunocompromised patients. Clin Infect Dis 17(2):244–247
Vilchez RA, McCurry K, Dauber J, Lacono A, Griffith B, Fung J, Kusne S (2002) Influenza virus infection in adult solid organ transplant recipients. Am J Transplant 2(3):287–291
Kumar D, Michaels MG, Morris MI, Green M, Avery RK, Liu C, Danziger-Isakov L, Stosor V, Estabrook M, Gantt S, Marr KA, Martin S, Silveira FP, Razonable RR, Allen UD, Levi ME, Lyon GM, Bell LE, Huprikar S, Patel G, Gregg KS, Pursell K, Helmersen D, Julian KG, Shiley K, Bono B, Dharnidharka VR, Alavi G, Kalpoe JS, Shoham S, Reid GE, Humar A (2010) Outcomes from pandemic influenza A H1N1 infection in recipients of solid-organ transplants: a multicentre cohort study. Lancet Infect Dis 10(8):521–526
Fiore AE, Shay DK, Broder K, Iskander JK, Uyeki TM, Mootrey G, Bresee JS, Cox NJ (2009) Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep 58(RR-8):1–52
Smith KG, Isbel NM, Catton MG, Leydon JA, Becker GJ, Walker RG (1998) Suppression of the humoral immune response by mycophenolate mofetil. Nephrol Dial Transplant 13(1):160–164
Sanchez-Fructuoso AI, Prats D, Naranjo P, Fernandez-Perez C, Gonzalez MJ, Mariano A, Gonzalez J, Figueredo MA, Martin JM, Paniagua V, Fereres J, Gomez de la Concha E, Barrientos A (2000) Influenza virus immunization effectivity in kidney transplant patients subjected to two different triple-drug therapy immunosuppression protocols: mycophenolate versus azathioprine. Transplantation 69(3):436–439
Wyzgal J, Brydak LB, Zygier D, Paczek L, Rowinski W, Grochowiecki T (2002) Study on efficacy of influenza vaccination in renal allograft recipients. Transplant Proc 34(2):572–575
Birdwell KA, Ikizler MR, Sannella EC, Wang L, Byrne DW, Ikizler TA, Wright PF (2009) Decreased antibody response to influenza vaccination in kidney transplant recipients: a prospective cohort study. Am J Kidney Dis 54(1):112–121
Carroll RN, Marsh SD, O’Donoghue EP, Breeze DC, Shackman R (1974) Response to influenza vaccine by renal transplant patients. Br Med J 2(5921):701–703
Scharpe J, Evenepoel P, Maes B, Bammens B, Claes K, Osterhaus AD, Vanrenterghem Y, Peetermans WE (2008) Influenza vaccination is efficacious and safe in renal transplant recipients. Am J Transplant 8(2):332–337
Candon S, Thervet E, Lebon P, Suberbielle C, Zuber J, Lima C, Charron D, Legendre C, Chatenoud L (2009) Humoral and cellular immune responses after influenza vaccination in kidney transplant recipients. Am J Transplant 9(10):2346–2354
Ridao-Cano N, Sanchez-Fructuoso AI, Rodriguez-Moreno A, Barrientos A (2009) H1N1 2009 influenza in kidney transplant patients. Transplantation 90(2):224–225
Camargo LF, de Sandes-Freitas TV, Silva CD, Bittante CD, Ono G, Correa L, Silva M Jr, Bellei NC, Goto JM, Medeiros EA, Gomes PS, Medina-Pestana JO (2012) Morbimortality of pandemic influenza A H1N1 infection in kidney transplant recipients requiring hospitalization: a comparative analysis with nonimmunocompromised patients. Transplantation 93(1):69–72
Keane WR, Helderman JH, Luby J, Gailiunas P, Hull AR, Kokko JP (1978) Epidemic renal transplant rejection associated with influenza A Victoria. Proc Clin Dial Transplant Forum 8:232–236
Kunisaki KM, Janoff EN (2009) Influenza in immunosuppressed populations: a review of infection frequency, morbidity, mortality, and vaccine responses. Lancet Infect Dis 9(8):493–504
Danziger-Isakov L, Cherkassky L, Siegel H, McManamon M, Kramer K, Budev M, Sawinski D, Augustine JJ, Hricik DE, Fairchild R, Heeger PS, Poggio ED (2010) Effects of influenza immunization on humoral and cellular alloreactivity in humans. Transplantation 89(7):838–844
Poggio ED, Clemente M, Riley J, Roddy M, Greenspan NS, Dejelo C, Najafian N, Sayegh MH, Hricik DE, Heeger PS (2004) Alloreactivity in renal transplant recipients with and without chronic allograft nephropathy. J Am Soc Nephrol 15(7):1952–1960
Heeger PS (2003) T-cell allorecognition and transplant rejection: a summary and update. Am J Transplant 3(5):525–533
Matl I, Hribova P, Honsova E, Brabcova I, Viklicky O (2010) Potential predictive markers in protocol biopsies for premature renal graft loss. Kidney Blood Press Res 33(1):7–14
Matz M, Beyer J, Wunsch D, Mashreghi MF, Seiler M, Pratschke J, Babel N, Volk HD, Reinke P, Kotsch K (2006) Early post-transplant urinary IP-10 expression after kidney transplantation is predictive of short- and long-term graft function. Kidney Int 69(9):1683–1690
Hricik DE, Rodriguez V, Riley J, Bryan K, Tary-Lehmann M, Greenspan N, Dejelo C, Schulak JA, Heeger PS (2003) Enzyme linked immunosorbent spot (ELISPOT) assay for interferon-gamma independently predicts renal function in kidney transplant recipients. Am J Transplant 3(7):878–884
Meyer S, Adam M, Schweiger B, Ilchmann C, Eulenburg C, Sattinger E, Runte H, Schluter M, Deuse T, Reichenspurner H, Costard-Jackle A (2011) Antibody response after a single dose of an AS03-adjuvanted split-virion Influenza A(H1N1) vaccine in heart transplant recipients. Transplantation 91(9):1031–1035
Andree H, Nickel P, Nasiadko C, Hammer MH, Schonemann C, Pruss A, Volk HD, Reinke P (2006) Identification of dialysis patients with panel-reactive memory T cells before kidney transplantation using an allogeneic cell bank. J Am Soc Nephrol 17(2):573–580
Wrammert J, Koutsonanos D, Li GM, Edupuganti S, Sui J, Morrissey M, McCausland M, Skountzou I, Hornig M, Lipkin WI, Mehta A, Razavi B, Del Rio C, Zheng NY, Lee JH, Huang M, Ali Z, Kaur K, Andrews S, Amara RR, Wang Y, Das SR, O’Donnell CD, Yewdell JW, Subbarao K, Marasco WA, Mulligan MJ, Compans R, Ahmed R, Wilson PC (2011) Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J Exp Med 208(1):181–193
Fairhead T, Hendren E, Tinckam K, Rose C, Sherlock CH, Shi L, Crowcroft NS, Gubbay JB, Landsberg D, Knoll G, Gill J, Kumar D (2012) Poor seroprotection but allosensitization after adjuvanted pandemic influenza H1N1 vaccine in kidney transplant recipients. Transpl Infect Dis 14(6):575–583
Ott U, Sauerbrei A, Lange J, Schafler A, Walther M, Wolf G, Wutzler P, Zell R, Krumbholz A (2012) Serological response to influenza A H1N1 vaccine (Pandemrix®) and seasonal influenza vaccine 2009/2010 in renal transplant recipients and in hemodialysis patients. Med Microbiol Immunol 201(3):297–302
Quintana LF, Serra N, De Molina-Llaurado P, Blasco M, Martinez M, Campos B, Bayas JM, Pumarola T, Campistol JM (2012) Influence of renal replacement therapy on immune response after one and two doses of the A(H1N1) pdm09 vaccine. Influenza Other Respi Viruses
Manuel O, Pascual M, Hoschler K, Giulieri S, Alves D, Ellefsen K, Bart PA, Venetz JP, Calandra T, Cavassini M (2011) Humoral response to the influenza A H1N1/09 monovalent AS03-adjuvanted vaccine in immunocompromised patients. Clin Infect Dis 52(2):248–256
Brakemeier S, Schweiger B, Lachmann N, Glander P, Schonemann C, Diekmann F, Neumayer HH, Budde K (2011) Immune response to an adjuvanted influenza A H1N1 vaccine (Pandemrix®) in renal transplant recipients. Nephrol Dial Transplant 27(1):423–428
Esposito S, Meregalli E, Daleno C, Ghio L, Tagliabue C, Valzano A, Serra D, Galeone C, Edefonti A, Principi N (2011) An open-label, randomized clinical trial assessing immunogenicity, safety and tolerability of pandemic influenza A/H1N1 MF59-adjuvanted vaccine administered sequentially or simultaneously with seasonal virosomal-adjuvanted influenza vaccine to paediatric kidney transplant recipients. Nephrol Dial Transplant 26(6):2018–2024
de Lavallade H, Garland P, Sekine T, Hoschler K, Marin D, Stringaris K, Loucaides E, Howe K, Szydlo R, Kanfer E, Macdonald D, Kelleher P, Cooper N, Khoder A, Gabriel IH, Milojkovic D, Pavlu J, Goldman JM, Apperley JF, Rezvani K (2011) Repeated vaccination is required to optimize seroprotection against H1N1 in the immunocompromised host. Haematologica 96(2):307–314
Muller K, Schachtner T, Sattler A, Meier S, Friedrich P, Trydzenskaya H, Hinrichs C, Trappe R, Thiel A, Reinke P, Babel N (2011) BK-VP3 as a new target of cellular immunity in BK virus infection. Transplantation 91(1):100–107
Bunde T, Kirchner A, Hoffmeister B, Habedank D, Hetzer R, Cherepnev G, Proesch S, Reinke P, Volk HD, Lehmkuhl H, Kern F (2005) Protection from cytomegalovirus after transplantation is correlated with immediate early 1-specific CD8 T cells. J Exp Med 201(7):1031–1036
Harari A, Petitpierre S, Vallelian F, Pantaleo G (2004) Skewed representation of functionally distinct populations of virus-specific CD4 T cells in HIV-1-infected subjects with progressive disease: changes after antiretroviral therapy. Blood 103(3):966–972
Kumar D, Campbell P, Humar A (2011) Donor-specific alloantibody upregulation after influenza vaccination in transplant recipients. Am J Transplant 11(11):2538
Lee VJ, Tay JK, Chen MI, Phoon MC, Xie ML, Wu Y, Lee CX, Yap J, Sakharkar KR, Sakharkar MK, Lin RT, Cui L, Kelly PM, Leo YS, Tan YJ, Chow VT (2010) Inactivated trivalent seasonal influenza vaccine induces limited cross-reactive neutralizing antibody responses against 2009 pandemic and 1934 PR8 H1N1 strains. Vaccine 28(42):6852–6857
Xing Z, Cardona CJ (2009) Preexisting immunity to pandemic (H1N1). Emerg Infect Dis 15(11):1847–1849
Duvvuri VR, Moghadas SM, Guo H, Duvvuri B, Heffernan JM, Fisman DN, Wu GE, Wu J (2010) Highly conserved cross-reactive CD4 + T-cell HA-epitopes of seasonal and the 2009 pandemic influenza viruses. Influenza Other Respi Viruses 4(5):249–258
Greenbaum JA, Kotturi MF, Kim Y, Oseroff C, Vaughan K, Salimi N, Vita R, Ponomarenko J, Scheuermann RH, Sette A, Peters B (2009) Pre-existing immunity against swine-origin H1N1 influenza viruses in the general human population. Proc Natl Acad Sci USA 106(48):20365–20370
Allwinn R, Geiler J, Berger A, Cinatl J, Doerr HW (2010) Determination of serum antibodies against swine-origin influenza A virus H1N1/09 by immunofluorescence, haemagglutination inhibition, and by neutralization tests: how is the prevalence rate of protecting antibodies in humans? Med Microbiol Immunol 199(2):117–121
Gueller S, Allwinn R, Mousset S, Martin H, Wieters I, Herrmann E, Serve H, Bickel M, Bug G (2011) Enhanced immune response after a second dose of an AS03-adjuvanted H1N1 influenza A vaccine in patients after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 17(10):1546–1550
Kamperschroer C, Dibble JP, Meents DL, Schwartzberg PL, Swain SL (2006) SAP is required for Th cell function and for immunity to influenza. J Immunol 177(8):5317–5327
Mozdzanowska K, Furchner M, Maiese K, Gerhard W (1997) CD4 + T cells are ineffective in clearing a pulmonary infection with influenza type A virus in the absence of B cells. Virology 239(1):217–225
van de Berg PJ, van Leeuwen EM, ten Berge IJ, van Lier R (2008) Cytotoxic human CD4(+) T cells. Curr Opin Immunol 20(3):339–343
Appay V (2004) The physiological role of cytotoxic CD4(+) T-cells: the holy grail? Clin Exp Immunol 138(1):10–13
Brown DM, Lee S, Garcia-Hernandez Mde L, Swain SL (2012) Multifunctional CD4 cells expressing gamma interferon and perforin mediate protection against lethal influenza virus infection. J Virol 86(12):6792–6803
Wilkinson TM, Li CK, Chui CS, Huang AK, Perkins M, Liebner JC, Lambkin-Williams R, Gilbert A, Oxford J, Nicholas B, Staples KJ, Dong T, Douek DC, McMichael AJ, Xu XN (2012) Preexisting influenza-specific CD4 + T cells correlate with disease protection against influenza challenge in humans. Nat Med 18(2):274–280
Ballet C, Roussey-Kesler G, Aubin JT, Brouard S, Giral M, Miqueu P, Louis S, van der Werf S, Soulillou JP (2006) Humoral and cellular responses to influenza vaccination in human recipients naturally tolerant to a kidney allograft. Am J Transplant 6(11):2796–2801
Ghendon Y (1990) The immune response to influenza vaccines. Acta Virol 34(3):295–304
Sant AJ, Chaves FA, Krafcik FR, Lazarski CA, Menges P, Richards K, Weaver JM (2007) Immunodominance in CD4 T-cell responses: implications for immune responses to influenza virus and for vaccine design. Expert Rev Vaccines 6(3):357–368
Teijaro JR, Verhoeven D, Page CA, Turner D, Farber DL (2010) Memory CD4 T cells direct protective responses to influenza virus in the lungs through helper-independent mechanisms. J Virol 84(18):9217–9226
Miesegaes G, Lute S, Brorson K (2010) Analysis of viral clearance unit operations for monoclonal antibodies. Biotechnol Bioeng 106(2):238–246
Neuzil KM, Jackson LA, Nelson J, Klimov A, Cox N, Bridges CB, Dunn J, DeStefano F, Shay D (2006) Immunogenicity and reactogenicity of 1 versus 2 doses of trivalent inactivated influenza vaccine in vaccine-naive 5-8-year-old children. J Infect Dis 194(8):1032–1039
Englund JA, Walter E, Black S, Blatter M, Nyberg J, Ruben FL, Decker MD (2010) Safety and immunogenicity of trivalent inactivated influenza vaccine in infants: a randomized double-blind placebo-controlled study. Pediatr Infect Dis J 29(2):105–110
Bickel M, Lassmann C, Wieters I, Doerr HW, Herrmann E, Wicker S, Brodt HR, Stephan C, Allwinn R, Jung O (2013) Immune response after a single dose of the 2010/11 Trivalent, seasonal influenza vaccine in HIV-1-infected patients and healthy controls. HIV Clin Trials 14(4):175–184
Walker WT, Faust SN (2010) Monovalent inactivated split-virion AS03-adjuvanted pandemic influenza A (H1N1) vaccine. Expert Rev Vaccines 9(12):1385–1398
Skowronski DM, Janjua NZ, De Serres G, Hottes TS, Dickinson JA, Crowcroft N, Kwindt TL, Tang P, Charest H, Fonseca K, Gubbay JB, Bastien N, Li Y, Petric M (2011) Effectiveness of AS03 adjuvanted pandemic H1N1 vaccine: case-control evaluation based on sentinel surveillance system in Canada, autumn 2009. BMJ 342:c7297
Acknowledgments
The authors thank nurses Silvia Fischer, Astrid Wilke, Hanna Zobel, and Anett Sefrin from outpatient transplant clinic for their dedicated assistance with the sample collection. The work was supported by BMBF grant to GERONTOSYS–Verbundprojekt “Primage” to AT, AN, NB.
Conflict of interest
All authors declared no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Vinay Rambal, Karin Müller Chantip Dang-Heine, Petra Reinke, and Nina Babel have contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Rambal, V., Müller, K., Dang-Heine, C. et al. Differential influenza H1N1-specific humoral and cellular response kinetics in kidney transplant patients. Med Microbiol Immunol 203, 35–45 (2014). https://doi.org/10.1007/s00430-013-0312-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-013-0312-3