Abstract
Background
The purpose of this study was to determine the safety and effectiveness, as assessed by risk of bleeding and incidence of deep venous thrombosis (DVT), of administering delayed low-molecular-weight heparin (LMWH) after total knee arthroplasty.
Methods
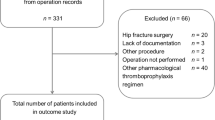
A prospective study of 210 consecutive patients undergoing primary unilateral total knee arthroplasty was undertaken. The patients were randomized into two groups: one of which was managed according to a standard LMWH program (LMWH-s group) and the other with delayed LMWH (LMWH-p). LMWH was initiated 12 h after wound closure in the LMWH-s group, and 24 h after wound closure in the LMWH-p group.
Results
The total blood loss in the first three postoperative days was calculated and all complications were recorded. The mean total blood loss was 435 and 387 mL in the LMWH-s group and LMWH-p group, respectively (p < 0.01). No significant difference in the incidence of symptomatic DVT was observed. The mean length of hospital stay was 7.29 days in the LMWH-s group and 6.56 days in the LMWH-p group (p < 0.05).
Conclusions
After total knee arthroplasty, LMWH-p is safer for bleeding than LMWH-s and equally effective concerning prevention of DVT.

Similar content being viewed by others
References
Hirsh J, Guyatt G, Lewis SZ (2008) Reflecting on eight editions of the American College of Chest Physicians antithrombotic guidelines. Chest 133(6):1293–1295. doi:10.1378/chest.08-0782
Dorr LD, Gendelman V, Maheshwari AV, Boutary M, Wan Z, Long WT (2007) Multimodal thromboprophylaxis for total hip and knee arthroplasty based on risk assessment. J Bone Joint Surg Am 89(12):2648–2657. doi:10.2106/JBJS.F.00235
Lie SA, Engesaeter LB, Havelin LI, Furnes O, Vollset SE (2002) Early postoperative mortality after 67,548 total hip replacements: causes of death and thromboprophylaxis in 68 hospitals in Norway from 1987 to 1999. Acta Orthop Scand 73(4):392–399. doi:10.1080/00016470216312
Howie C, Hughes H, Watts AC (2005) Venous thromboembolism associated with hip and knee replacement over a ten-year period: a population-based study. J Bone Joint Surg Br 87(12):1675–1680. doi:10.1302/0301-620X.87B12.16298
Lassen MR, Gallus A, Raskob GE, Pineo G, Chen D, Ramirez LM (2010) Apixaban versus enoxaparin for thromboprophylaxis after hip replacement. N Engl J Med 363(26):2487–2498. doi:10.1056/NEJMoa1006885
Kakkar AK, Brenner B, Dahl OE, Eriksson BI, Mouret P, Muntz J, Soglian AG, Pap AF, Misselwitz F, Haas S (2008) Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial. Lancet 372(9632):31–39. doi:10.1016/S0140-6736(08)60880-6
Turpie AG, Lassen MR, Eriksson BI, Gent M, Berkowitz SD, Misselwitz F, Bandel TJ, Homering M, Westermeier T, Kakkar AK (2011) Rivaroxaban for the prevention of venous thromboembolism after hip or knee arthroplasty. Pooled analysis of four studies. Thromb Haemost 105(3):444–453. doi:10.1160/TH10-09-0601
Jensen CD, Steval A, Partington PF, Reed MR, Muller SD (2011) Return to theatre following total hip and knee replacement, before and after the introduction of rivaroxaban: a retrospective cohort study. J Bone Joint Surg Br 93(1):91–95. doi:10.1302/0301-620X.93B1.24987
Kulshrestha V, Kumar S (2013) DVT prophylaxis after TKA: routine anticoagulation vs risk screening approach—a randomized study. J Arthroplasty. doi:10.1016/j.arth.2013.05.025
Sindali K, Rose B, Soueid H, Jeer P, Saran D, Shrivastava R (2013) Elective hip and knee arthroplasty and the effect of rivaroxaban and enoxaparin thromboprophylaxis on wound healing. Eur J Orthop Surg Traumatol 23(4):481–486. doi:10.1007/s00590-012-0987-y
Hull R, Raskob G, Pineo G, Rosenbloom D, Evans W, Mallory T, Anquist K, Smith F, Hughes G, Green D et al (1993) A comparison of subcutaneous low-molecular-weight heparin with warfarin sodium for prophylaxis against deep-vein thrombosis after hip or knee implantation. N Engl J Med 329(19):1370–1376. doi:10.1056/NEJM199311043291902
RD Heparin Arthroplasty Group (1994) RD heparin compared with warfarin for prevention of venous thromboembolic disease following total hip or knee arthroplasty. J Bone Joint Surg Am 76(8):1174–1185
Cho KY, Kim KI, Khurana S, Bae DK, Jin W (2013) Is routine chemoprophylaxis necessary for prevention of venous thromboembolism following knee arthroplasty in a low incidence population? Arch Orthop Trauma Surg 133(4):551–559. doi:10.1007/s00402-013-1691-z
Eriksson BI, Dahl OE, Rosencher N, Kurth AA, van Dijk CN, Frostick SP, Prins MH, Hettiarachchi R, Hantel S, Schnee J, Buller HR (2007) Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double-blind, non-inferiority trial. Lancet 370(9591):949–956. doi:10.1016/S0140-6736(07)61445-7
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58(3):277–280
Committee for Proprietary Medicinal Products (CPMP) (2004) Committee for Proprietary Medicinal Products (CPMP): points to consider on adjustment for baseline covariates. Stat Med 23((5):701–709. doi:10.1002/sim.1647
Thirugnanam S, Pinto R, Cook DJ, Geerts WH, Fowler RA (2012) Economic analyses of venous thromboembolism prevention strategies in hospitalized patients: a systematic review. Crit Care 16(2):R43. doi:10.1186/cc11241
Lieberman JR, Barnes CL, Lachiewicz PF, Hanssen AD, Clarke HD, Pellegrini VD Jr (2009) Venous thromboembolism debate in joint arthroplasty. J Bone Joint Surg Am 91 Suppl 5:29–32. doi:10.2106/JBJS.I.00364
Enyart JJ, Jones RJ (2005) Low-dose warfarin for prevention of symptomatic thromboembolism after orthopedic surgery. Ann Pharmacother 39(6):1002–1007. doi:10.1345/aph.1E536
Coventry MB, Nolan DR, Beckenbaugh RD (1973) “Delayed” prophylactic anticoagulation: a study of results and complications in 2,012 total hip arthroplasties. J Bone Joint Surg Am 55(7):1487–1492
Fitzgerald RH, Spiro TE, Trowbridge AA, Gardiner GA, Whitsett TL, O’Connell MB, Ohar JA, Young TR (2001) Prevention of venous thromboembolic disease following primary total knee arthroplasty. A randomized, multicenter, open-label, parallel-group comparison of enoxaparin and warfarin. J Bone Joint Surg Am 83-A(6):900–906
Lotke PA, Lonner JH (2005) Deep venous thrombosis prophylaxis: better living through chemistry—in opposition. J Arthroplasty 20(4 Suppl 2):15–17. doi:10.1016/j.arth.2005.03.002
Parvizi J, Azzam K, Rothman RH (2008) Deep venous thrombosis prophylaxis for total joint arthroplasty: American Academy of Orthopaedic Surgeons guidelines. J Arthroplasty 23(7 Suppl):2–5. doi:10.1016/j.arth.2008.06.028
Confalonieri N, Manzotti A, Pullen C (2004) Is closed-suction drain necessary in unicompartmental knee replacement? a prospective randomised study. Knee 11(5):399–402. doi:10.1016/j.knee.2003.10.001
Montoya RC, Gajra A (2012) Current status of new anticoagulants in the management of venous thromboembolism. Adv Hematol 2012:856341. doi:10.1155/2012/856341
Ageno W, Spyropoulos AC, Turpie AG (2012) Role of new anticoagulants for the prevention of venous thromboembolism after major orthopaedic surgery and in hospitalised acutely ill medical patients. Thromb Haemost 107(6):1027–1034. doi:10.1160/TH11-11-0787
Nieto JA, Espada NG, Merino RG, Gonzalez TC (2012) Dabigatran, rivaroxaban and apixaban versus enoxaparin for thomboprophylaxis after total knee or hip arthroplasty: pool-analysis of phase III randomized clinical trials. Thromb Res 130(2):183–191. doi:10.1016/j.thromres.2012.02.011
McCullagh L, Tilson L, Walsh C, Barry M (2009) A cost-effectiveness model comparing rivaroxaban and dabigatran etexilate with enoxaparin sodium as thromboprophylaxis after total hip and total knee replacement in the irish healthcare setting. Pharmacoeconomics 27(10):829–846. doi:10.2165/11313800-000000000-00000
Acknowledgments
The authors received no grants or outside funding in support of their research or in the preparation of this manuscript. They did not receive payments or other benefits from, or have a commitment or agreement with, any commercial entity.
Conflict of interest
Each author certifies that he has no commercial associations that might pose a conflict of interest in connection with the submitted article.
Author information
Authors and Affiliations
Corresponding author
Additional information
F. Liu and X. Chu are the co-first authors.
Rights and permissions
About this article
Cite this article
Liu, F., Chu, X., Huang, J. et al. Administration of enoxaparin 24 h after total knee arthroplasty: safer for bleeding and equally effective for deep venous thrombosis prevention. Arch Orthop Trauma Surg 134, 679–683 (2014). https://doi.org/10.1007/s00402-014-1939-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-1939-2