Abstract
Purpose
The optimal management of simple hepatic cysts (SHCs) remains controversial. A retrospective review was carried out to evaluate the clinical presentation and surgical consideration of children with SHCs and outcome of management at our institution.
Methods
We performed a retrospective review of all patients diagnosed with SHCs between January 1993 and May 2013. Patient variables included prenatal findings, age, gender, presenting symptoms, signs and diagnostic modality. Operative management and nonoperative follow-up were abstracted.
Results
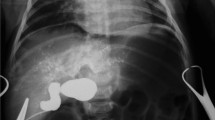
The 67 patients comprised 42 females and 25 males: 16 had prenatally detected, and 51 had postnatally detected hepatic cysts with a mean follow-up of 3.2 years (10 months−12 years). The average age was 5.9 years (0−17 years). Ten patients (six females and four males) were treated surgically. Fifty-seven asymptomatic patients were observed. Of those 57 patients, 9 (17 %) had enlarged cysts, and 1 (2 %) had clinical signs. The average enlargement time was 36 months (6−67 months). The cysts occurred in the right lobe in 47 patients, in the left lobe in 17 patients and in both lobes in 3 patients. The median cyst size for the asymptomatic cases was 2.1 cm (1.5−6 cm) and 13.7 cm (8−25 cm) for the surgery group. A statistically significant difference in cyst size was found between these two groups (p < 0.05). Prenatally detected cysts (n = 5) were subjected to surgery postnatally at an average age of 1.5 months (1 week−6 months). The main indication was the compressive effect of the cyst on the surrounding area. There was one case of hepatomegaly found to be causing pressure symptoms, two cases of respiratory distress, one case of hydroureteronephrosis, and one case of jaundice due to compression of the biliary system. Five patients underwent surgery in the postnatally detected group, and the main indication was a complication of the cyst or progressive enlargement. Symptoms included abdominal discomfort and pain in all five patients: one case exhibited a hemorrhage within the cyst, one case displayed a rupture with possible peritonitis, one case had a 25-cm cyst leading to secondary infection, and two cases were admitted with progressive enlargement with clinical symptoms.
Conclusion
Conservative management of SHCs is practical. Surgical excision is recommended in patients with larger cysts, causing pressure symptoms, or if the cyst size does not seem to involute with intractable abdominal pain or becomes complicated in the follow-up period.



Similar content being viewed by others
References
Benhamou JP, Menu Y (1988) Non parasitic cystic diseases of the liver and intrahepatic biliary tree. In: Blumgart LH (ed) Surgery of the liver and biliary tree. Churchill Livingstone, Edinburgh, pp 1013–1024
Van Sonnenberg E, Wroblicka JT, D’ Agostino HB, Mathieson JR, Casola G, O’Laoida R (1994) Symptomatic hepatic cysts: percutaneous drainage and sclerosis. Radiology 190:387–392
Litwin DE, Taylor BR, Greig P, Langer B (1987) Non-parasitic cysts of the liver-the case for conservative surgical management. Ann Surg 205:45–48
Martin IJ, McKinley AJ, Currie EJ, Holmes P, Garden OJ (1998) Tailoring the management of nonparasitic liver cysts. Ann Surg 228:167–172
Liang P, Cao B, Wang Y, Yu X, Yu D, Dong B (2005) Differential diagnosis of hepatic cystic lesions with gray-scale and color Doppler sonography. J Clin Ultrasound 33:100–105
Henson SW, Gray HK, Dockerty MB (1956) Benign tumours of liver III Solitary cysts. Surg Gynecol Obstet 103:607–612
Cowles RA, Mulholland MW (2000) Solitary hepatic cysts. J Am Coll Surg 191:311–321
Macedo FI (2013) Current management of noninfectious hepatic cystic lesions: A review of the literature. World J Hepatol 5:462–469
Sanfelippo PM, Beahrs OH, Weiland LH (1974) Cystic disease of the liver. Ann Surg 179:922–925
Klinger PJ, Gadenstatter M, Schmid T, Bodner E, Schwelberger HG (1997) Treatment of hepatic cysts in the era of laparoscopic surgery. Br J Surg 84:438–444
Berg C, Baschat AA, Geipel A, Krapp M, Germer U, Smrcek JM, Sigge W, Gembruch U (2002) First-trimester diagnosis of fetal hepatic cyst. Ultrasound Obstet Gynecol 19:287–289
Rogers T, Woodley H, Ramsden W, Wyatt JI, Stringer MD (2007) Solitary liver cysts in children: not always so simple. J Pedr Surg 42:333–339
Avni EF, Rypens F, Donner C, Cuvelliez P, Rodesch F (1994) Hepatic cysts and hyperechogenicities: perinatal assessment and unifying theory on their origin. Pediatr Radiol 24:569–572
Shankar SR, Parelkar SV, Das SA, Mathure AB (2000) An antenally diagnosed solitary, non-parasitic hepatic cyst with duodenal obstruction. Pediatr Surg Int 16:214–215
Charlesworth P, Ade-Ajayi N, Davenport M (2007) Natural history and long-term follow-up of antenatally detected liver cysts. J Pediatr Surg 42(3):494–499
Lai E, Wong J (1990) Symptomatic non-parasitic cysts of the liver. World J Surg 14:452–455
Seo JK, Kim SH, Lee SH, Park JK, Woo SM, Jeong JB, Hwang JH, Ryu JK, Kim JW, Jeong SH, Kim YT, Yoon YB, Lee KU, Kim SH, Kim MA (2010) Appropriate diagnosis of biliary cystic tumors: comparison with atypical hepatic simple cysts. Eur J Gastroenterol Hepatol 22:989–996
Salemis SN, Georgoulis E, Guorgiotis S, Tsohataridis E (2007) Spontaneous rupture of a giant non-parasitic hepatic cyst presenting as an acute surgical abdomen. Ann of Hepatol 6:190–193
Emmermann A, zornig C, Lloyd DM, Peiper M, Bloechle C, Broelsch CE (1997) Laparoscopic treatment of nonparasitic cysts of the liver with omental transposition flap. Surg Endosc 11:734–736
Diez J, Decount J, Gutierrez L, Suhl A, Merello J (1998) Laparoscopic treatment os symptomatic cysts of the liver. Br J Surg 85:25–27
Wellwood TM, Madara JL, Cady B, Haggitt RC (1978) Large intrahepatic cysts and pseudocysts. Pitfalls in diagnosis and treatment. Am J Surg 35:57–64
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Celebi, S., Kutluk, G., Bestas, C.B. et al. Current diagnosis and management of simple hepatic cysts detected prenatally and postnatally. Pediatr Surg Int 30, 599–604 (2014). https://doi.org/10.1007/s00383-014-3509-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-014-3509-7