Abstract
Objectives
The subcommittee on scrotal imaging, appointed by the board of the European Society of Urogenital Radiology (ESUR), have produced guidelines on imaging and follow-up in testicular microlithiasis (TML).
Methods
The authors and a superintendent university librarian independently performed a computer-assisted literature search of medical databases: MEDLINE and EMBASE. A further parallel literature search was made for the genetic conditions Klinefelter’s syndrome and McCune-Albright syndrome.
Results
Proposed guidelines are: follow-up is not advised in patients with isolated TML in the absence of risk factors (see Key Points below); annual ultrasound (US) is advised for patients with risk factors, up to the age of 55; if TML is found with a testicular mass, urgent referral to a specialist centre is advised.
Conclusion
Consensus opinion of the scrotal subcommittee of the ESUR is that the presence of TML alone in the absence of other risk factors is not an indication for regular scrotal US, further US screening or biopsy. US is recommended in the follow-up of patients at risk, where risk factors other than microlithiasis are present. Risk factors are discussed and the literature and recommended guidelines are presented in this article.
Key Points
• Follow up advised only in patients with TML and additional risk factors.
• Annual US advised for patients with risk factors up to age 55.
• If TML is found with testicular mass, urgent specialist referral advised.
• Risk factors – personal/ family history of GCT, maldescent, orchidopexy, testicular atrophy.
Similar content being viewed by others
References
De Jong BW, De Gouveia Brazao CA, Stoop H, Wolffenbuttel KP, Oosterhuis JW, Puppels GJ et al (2004) Raman spectroscopic analysis identifies testicular microlithiasis as intratubular hydroxyapatite. J Urol 171(1):92–96
Kim B, Winter TC, Ryu JA (2003) Testicular microlithiasis: clinical significance and review of the literature. Eur Radiol 13(12):2567–2576
Renshaw AA (1998) Testicular calcifications: incidence, histology and proposed pathological criteria for testicular microlithiasis. J Urol 160(5):1625–1628
Drut R, Monica R (2002) Testicular microlithiasis: histologic and immunohistochemical findings in 11 pediatric cases. Pediatr Dev Pathol 5(6):544–550
Bennett HF, Middleton WD, Bullock AO, Teefey SA (2001) Testicular microlithiasis: US follow-up. Radiology 218(2):359–363
Backus ML, Mack LA, Middleton WD, King BF, Winter TC 3rd, True LD (1994) Testicular microlithiasis: imaging appearances and pathologic correlation. Radiology 192(3):781–785
Jungwirth A, Diemer T, Dohle GR, Giwercman A, Kopa Z, Tournaye H, Krausz C (2013) Guidelines on male infertility: European Association of Urology. Available from: http://www.uroweb.org/gls/pdf/16_Male_Infertility_LR.pdf
Elzinga-Tinke JE, Sirre ME, Looijenga LH, van Casteren N, Wildhagen MF, Dohle GR (2010) The predictive value of testicular ultrasound abnormalities for carcinoma in situ of the testis in men at risk for testicular cancer. Int J Androl 33(4):597–603
DeCastro BJ, Peterson AC, Costabile RA (2008) A 5-year followup study of asymptomatic men with testicular microlithiasis. J Urol 179(4):1420–1403
Montgomery JS, Bloom DA (2011) The diagnosis and management of scrotal masses. Med Clin North Am 95(1):235–244
Tan IB, Ang KK, Ching BC, Mohan C, Toh CK, Tan MH (2010) Testicular microlithiasis predicts concurrent testicular germ cell tumors and intratubular germ cell neoplasia of unclassified type in adults: a meta-analysis and systematic review. Cancer 116(19):4520–4532
Miller FN, Rosairo S, Clarke JL, Sriprasad S, Muir GH, Sidhu PS (2007) Testicular calcification and microlithiasis: association with primary intra-testicular malignancy in 3,477 patients. Eur Radiol 17(2):363–369
Manecksha RP, Fitzpatrick JM (2009) Epidemiology of testicular cancer. BJU Int 104(9 Pt B):1329–1333
Skakkebaek NE (2003) Testicular dysgenesis syndrome. Horm Res 60(Suppl 3):49
Skakkebaek NE, Holm M, Hoei-Hansen C, Jorgensen N, Rajpert-De E, Mayer F et al (2003) Association between testicular dysgenesis syndrome (TDS) and testicular neoplasia: evidence from 20 adult patients with signs of maldevelopment of the testis. APMIS 111(1):1–11
Joensen UN, Jorgensen N, Rajpert-De E, Skakkebaek NE (2008) Testicular dysgenesis syndrome and Leydig cell function. Basic Clin Pharmacol Toxicol 102(2):155–161
Martin OV, Shialis T, Lester JN, Scrimshaw MD, Boobis AR, Voulvoulis N (2008) Testicular dysgenesis syndrome and the estrogen hypothesis: a quantitative meta-analysis. Environ Health Perspect 116(2):149–157
Wohlfahrt-Veje C, Main KM, Skakkebaek NE (2009) Testicular dysgenesis syndrome: foetal origin of adult reproductive problems. Clin Endocrinol 71(4):459–465
James WH (2010) Further grounds for abandoning the concept of testicular dysgenesis syndrome: a response to the paper of Akre and Richiardi (2009). Hum Reprod 25(4):1084–1086
Akre O, Richiardi L (2009) Does a testicular dysgenesis syndrome exist? Hum Reprod 24(9):2053–2060
Cvancarova M, Oldenburg J, Sprauten M, Stensheim H, Fossa SD (2011) Reproduction rates prior to diagnosis of testicular cancer: does the testicular dysgenesis syndrome exist? J Clin Oncol 29(15 Suppl 1)
Greene MH, Kratz CP, Mai PL, Mueller C, Peters JA, Bratslavsky G et al (2010) Familial testicular germ cell tumors in adults: 2010 summary of genetic risk factors and clinical phenotype. Endocr Relat Cancer 17(2):R109–R121
Hemminki K, Chen B (2006) Familial risks in testicular cancer as aetiological clues. Int J Androl 29(1):205–210
Mai PL, Chen BE, Tucker K, Friedlander M, Phillips KA, Hogg D et al (2009) Younger age-at-diagnosis for familial malignant testicular germ cell tumor. Fam Cancer 8(4):451–456
Coffey J, Huddart RA, Elliott F, Sohaib SA, Parker E, Dudakia D et al (2007) Testicular microlithiasis as a familial risk factor for testicular germ cell tumour. Br J Cancer 97(12):1701–1706
Korde LA, Premkumar A, Mueller C, Rosenberg P, Soho C, Bratslavsky G et al (2008) Increased prevalence of testicular microlithiasis in men with familial testicular cancer and their relatives. Br J Cancer 99(10):1748–1753
Goede J, Hack WW, Sijstermans K, van der Voort-Doedens LM, Van der Ploeg T, Meij-de Vries A et al (2011) Normative values for testicular volume measured by ultrasonography in a normal population from infancy to adolescence. Horm Res Paediatr 76(1):56–64
Okada H, Fujioka H, Tatsumi N, Kanzaki M, Okuda Y, Fujisawa M et al (1999) Klinefelter’s syndrome in the male infertility clinic. Hum Reprod 14(4):946–952
Boyce AM, Chong WH, Shawker TH, Pinto PA, Linehan WM, Bhattacharryya N et al (2012) Characterization and management of testicular pathology in McCune-Albright syndrome. J Clin Endocrinol Metab 97(9):E1782–E1790
Daneman A, Daneman D (2007) McCune-Albright syndrome. J Pediatr Endocrinol Metab 20(12):1265
Thomas K, Wood SJ, Thompson AJ, Pilling D, Lewis-Jones DI (2000) The incidence and significance of testicular microlithiasis in a subfertile population. Br J Radiol 73(869):494–497
Albers P, Albrecht W, Algaba F, Bokemeyer C, Cohn-Cedermark G, Fizazi K et al (2011) EAU guidelines on testicular cancer: 2011 update. Eur Urol 60(2):304–319
Butruille C, Marcelli F, Ghoneim T, Lemaitre L, Puech P, Leroy X et al (2012) Management of testicular lesions in a population of infertile patients. [French] Prise en charge des nodules testiculaires dans une population de patients infertiles. Prog Urol 22(1):45–52
Furness PD 3rd, Husmann DA, Brock JW 3rd, Steinhardt GF, Bukowski TP, Freedman AL et al (1998) Multi-institutional study of testicular microlithiasis in childhood: a benign or premalignant condition? J Urol 160(3 Pt 2):1151–1154, discussion 78
Goede J, Hack WWM, van der Voort-Doedens LM, Sijstermans K, Pierik FH (2009) Prevalence of testicular microlithiasis in asymptomatic males 0 to 19 years old. J Urol 182(Suppl 4):1516–1520
Chiang LW, Yap TL, Asiri MM, Phaik Ong CC, Low Y, Jacobsen AS (2012) Implications of incidental finding of testicular microlithiasis in paediatric patients. J Pediatr Urol 8(2):162–165
Goede J, Hack WW (2012) Clinical aspects of testicular microlithiasis in boys: a review. J Pediatr Urol 8(5):459–469
Deganello A, Svasti-Salee D, Allen P, Clarke JL, Sellars ME, Sidhu PS (2012) Scrotal calcification in a symptomatic paediatric population: prevalence, location, and appearance in a cohort of 516 patients. Clin Radiol 67(9):862–867
Hoei-Hansen CE, Olesen IA, Jorgensen N, Carlsen E, Holm M, Almstrup K et al (2007) Current approaches for detection of carcinoma in situ testis. Int J Androl 30(4):398–404, discussion 404–405
Acknowledgments
The scientific guarantor of this publication is Jonathan Richenberg. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional review board approval was not required because not applicable. Methodology: prospective/retrospective
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
Patient leaflet for testicular microlithiasis
What is testicular microlithiasis?
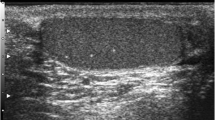
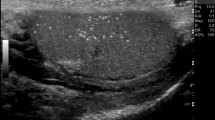
Small lumps of calcium lie in the small tubes within the testicle. There must be at least 5 such calcifications in one (or both) testicles before the label testicular microlithiasis (TML) is applied. TML is seen in about 2 or 3 men in every hundred.
How is TML detected?
The calcium lumps cannot be felt and they do NOT cause discomfort. They can only be seen on ultrasound. In other words, TML was discovered incidentally during your ultrasound scan of the testes.
Why is TML important?
At the end of the 1990s, there was some concern that TML might lead to cancer of the testicle. Since then, many studies across the world have looked at TML. They have NOT confirmed the initial worries.
There is no evidence that TML on its own leads to cancer.
What should I do?
Like every man, including men who do not have TML, you should practice monthly self-examination of the testicles. If you are uncertain about how to do this, please ask your doctor. Nothing else is required. You do not need regular ultrasound scans. The calcium in the testicles is not related to your diet or to any sexual or other activity.
What should I do if I feel a new lump during self-examination?
Please contact your family doctor or specialist. Your family doctor or specialist will examine you and if thought appropriate will refer you on for a specialist opinion. It is likely that you will be referred also for an urgent ultrasound scan. This will be usually at the hospital where the initial scan was performed.
Appendix 2
Checklist to be completed in men discovered to have TML
If you discover a patient has TML during ultrasound scanning, risk factors for developing GCT should be ascertained.
Risk factor | Comments | Yes >=5 ML per FoV | Yes Diffuse | No TML i.e. no FoV contains 5 or more microliths |
|---|---|---|---|---|
Maldescent | Ask patient for relevant history | Annual US | Annual US | Discharge |
Orchidopexy | Ask patient for relevant history | Annual US | Annual US | Discharge |
Previous GCT | Likely to have orchidectomy so this should be easy to ascertain. If there is any doubt, ask the patient | Annual US | Annual US | Discharge |
Genetic disease | Ask patient for relevant history | Repeat US at 6 and 12 months, D/C if no nodule >3mm | Refer | Discharge |
Family history of GCT | Ask patient for relevant history | Encourage self-examination and offer open access | Encourage self-examination and offer open access | Discharge |
Atrophic testis | Should be noted during the ultrasound examination | Annual US | Annual US | Discharge |
Rights and permissions
About this article
Cite this article
Richenberg, J., Belfield, J., Ramchandani, P. et al. Testicular microlithiasis imaging and follow-up: guidelines of the ESUR scrotal imaging subcommittee. Eur Radiol 25, 323–330 (2015). https://doi.org/10.1007/s00330-014-3437-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3437-x