Abstract
Purpose
KX2-391 is an oral non-ATP-competitive inhibitor of Src kinase and tubulin polymerization. In phase 1 trials, prostate-specific antigen (PSA) declines were seen in patients with advanced prostate cancer. We conducted a single-arm phase 2 study evaluating KX2-391 in men with chemotherapy-naïve bone-metastatic castration-resistant prostate cancer (CRPC).
Methods
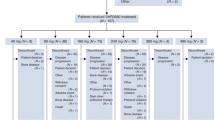
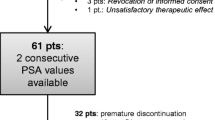
We treated 31 patients with oral KX2-391 (40 mg twice-daily) until disease progression or unacceptable toxicity. The primary endpoint was 24-week progression-free survival (PFS); a 50 % success rate was pre-defined as clinically significant. Secondary endpoints included PSA progression-free survival (PPFS) and PSA response rates. Exploratory outcomes included pharmacokinetic studies, circulating tumor cell (CTC) enumeration, and analysis of markers of bone resorption [urinary N-telopeptide (uNTx); C-telopeptide (CTx)] and formation [bone alkaline phosphatase (BAP); osteocalcin].
Results
The trial closed early after accrual of 31 patients, due to a pre-specified futility rule. PFS at 24 weeks was 8 %, and median PFS was 18.6 weeks. The PSA response rate (≥30 % decline) was 10 %, and median PPFS was 5.0 weeks. Additionally, 18 % of men with unfavorable (≥5) CTCs at baseline converted to favorable (<5) CTCs with treatment. The proportion of men with declines in bone turnover markers was 32 % for uNTx, 21 % for CTx, 10 % for BAP, and 25 % for osteocalcin. In pharmacokinetic studies, median C max was 61 (range 16–129) ng/mL, and median AUC was 156 (35–348) ng h/mL. Common toxicities included hepatic derangements, myelosuppression, fatigue, nausea, and constipation.
Conclusion
KX2-391 dosed at 40 mg twice-daily lacks antitumor activity in men with CRPC, but has modest effects on bone turnover markers. Because a C max of ≥142 ng/mL is required for tubulin polymerization inhibition (defined from preclinical studies), higher once-daily dosing will be used in future trials.



Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62:10–29
Antonarakis ES, Eisenberger MA (2011) Expanding treatment options for metastatic prostate cancer. N Engl J Med 364:2055–2058
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Chang YM, Kung HJ, Evans CP (2007) Non-receptor tyrosine kinases in prostate cancer. Neoplasia 9:90–100
Posadas EM, Al-Ahmadie H, Robinson VL et al (2009) FYN is overexpressed in human prostate cancer. BJU Int 103:171–177
Fizazi K (2007) The role of Src in prostate cancer. Ann Oncol 18:1765–1773
Araujo JC, Logothetis CJ (2009) Targeting Src signaling in metastatic bone disease. Int J Cancer 124:1–6
Tatarov O, Mitchell TJ, Seywright M et al (2009) Src family kinase activity is upregulated in hormone-refractory prostate cancer. Clin Cancer Res 15:3540–3549
Yu EY, Wilding G, Posadas E et al (2009) Phase II study of dasatinib in patients with metastatic castration-resistant prostate cancer. Clin Cancer Res 15:7421–7428
Araujo JC, Mathew P, Armstrong AJ et al (2012) Dasatinib combined with docetaxel for castration-resistant prostate cancer: results from a phase 1–2 study. Cancer 118:63–71
Fallah-Tafti A, Foroumadi A, Tiwari R et al (2011) Thiazolyl N-benzyl-substituted acetamide derivatives: synthesis, Src kinase inhibitory and anticancer activities. Eur J Med Chem 46:4853–4858
Hangauer D, Gelman I, Dyster L et al (2007) Potent and selective in vitro and in vivo inhibition of tumor proliferation by KXO1, a novel non-ATP competitive Src inhibitor. Proc Am Assoc Cancer Res 2007: abstract 3245
Bu Y, Gao L, Smolinski M et al (2008) KX01 (KX2–391), a Src-family kinase inhibitor targeting the peptide-binding domain, suppresses oncogenic proliferation in vitro and in vivo. Proc Am Assoc Cancer Res 2008: abstract 4983
Adjei AA, Cohen RB, Kurzrock R et al (2009) Results of a phase I trial of KX2-391, a novel non-ATP competitive substrate-pocket directed Src inhibitor, in patients with advanced malignancies. J Clin Oncol 27(Suppl): abstract 3511
Scher HI, Halabi S, Tannock I et al (2008) Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol 26:1148–1159
Morris MJ, Basch EM, Wilding G et al (2009) Department of Defense prostate cancer clinical trials consortium: a new instrument for prostate cancer clinical research. Clin Genitourin Cancer 7:51–57
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 92:205–216
Shaffer DR, Leversha MA, Danila DC et al (2007) Circulating tumor cell analysis in patients with progressive castration-resistant prostate cancer. Clin Cancer Res 13:2023–2029
Franke RM, Carducci MA, Rudek MA et al (2010) Castration-dependent pharmacokinetics of docetaxel in patients with prostate cancer. J Clin Oncol 28:4562–4567
Fizazi K, Lipton A, Mariette X et al (2009) Randomized phase II trial of denosumab in patients with bone metastases from prostate cancer, breast cancer, or other neoplasms after intravenous bisphosphonates. J Clin Oncol 27:1564–1571
Carducci MA, Saad F, Abrahamsson PA et al (2007) A phase 3 randomized controlled trial of the efficacy and safety of atrasentan in men with metastatic hormone-refractory prostate cancer. Cancer 110:1959–1966
Simon R (1989) Optimal two-stage designs for phase II clinical trials. Control Clin Trials 10:1–10
Lara PN Jr, Longmate J, Evans CP et al (2009) A phase II trial of the Src-kinase inhibitor AZD0530 in patients with advanced castration-resistant prostate cancer: a California Cancer Consortium study. Anticancer Drugs 20:179–184
Lipton A, Cook R, Saad F et al (2008) Normalization of bone markers is associated with improved survival in patients with bone metastases from solid tumors and elevated bone resorption receiving zoledronic acid. Cancer 113:193–201
Yu EY, Massard C, Gross ME et al (2011) Once-daily dasatinib: expansion of phase II study evaluating safety and efficacy of dasatinib in patients with metastatic castration-resistant prostate cancer. Urology 77:1166–1171
Acknowledgments
We thank the patients who volunteered to participate in this study and their families, as well as the staff members who cared for them at each site. Supported by Kinex Pharmaceuticals LLC; a Conquer Cancer Foundation 2009 Young Investigator Award; an NIH/NCI training grant (T32 CA009071); the Department of Defense Prostate Cancer Research Program (PC051382); and the Prostate Cancer Foundation.
Conflict of interest
E.S.A, E.I.H, E.M.P, M.R.H, J.Y.B, E.Y.Y., S.YC., and G.J.F. have no relevant conflicts of interest. G.E.W. is a paid consultant/advisor for Kinex Pharmaceuticals. D.H.G is the Chief Scientific Officer of Kinex Pharmaceuticals, and has stock ownership in Kinex Pharmaceuticals. M.R.K. is the Chief Medical Officer of Kinex Pharmaceuticals, and has stock ownership in Kinex Pharmaceuticals. L.M.D. is the Vice President of Operations of Kinex Pharmaceuticals, and has stock ownership in Kinex Pharmaceuticals. M.A.C. received research funding from Kinex Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Appendix: Derivation of 142 ng/mL as the plasma threshold for KX2-391 activity
Appendix: Derivation of 142 ng/mL as the plasma threshold for KX2-391 activity
KX2-391 is 83 % protein-bound in the serum. This correlates with an approximate fourfold reduction in potency for both mechanisms of action (Src inhibition, and tubulin polymerization inhibition) measured in whole cells in the presence of human plasma. The IC50 for Src inhibition in human tumor cells is about 25 nM in the absence of human plasma and about 100 nM in the presence of human plasma. However, the IC50 for tubulin polymerization inhibition in human tumor cells is about 125 nM in the absence of plasma and about 500 nM in the presence of plasma. 500 nM of KX2-391 corresponds to a plasma concentration of 216 ng/mL. In mouse HT29 xenograft studies, it was determined that KX2-391 partitions into tumor tissue versus plasma at a ratio of 1.52. This reduces the required plasma concentration by 1.52-fold (i.e. 216/1.52 = 142 ng/mL). Based upon these assumptions, both mechanisms of action of KX2-391 will be engaged in patients when plasma levels reach approximately 142 ng/mL or higher (which should result in tumor tissue levels of at least 216 ng/mL). In addition, the drug level needs to remain above 142 ng/mL for long enough to cause significant apoptosis in tumor cells. An 80 mg dose of KX2-391 produces a C max of 242 ng/mL, and plasma levels stay above the 142 ng/mL threshold for about 3 h [14]. This suggests that significant efficacy may be obtained with KX2-391 when it is dosed at or above 80 mg in patients. Preclinical toxicity and efficacy studies in mice indicated that once-daily dosing of KX2-391 was less toxic, allowing at least threefold higher drug doses to be administered, and appeared more efficacious than twice-daily dosing. Once-daily KX2-391 dosing in ongoing trials (NCT01397799) suggests that the maximum tolerated dose will be above 80 mg.
Rights and permissions
About this article
Cite this article
Antonarakis, E.S., Heath, E.I., Posadas, E.M. et al. A phase 2 study of KX2-391, an oral inhibitor of Src kinase and tubulin polymerization, in men with bone-metastatic castration-resistant prostate cancer. Cancer Chemother Pharmacol 71, 883–892 (2013). https://doi.org/10.1007/s00280-013-2079-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-013-2079-z