Abstract
Purpose
Temsirolimus, a selective inhibitor of mammalian target of rapamycin, is an approved treatment for patients with advanced renal cell carcinoma (RCC). This study assessed the effect of intravenous (i.v.) temsirolimus 25 mg, the recommended dose for patients with RCC, on the corrected QT (QTc) interval.
Methods
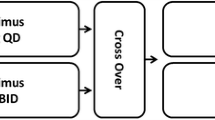
This 3-period crossover study enrolled healthy subjects. In periods 1 and 2, subjects received i.v. placebo either alone or with open-label oral moxifloxacin. In period 3, subjects received a single dose of temsirolimus 25 mg. The primary statistical objective was to estimate the effect of temsirolimus compared with placebo on change from time-matched baseline QTc at the end of infusion (0.5 h). Assay sensitivity was evaluated by the effect of moxifloxacin on change from time-matched baseline QTc compared with placebo.
Results
In total, 58 subjects were enrolled. Temsirolimus had no effect on QTc interval in the primary analysis. At 11 of 12 secondary time points, the upper bound for the temsirolimus QTc 90% confidence intervals for the time-matched change from baseline difference from placebo was <10 ms, with no evidence of QTc trends or relationship to concentrations of temsirolimus or its major metabolite, sirolimus. Moxifloxacin, the positive control, produced a significant increase in the QTc interval compared with placebo 0.5–4 h post-dose (P < 0.0001). No subject had a QTc interval exceeding 450 ms or a change from baseline of >30 ms.
Conclusions
Therapeutic exposure to temsirolimus is not associated with clinically significant changes in QTc intervals in healthy adults.



Similar content being viewed by others
References
Farkas AS, Nattel S (2010) Minimizing repolarization-related proarrhythmic risk in drug development and clinical practice. Drugs 70:573–603
Salvi V, Karnad DR, Panicker GK, Kothari S (2010) Update on the evaluation of a new drug for effects on cardiac repolarization in humans: issues in early drug development. Br J Pharmacol 159:34–48
Shah RR (2002) The significance of QT interval in drug development. Br J Clin Pharmacol 54:188–202
Abraham RT, Gibbons JJ (2007) The mammalian target of rapamycin signaling pathway: twists and turns in the road to cancer therapy. Clin Cancer Res 13:3109–3114
Boni JP, Hug B, Leister C, Sonichsen D (2009) Intravenous temsirolimus in cancer patients: clinical pharmacology and dosing considerations. Semin Oncol 36:S18–S25
Hudes G, Carducci M, Tomczak P, Dutcher J, Figlin R, Kapoor A, Staroslawska E, Sosman J, McDermott D, Bodrogi I, Kovacevic Z, Lesovoy V, Schmidt-Wolf I, Barbarash O, Gokmen E, O’Toole T, Lustgarten S, Moore L, Motzer R, Global ARCC Trial (2007) Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med 356:2271–2281
Food and Drug Administration (2005) International Conference on Harmonisation; guidance on E14 clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drug. Fed Regist 70:61134–61135
Hug B, Abbas R, Leister C, Burns J, Sonnichsen D (2010) A single-dose, crossover, placebo- and moxifloxacin-controlled study to assess the effects of neratinib (HKI-272) on cardiac repolarization in healthy adult subjects. Clin Cancer Res 16:4016–4023
Boni J, Leister C, Burns J, Cincotta M, Hug B, Moore L (2007) Pharmacokinetic profile of temsirolimus with concomitant administration of cytochrome P450-inducing medications. J Clin Pharmacol 47:1430–1439
Boni J, Abbas R, Leister C, Burns J, Jordan R, Hoffmann M, DeMaio W, Hug B (2009) Disposition of desipramine, a sensitive cytochrome P450 2D6 substrate, when coadministered with intravenous temsirolimus. Cancer Chemother Pharmacol 64:263–270
Torisel [package insert] (2011) Pfizer Inc, Philadelphia
Avelox [package insert] (2008) Bayer HealthCare Pharmaceuticals, Wayne
Punt CJ, Boni J, Bruntsch U, Peters M, Thielert C (2003) Phase I and pharmacokinetic study of CCI-779, a novel cytostatic cell-cycle inhibitor, in combination with 5-fluorouracil and leucovorin in patients with advanced solid tumors. Ann Oncol 14:931–937
Evans WE, Schentag JJ, Jusko WJ (eds) (1992) Applied pharmacokinetics: principles of therapeutic drug monitoring. Lippincott Williams & Wilkins, New York
Zareba W, Moss AJ, Rosero SZ, Hajj-Ali R, Konecki J, Andrews M (1997) Electrocardiographic findings in patients with diphenhydramine overdose. Am J Cardiol 80:1168–1173
Atkins MB, Hidalgo M, Stadler WM, Logan TF, Dutcher JP, Hudes GR, Park Y, Liou SH, Marshall B, Boni JP, Dukart G, Sherman ML (2004) Randomized phase II study of multiple dose levels of CCI-779, a novel mammalian target of rapamycin kinase inhibitor, in patients with advanced refractory renal cell carcinoma. J Clin Oncol 22:909–918
Boni JP, Leister C, Burns J, Hug B (2008) Differential effects of ketoconazole on exposure to temsirolimus following intravenous infusion of temsirolimus. Br J Cancer 98:1797–1802
Hess G, Herbrecht R, Romaguera J, Verhoef G, Crump M, Gisselbrecht C, Laurell A, Offner F, Strahs A, Berkenblit A, Hanushevsky O, Clancy J, Hewes B, Moore L, Coiffier B (2009) Phase III study to evaluate temsirolimus compared with investigator’s choice therapy for the treatment of relapsed or refractory mantle cell lymphoma. J Clin Oncol 27:3822–3829
Benton RE, Sale M, Flockhart DA, Woosley RL (2000) Greater quinidine-induced QTc interval prolongation in women. Clin Pharmacol Ther 67:413–418
Boni JP, Leister C, Bender G, Fitzpatrick V, Twine N, Stover J, Dorner A, Immermann F, Burczynski ME (2005) Population pharmacokinetics of CCI-779: correlations to safety and pharmacogenomic responses in patients with advanced renal cancer. Clin Pharmacol Ther 77:76–89
Boni JP, Zhou S, Burns J, Smith K, Liao S (2006) Integrated population pharmacokinetic analysis of temsirolimus in cancer patients following weekly IV treatments [abstract 552]. Eur J Cancer Suppl 4:167
Schmidinger M, Zielinski CC, Vogl UM, Bojic A, Bojic M, Schukro C, Ruhsam M, Hejna M, Schmidinger H (2008) Cardiac toxicity of sunitinib and sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol 26:5204–5212
Force T, Krause DS, Van Etten RA (2007) Molecular mechanisms of cardiotoxicity of tyrosine kinase inhibition. Nat Rev Cancer 7:332–344
Girardi F, Franceschi E, Brandes AA (2010) Cardiovascular safety of VEGF-targeting therapies: current evidence and handling strategies. Oncologist 15:683–694
Bello CL, Mulay M, Huang X, Patyna S, Dinolfo M, Levine S, Van VA, Toh M, Baum C, Rosen L (2009) Electrocardiographic characterization of the QTc interval in patients with advanced solid tumors: pharmacokinetic- pharmacodynamic evaluation of sunitinib. Clin Cancer Res 15:7045–7052
Keisner SV, Shah SR (2011) Pazopanib: the newest tyrosine kinase inhibitor for the treatment of advanced or metastatic renal cell carcinoma. Drugs 71:443–454
Tolcher AW, Appleman LJ, Shapiro GI, Mita AC, Cihon F, Mazzu A, Sundaresan PR (2011) A phase I open-label study evaluating the cardiovascular safety of sorafenib in patients with advanced cancer. Cancer Chemother Pharmacol 67:751–764
Acknowledgments
This study was sponsored by Wyeth Research, which was acquired by Pfizer Inc in October 2009. We thank all of the participants, research nurses, study coordinators, and operations staff who participated in this study. We also thank Christine H. Blood, PhD, of Peloton Advantage, LLC, for assistance with manuscript preparation, which was funded by Pfizer Inc.
Conflict of interest
At the time of this study, all authors were employees of Wyeth Pharmaceuticals. In addition, J. Boni, C. Leister, and D. Sonnichsen were stockholders in Wyeth.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boni, J.P., Leister, C., Hug, B. et al. A single-dose placebo- and moxifloxacin-controlled study of the effects of temsirolimus on cardiac repolarization in healthy adults. Cancer Chemother Pharmacol 69, 1433–1442 (2012). https://doi.org/10.1007/s00280-012-1845-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-012-1845-7