Abstract
Context
Percutaneous injuries occur frequently during surgical procedures and represent a significant occupational hazard to operating room personnel.
Objectives
To evaluate the feasibility of performing select general surgical procedures using a combination of non-sharp devices and techniques to replace the conventional use of scalpels and needles.
Design, Setting, and Participants
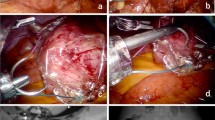
Candidate procedures for which sharpless techniques could replace conventional scalpels and suture needles were identified preoperatively in an urban, university-based general surgical practice over a 1-year period (June 2003–June 2004). Non-sharp techniques included monomeric 2-octyl cyanoacrylate adhesive, electrocautery, tissue stapler, and minimally invasive instrumentation. Conventional scalpels and suture needles were readily available and used whenever necessary.
Main Outcome Measures
We rated the feasibility of performing specific procedures without sharps. We also documented the rate of overall reversion to sharps during operations on patients that had been identified preoperatively as candidates for sharpless surgery.
Results
Of 358 procedures performed in the general surgery university practice, 91 were identified preoperatively as appropriate for sharpless surgery. Of these, 86.8% (79/91) were completed without the use of sharps, including 13/22 (59.1%) open laparotomy procedures, 20/22 (90.9%) laparoscopic procedures, and 46/47 (97.8%) soft tissue procedures. Intraoperative reversion to sharps occurred in 12 cases when deemed necessary by the surgeon.
Conclusions
Select common procedures can be performed entirely with sharpless techniques, eliminating the risk to surgical personnel associated with intraoperative percutaneous injuries.
Similar content being viewed by others
References
Gerberding JL, Littell C, Tarkington A, et al. Risk of exposure of surgical personnel to patients’ blood during surgery at San Francisco General Hospital. N Engl J Med 1990;322:1788–1793
Cobelens F. Needlestick injuries, surgeons, and HIV risks. Lancet 1990;335:924
Tokars JI, Bell DM, Culver DH, et al. Percutaneous injuries during surgical procedures. J Am Med Assoc 1992;267:2899–2904
Quebbeman EJ, Telford GL, Hubbard S, et al. Risk of blood contamination and injury to operating room personnel. Ann Surg 1991;214:614–620
Leentvaar-Kuijpers A, Dekker MM, Coutinho RA, et al. Needlestick injuries, surgeons, and HIV risks. Lancet 1990;335:546–547
Jagger J, Bentley M, Tereskerz P. A study of patterns and prevention of blood exposures in OR personnel. AORN J 1998;67:979–981, 983–984, 986–987 passim
Panlilio AL, Foy DR, Edwards JR, et al. Blood contacts during surgical procedures. J Am Med Assoc 1991;265:1533–1537
Gerberding JL. Clinical practice. occupational exposure to HIV in health care settings. N Engl J Med 2003;348:826–833
Weiss ES, Makary MA, Wang T, et al. Prevalence of blood-borne pathogens in an urban, university-based general surgical practice. Ann Surg 2005;241:803–807; discussion 807–809
Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med 1999;341:556–562
Centers for Disease Control and Prevention (CDC). Viral hepatitis C fact sheet. Available at: http://www.cdc.gov/ncidod/diseases/hepatitis/c/fact.htm. Accessed July 15, 2005
Martinson FE, Weigle KA, Mushahwar IK, et al. Seroepidemiological survey of hepatitis B and C virus infections in Ghanaian children. J Med Virol 1996;48:278–283
Sagoe-Moses C, Pearson RD, Perry J, et al. Risks to health care workers in developing countries. N Engl J Med 2001;345:538–541
2004 Report on the Global AIDS Epidemic. Geneva: Joint United Nations Program on HIV/AIDS; 2004
Steinbrook R. The AIDS epidemic in 2004. N Engl J Med 2004;351:115–117
Joint United Nations Programme on HIV/AIDS UNAIDS. AIDS epidemic update: December 1999. AIDS Anal Afr 2000;10:2
Kearns SR, Connolly EM, McNally S, et al. Randomized clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg 2001;88:41–44
Franchi M, Ghezzi F, Benedetti-Panici PL, et al. A multicentre collaborative study on the use of cold scalpel and electrocautery for midline abdominal incision. Am J Surg 2001;181:128–132
Quinn J, Wells G, Sutcliffe T, et al. A randomized trial comparing octylcyanoacrylate tissue adhesive and sutures in the management of lacerations. J Am Med Assoc 1997;277:1527–1530
Gennari R, Rotmensz N, Ballardini B, et al. A prospective, randomized, controlled clinical trial of tissue adhesive (2-octylcyanoacrylate) versus standard wound closure in breast surgery. Surgery 2004;136:593–599
Singer AJ, Quinn JV, Clark RE, and the TraumaSeal Study Group, et al. Closure of lacerations and incisions with octylcyanoacrylate: a multicenter randomized controlled trial. Surgery 2002;131:270–276
String A, Berber E, Foroutani A, et al. Use of the optical access trocar for safe and rapid entry in various laparoscopic procedures. Surg Endosc 2001;15:570–573
McKernan JB, Finley CR. Experience with optical trocar in performing laparoscopic procedures. Surg Laparosc Endosc Percutan Tech 2002;12:96–99
Barker DE, Kaufman HJ, Smith LA, et al. Vacuum pack technique of temporary abdominal closure: a 7-year experience with 112 patients. J Trauma 2000;48:201–206; discussion 206–207
Garner GB, Ware DN, Cocanour CS, et al. Vacuum-assisted wound closure provides early fascial reapproximation in trauma patients with open abdomens. Am J Surg 2001;182:630–638
Jagger J, Balon M. Suture needle and scalpel blade injuries: frequent but underreported. Infect Control Steril Technol 1996;2:15–22
Short L, Chamberland M, Culver D, et al. Underreporting of needlestick injuries (NSIs) among health care workers (HCWs). Infect Control Hosp Epidemiol 1994;15
Bennett NT, Howard RJ. Quantity of blood inoculated in a needlestick injury from suture needles. J Am Coll Surg 1994;178:107–110
Tokars JI, Chamberland ME, Schable CA, et al. A survey of occupational blood contact and HIV infection among orthopedic surgeons. The American Academy of Orthopedic Surgeons Serosurvey Study Committee. J Am Med Assoc 1992;268:489–494
Lowenfels AB, Wormser GP, Jain R. Frequency of puncture injuries in surgeons and estimated risk of HIV infection. Arch Surg 1989;124:1284–1286
Jagger J, Bentley M, Juillet E. Direct cost of follow-up for percutaneous and mucocutaneous exposures to at-risk body fluids: data from two hospitals. Adv Exposure Prevent 1998;3:54–56
Guimet M, Mendicino S, Rockett MS. Percutaneous injuries in a high-volume podiatric surgical residency program. J Foot Ankle Surg 2001;40:15–20
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Makary, M.A., Pronovost, P.J., Weiss, E.S. et al. Sharpless Surgery: A Prospective Study of the Feasibility of Performing Operations using Non-sharp Techniques in an Urban, University-based Surgical Practice. World J. Surg. 30, 1224–1229 (2006). https://doi.org/10.1007/s00268-005-0605-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0605-9