Abstract
Introduction and hypothesis
The aim of our study was to determine the prevalence of pelvic organ prolapse (POP) symptoms in a community-dwelling population in the United Kingdom.
Methods
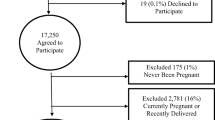
All women over the age of 18 from a community practice were sent the validated International Consultation on Incontinence Questionnaire for vaginal symptoms (ICIQ-VS), to determine their POP symptoms. Data were analysed as numbers (raw data) and percentages of responders. Statistical comparisons were made using Chi-squared and Kruskal–Wallis tests as appropriate.
Results
Questionnaires were mailed to 3,412 women, 1,832 completed questionnaires were received (response 53.7 %). Symptoms strongly associated with prolapse; vaginal bulge/lump and bulge or lump outside of the vagina had a prevalence of 8.4 % and 4.9 % respectively. Vaginal symptoms, previous pelvic floor surgery, and age were statistically increased in those who had had a previous vaginal delivery. There were statistically worse scores (more symptoms) for the group with any vaginal delivery with regard to “feeling a loose or lax vagina”, “a vaginal lump or bulge coming down in the vagina”. There was a high prevalence of worry regarding sexual function, regardless of delivery status, with no statistically significant differences found between those who had had a vaginal delivery and those who had not. The group with no vaginal deliveries described a statistically significant increase in the reported sensation of “do you feel your vagina is too tight”.
Conclusions
Symptoms of POP were increased in those women who had experienced a vaginal delivery, whilst the sensation of having a tight vagina was decreased in those who had had a previous vaginal birth.
Similar content being viewed by others
References
Hagen S, Stark D (2011) Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev 7(12):CD003882. doi:10.1002/14651858.CD003882.pub4
Samuelsson EC, Arne Victor FT, Tibblin G, Svärdsudd KF (1999) Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol 180(2):299–305. doi:10.1016/S0002-9378(99)70203-6
Glazener C, Elders A, MacArthur C, Lancashire R, Herbison P, Hagen S, Dean N, Bain C, Toozs-Hobson P, Richardson K, McDonald A, McPherson G, Wilson D (2013) Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG 120(2):161–168
Barber M, Maher C (2013) Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J 24(11):1783–1790. doi:10.1007/s00192-013-2169-9
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–506
Jha S (2011) Uterovaginal prolapse. In: Arulkumaran S, Regan L, Papageorghiou A, Monga A, Farquharson D (eds) Oxford desk reference: obstetrics and gynaecology. Oxford University Press, Oxford, pp 626–628
FDA (2011) Urogynecologic surgical mesh: update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. FDA, http://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM262760.pdf
Pradhan A, Tincello D, Kearney R (2013) Childbirth after pelvic floor surgery: analysis of hospital episode statistics in England, 2002–2008. BJOG 120(2):200–204
Cuicchi D, Lombardi R, Cariani S, Leuratti L, Lecce F, Cola B (2013) Are there changes in symptoms of pelvic floor disorders after bariatric surgery? Surg Obes Relat Dis 9(1):69–71
Gyhagen M, Bullarbo M, Nielson TF, Milsom I (2013) Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120(2):152–160
Digesu GA, Khullar V, Cardozo L, Robinson D, Salvatore S (2005) P-QOL: a validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int Urogynecol J 16(3):176–181. doi:10.1007/s00192-004-1225-x
Slieker-ten Hove MP, Pool-Goudzwaard A, Eijkemans MC, Steegers-Theunissen RM, Burger C, Vierhout M (2009) The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int Urogynecol J 20(9):1037–1045. doi:10.1007/s00192-009-0902-1
Tegerstedt G, Maehle-Schmidt M, Nyrén O, Hammarström M (2005) Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Int Urogynecol J 16(6):497–503. doi:10.1007/s00192-005-1326-1
Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL (2007) Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol 109(6):1396–1403
MacLennan AH, Taylor AW, Wilson DH, Wilson D (2000) The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG 107:1460–1470
Doaee M, Moradi-Lakeh M, Nourmohammadi A, Razavi-Ratki SK, Nojomi M (2014) Management of pelvic organ prolapse and quality of life: a systematic review and meta-analysis. Int Urogynecol J 25(2):153–163. doi:10.1007/s00192-013-2141-8
Price N, Jackson SR, Avery K, Brookes ST, Abrams P (2006) Development and psychometric evaluation of the ICIQ vaginal symptoms questionnaire: the ICIQ-VS. BJOG 113(6):700–712
Barber MD, Neubauer NL, Klein-Olarte V (2006) Can we screen for pelvic organ prolapse without a physical examination in epidemiologic studies? Am J Obstet Gynecol 195(4):942–948. doi:10.1016/j.ajog.2006.02.050
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE (2001) Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol 185(6):1332–1337. doi:10.1067/mob.2001.119078, discussion 1337-1338
Swift S, Woodman P, O’Boyle A, Kahn M, Valley M, Bland D, Wang W, Schaffer J (2005) Pelvic organ support study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol 192(3):795–806. doi:10.1016/j.ajog.2004.10.602
Bowling A (2005) Mode of questionnaire administration can have serious effects on data quality. J Public Health 27:281–291
Hunskaar S, Lose G, Sykes D, Voss S (2004) The prevalence of urinary incontinence in women in four European countries. BJU Int 93:324–330
Perry S, Shaw C, Assassa P, Dallosso H, Williams K, Brittain KR, Mensah F, Smith N, Clarke M, Jagger C, Mayne C, Castleden CM, Jones J, McGrother CW (2000) An epidemiological study to establish prevalence of urinary symptoms and felt need in the community: The Leicestershire MRC incontinence study. J Public Health Med 22:427–434
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kapp Z, Herschorn S, Coyne K, Kelleher C, Hampel C, Artibani W, Abrams P (2006) Population based survey on urinary incontinence, overactive bladder and other lower urinary tract symptoms in five countries. Results of the EPIC study. Eur Urol 50:1306–1315
Mant J, Painter R, Vessey M (1997) Epidemiology of genital prolapse: observations from the oxford family planning association study. BJOG: Int J Obstet Gynaecol 104(5):579–585. doi:10.1111/j.1471-0528.1997.tb11536.x
Dua A, Radley S, Brown S, Jha S, Jones G (2012) The effect of posterior colporrhaphy on anorectal function. Int Urogynecol J 23(6):749–753. doi:10.1007/s00192-011-1603-0
Bondili A, Deguara C, Cooper J (2012) Medium term effects of a monofilament polypropylene mesh for pelvic organ prolapse and sexual function symptoms. J Obstet Gynaecol 32:285–290
Cooper J, Bondili A, Dequara C, Siraj N (2013) Vaginal repair with polypropylene mesh compared to traditional colporrhaphy for pelvic organ prolapse: medium-term follow Up. J Gynecol Surg 29(1):1–6. doi:10.1089/gyn.2012.0073
D’Hoore A, Penninckx F (2003) Obstructed defecation. Colorectal Dis 5:280–287. doi:10.1046/j.1463-1313.2003.00497.x
Funding
This study was funded by the principal author through a Keele University Research Account.
Conflicts of interest
J. Cooper has received lecture fees from Astellas. None of the other authors has any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cooper, J., Annappa, M., Dracocardos, D. et al. Prevalence of genital prolapse symptoms in primary care: a cross-sectional survey. Int Urogynecol J 26, 505–510 (2015). https://doi.org/10.1007/s00192-014-2556-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2556-x