Abstract
Purpose
To evaluate the effectiveness of peer-delivered interventions in improving clinical and psychosocial outcomes among individuals with severe mental illness (SMI) or depression.
Methods
Systematic review and meta-analysis of randomised controlled trials comparing a peer-delivered intervention to treatment as usual or treatment delivered by a health professional. Random effect meta-analyses were performed separately for SMI and depression interventions.
Results
Fourteen studies (10 SMI studies, 4 depression studies), all from high-income countries, met the inclusion criteria. For SMI, evidence from three high-quality superiority trials showed small positive effects favouring peer-delivered interventions for quality of life (SMD 0.24, 95 % CI 0.08–0.40, p = 0.003, I 2 = 0 %, n = 639) and hope (SMD 0.24, 95 % CI 0.02–0.46, p = 0.03, I 2 = 65 %, n = 967). Results of two SMI equivalence trials indicated that peers may be equivalent to health professionals in improving clinical symptoms (SMD −0.14, 95 % CI −0.57 to 0.29, p = 0.51, I 2 = 0 %, n = 84) and quality of life (SMD −0.11, 95 % CI −0.42 to 0.20, p = 0.56, I 2 = 0 %, n = 164). No effect of peer-delivered interventions for depression was observed on any outcome.
Conclusions
The limited evidence base suggests that peers may have a small additional impact on patient’s outcomes, in comparison to standard psychiatric care in high-income settings. Future research should explore the use and applicability of peer-delivered interventions in resource poor settings where standard care is likely to be of lower quality and coverage. The positive findings of equivalence trials demand further research in this area to consolidate the relative value of peer-delivered vs. professional-delivered interventions.
Similar content being viewed by others
Introduction
Persons with a history of mental illness have been utilised as providers of conventional mental health services in a variety of high-income countries [1–3]. In this capacity, they are called peer health workers. Peers have been defined only vaguely in the literature and their definition often overlaps with those of volunteers or paraprofessionals. However, what distinguishes peers from other lay health providers is that their knowledge is not derived from formal training, but from personal experience [4, 5]. Peers may also share socio-demographic characteristics with the service users they work with and may be matched with the patient by family background, community, age, gender or ethnicity [4, 6].
Due to their experiential knowledge of mental illness [5], persons with a history of mental disorders are thought to relate particularly well with the service user and may be a useful resource to facilitate patient recovery. Peers can act as role-models and may restore hope by positive self-disclosure [1]. As a result, peers have been called upon to perform a variety of tasks including provision of social support and befriending, case management, disease self-management, counselling, outreach, coaching and advocacy [2]. Peers may provide different types of support strategies including emotional support, support based on appraisal (providing feedback on illness self-management or lifestyle) or providing general information about the disease [4, 7]. Peer support is distinct from support received by self-help groups. Davidson et al. [8] conceptualised peer support as an asymmetric, one-directional relationship. This differs from the support received in self-help groups as this format encourages reciprocal support in which all members of the group share problems and experiences [8].
To date three reviews on the evidence of peer support in mental health have been published, one meta-analysis [2] and two qualitative syntheses including non-randomised studies [2, 9]. Pitt et al. [2] included 11 RCTs in their systematic review and focused on outcomes for service provision such as client satisfaction and use of services. Clinical and psychosocial outcomes were also reported, however, only two trials were included which assessed the effect of consumer-providers on clinical outcomes, and two trials on quality of life. Of these four studies, two are included in our review, the other two studies were not compatible with our inclusion criteria. Simpson et al. [3] reviewed the evidence on the involvement of users in mental health services. Authors included three RCTs on the use of current users of mental health services as service providers (one of which is included in our review). Repper and Cater [9] summarised the evidence of peer support in mental health services between 1995 and 2000. One RCT used by Repper and Cater met the inclusion criteria for our review. The remaining six RCTs were not considered, as different outcome measures were reported in these trials.
The aims of this systematic review and meta-analysis are threefold: (1) to synthesise the global evidence of peer-delivered interventions on clinical and psychosocial outcomes among individuals with severe mental illness (SMI) or depression (2) to update earlier reviews on that topic, and (3) to provide further guidance for future research on peer-delivered interventions.
Methods
We developed this systematic review in line with the PRISMA statement for reporting systematic reviews and report the methods and findings according to its checklist [10]. The review was guided by a review protocol developed by all authors (available upon request).
Identification of studies and search strategy
Study inclusion and exclusion criteria are listed in online data supplement I. Included studies were randomised controlled trials (RCTs) which compared the effectiveness of a peer-delivered intervention on service users’ mental health outcomes to treatment as usual (TAU; superiority trials) or to treatment delivered by a professional health worker (equivalence trials). Superiority trials (trials in which the experimental arm was peer delivery in addition to TAU compared to TAU only) as well as equivalence trials (trials which compared the peer-delivered intervention to the same treatment delivered by a health professional) were eligible for inclusion. Service users were adults diagnosed with a mental disorder classified according to ICD-10 or DSM-IV criteria. Peers were defined as non-professional health workers who possess knowledge of a disease or a specific stressor from personal experience rather than formal training and who may share salient target population similarities such as gender or age with the recipient [6]. Interventions were included which placed service users in direct contact with at least one peer who provided a conventional service in an intentional, one-directional relationship [8]. RCTs were eligible for inclusion if service users’ clinical (e.g. change in symptoms) or psychosocial outcomes (e.g. quality of life, social functioning, hope and loneliness) were assessed using a validated quantitative measure.
The search strategy was developed in collaboration with an information scientist (see online data supplement II). The search was not limited by language, mental disorder or study design. The following databases were searched: Medline (1946 to Dec 2012), Embase (1980 to Dec 2012), PsycINFO (1806 to Dec 2012), Global Health (1910 to Dec 2012), CINAHL (1937 to Dec 2012), Social Science Citation Index (1970 to Dec 2012), Sociofile (1963 to Dec 2012) and Cochrane Libraries (CDSR, DARE, CENTRAL). In addition, bibliographies of eligible papers were reviewed and authors of included studies contacted to identify further relevant studies.
The literature search was conducted by DF who initially screened all titles and abstracts for studies not related to mental disorders. The remaining papers were double screened by two authors (DF, TS) who selected papers for full text screening. The same authors determined the eligibility of full text papers according to the inclusion and exclusion criteria outlined above. In cases of disagreement, a third author (MDS) was consulted and a decision agreed. Data from eligible papers were double extracted by three authors (DF, TS, NA) using a standard data extraction form specifically developed for the review. Data regarding study characteristics (e.g. study participants, peers and their training/supervision, intervention and mode of intervention delivery) as well as details of the intervention and control group, outcome measures, effect estimates and methodological quality of studies were extracted (extended summary of findings table is included in online data supplement III). The methodological quality of studies was independently assessed by three authors (DF, TS, NA) using the Cochrane Risk of Bias tool [11]. Risk of bias was assessed both at the study (e.g. allocation concealment) and outcome level (e.g. loss of follow-up). Authors of eligible papers were contacted for relevant unreported data and clarification where data were reported in an ambiguous manner.
Statistical analysis
Review Manager 5 [12] was used to perform statistical analyses. Post-treatment means and standard deviations (SDs) of the experimental and control group were extracted separately for SMI and depression for clinical (change in symptoms) and psychosocial outcomes which were reported in studies (for SMI: quality of life, social functioning and hope/self-esteem; for depression: loneliness). Hope and self-esteem were grouped together as self-esteem can be thought as sub-construct of hope, helping patients believing that they can reach a desired goal using their own abilities and skills [13]. In addition to post-treatment means and SDs, the sample size of the experimental and control group was extracted to calculate the standardised mean difference (SMD) for each RCT. Random effects analyses were performed separately for SMI and depression, and separately for clinical and psychosocial outcomes. This was done to assess whether peer-delivered interventions would have different effects on the two types of disorders and outcomes. To interpret SMDs, we referred to Cohen et al. [14, 15] who recommend that 0.2 represents a small effect, 0.5 a moderate effect and 0.8 a large effect. Heterogeneity was assessed using the I 2 statistic.
Clinical scales were multiplied by −1 to ensure that clinical and psychosocial scales point in the same direction (i.e. all clinical scales which were used in the trials increased in symptom severity whereas all psychosocial scales decreased in symptom severity). This was done to harmonise differences and interpretation of scales among outcomes across the trials. Data from cluster RCTs [16] were combined with data of individual RCTs if cluster RCTs adjusted for clustering at the analytical level [17].
For our main analyses, we considered the effect of peer-delivered interventions for high-quality trials only. Trials that had a risk of bias for allocation concealment, a risk of bias for sequence generation/and or masking of outcome assessment were excluded. In addition, a series of sensitivity analyses was conducted. Firstly, all superiority trials were separately investigated from equivalence trials. Secondly, we investigated the effect of peer-delivered interventions on clinical and psychosocial outcomes irrespective of study quality. Thirdly, the effect of individual peer-delivered interventions (i.e. one-to-one interventions) and group interventions (i.e. peer delivering the intervention to more than one person) on clinical and psychosocial outcomes for SMI and depression were assessed. Fourthly, we investigated the effect of short- and long-term follow-up to explore if the effect of peer-delivered interventions changes over time. Short-term follow-up was defined as follow-up of less than 6 months, and long-term follow-up of more than 6 months. This breakdown was chosen as one group of trials had a follow-up time of 3–6 months, whilst another group of trials had a follow-up time of 6–9 months and beyond (12 months maximum).
Funnel plots were generated for the main analyses to assess publication bias. This was done separately for SMI and depression outcomes. We performed a visual inspection of funnel plots instead of performing a statistical test of asymmetry as numbers of trials were limited and heterogeneity between trials was large [15, 18].
Results
Effect of peer-delivered interventions on severe mental illness
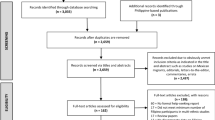
The electronic database search identified 10,799 potentially relevant studies. Fourteen studies met the eligibility criteria and were included in the review. Selection of studies is presented in Fig. 1. Ten studies included service users with a diagnosis of SMI [16, 19–27]. The remaining four studies evaluated the effect of peer-delivered interventions on service users with a diagnosis of depression [7, 28–30]. SMI trials included service users with psychosis or comorbid psychosis. Thirteen trials were individual RCTs, whilst one was a cluster RCT. The majority of trials were superiority trials, and there were two SMI equivalence trials. All included studies were conducted in high-income settings. Nine trials were from the US, four from Canada, and one from the Netherlands. All studies were published in English language journals. Summary of findings is presented in Table 1 with a more comprehensive summary of findings table being included in online data supplement III.
Superiority trials
Of the 8 superiority SMI trials, three were group interventions in which group size ranged from 4 to 13 service users. All group interventions were manual-based recovery and disease self-management interventions in which peers provided psycho-education, social support, information about the disease and taught strategies to overcome disease-specific problems in weekly sessions. There were five individual interventions in which the peer provided intensive case management to one service user over a period of several months. Individual interventions were primarily based on provision of support and befriending. None of the peer-delivered SMI interventions had an active psychotherapeutic ingredient such as cognitive behaviour therapy.
Five superiority SMI trials reported long-term outcomes (e.g. ≥6 month follow-up), and three trials reported a short-term follow-up time of 6 months and less. Clinical outcomes such as change in psychiatric symptoms as well as psychosocial outcomes such as quality of life, social functioning and hope were reported across all SMI trials. Five out of the eight trials had an overall high risk of bias.
All superiority trials took place in the community. Peers were persons with a history of mental illness or persons in recovery who received training and regular supervision from clinical coordinators or project staff during intervention delivery. TAU provided in the control group consisted of comprehensive outpatient community mental health care which was delivered by a range of community-based agents such as general practitioners and community health nurses.
Figure 2 shows the primary analyses for high-quality SMI superiority trials only. Excluding low quality of life trials led to a small positive effect favouring peer-delivered interventions (SMD 0.24, 95 % CI 0.08–0.40, p = 0.003, I 2 = 0 %, n = 639). Excluding hope trials with an overall high risk of bias led to a small positive effect for peer-delivered interventions as well (SMD 0.24, 95 % CI 0.02–0.46, p = 0.03, I 2 = 65 %, n = 967). No effect on clinical outcomes could be observed.
In addition, we assessed the effect of peer-delivered interventions on clinical outcomes, quality of life, social functioning and hope irrespective of study quality. There was no effect on any of these outcomes in this kind of analysis (Fig. 1.1, online data supplement IV). Sensitivity analyses for clinical outcomes and social functioning conducted separately for delivery type and length of follow-up did not impact this result. Further sensitivity analyses for quality of life indicated a small appreciable benefit favouring individual peer-delivered interventions (SMD 0.24, 95 % CI 0.08–0.40, p = 0.003, I 2 = 0 %, n = 639) of short-term follow-up (Figs. 1.4 and 1.5, online data supplement IV). Similarly, for hope, sensitivity analyses showed a positive effect favouring individual peer-delivered interventions which had a short-term follow-up time as well (SMD 0.24, 95 % CI 0.02–0.46, p = 0.03, I 2 = 65 %, n = 967; Fig. 1.6, online data supplement IV).
Equivalence trials
Of the two SMI equivalence trials, one was a group-based disease self-management programme delivered by a peer in six weekly sessions. There were eight service users in one group who met over a duration of 6 months. The other equivalence trial consisted of individual case management and was based on an assertive community treatment model provided by a peer over 12 months. Both trials took place in the community and measured quality of life as well as clinical outcomes. Both trials were of good methodological quality. Participants in the experimental arm received the peer-delivered intervention only. The control group received either the same intervention or standard psychiatric care provided by a psychiatrist.
The forest plot for the two equivalence trials is presented in Fig. 3. Results for clinical symptoms or quality of life were not significant between the groups, indicating the equivalence of peer-delivered and professional-delivered interventions.
Effect of peer-delivered interventions on depression
Four superiority trials assessed the effect of peer-delivered interventions on depression. Two outcomes were measured across the depression trials: change in psychiatric symptoms and loneliness. The trials consisted of one group intervention and three individual interventions. The group intervention consisted of a structured disease self-management programme. Individual interventions were based on provision of informational, emotional, affirmational and practical support by a peer. One trial had a follow-up time of 12 months, the other two trials of less than 6 months. Out of the four depression trials, one had an overall high risk of bias.
All depression trials took place in the community. Peers attended a training workshop before intervention delivery and received ongoing supervision through the entire period of the trials. TAU consisted of standard community care provided by public health nurses, physicians and other providers.
There was no effect of peer-delivered interventions on clinical outcomes (SMD −0.12, 95 % CI −0.56 to 0.32, p = 0.60, I 2 = 68 %, n = 695) or loneliness (SMD 0.27, 95 % CI −0.19 to 0.72, p = 0.25, I 2 = 57 %, n = 641) (Fig. 2.1, online data supplement IV.). Excluding one study with low quality or investigating the effect of individual vs. group interventions and short-term vs. long-term follow-up did not change the effect size or precision of estimate (see Fig. 2, online data supplement IV).
Publication bias
Funnel plots were largely symmetrical, although the funnel plot for the main SMI meta-analyses had three outliers. Asymmetry may have caused the large heterogeneity between studies and/or by the poor methodological quality of studies [15, 17]. Funnel plots are available online in data supplement V.
Discussion
Main findings
Peers have the potential to deliver care to persons with SMI and seem to positively influence patient’s clinical and psychosocial outcomes. Analysing high-quality superiority trials for SMI led to a small effect of peer-delivered interventions on quality of life and hope. There are some signs that interventions which are delivered in an individual format seem to work better than group interventions. This effect seems to level over the long term and does not seem to be sustainable beyond 6 months. Our results indicate that there is equivalence in clinical and psychosocial outcomes regardless of whether the intervention is delivered by a peer or professional. However, these results may not be generalisable due to the small number of studies included in the analysis.
For depression, no effect of peer-delivered interventions on improvements in clinical and psychosocial outcomes was found. Investigation of individual vs. group interventions, short- vs. long-term follow-up and the exclusion of low-quality studies did not change this result. For both depression and SMI, there is no evidence that peers negatively affect clinical or psychosocial outcomes of patients.
Our findings are in line with those of previous reviews. Pitt et al. [2] found no difference in clinical outcomes and quality of life between service users participating in peer-delivered interventions and patients in the control group in equivalence trials. For superiority trials, no data were presented for clinical outcomes or quality of life. In their qualitative synthesis, Simpson and House [3] concluded that employing service users in the mental health system has no negative effect on client’s symptoms, and can lead to improvement in service user quality of life [3]. Similarly, Repper and Cater [9] reported that peer-delivered interventions can lead to an increase in service users’ hope and prospects for the future. All findings of these reviews were based on a low number of studies.
Strengths and methodological limitations of the review
There are a few methodological limitations hampering the strength of evidence for this systematic review. Although peer support is widely used in high-income countries [1–3, 8, 9, 31], there are still few good quality trials evaluating the effectiveness of peer-delivered interventions. The evidence base is, therefore, limited as five out of the eight superiority SMI trials and one of the four depression trials had an overall high risk of bias. Similarly, our positive finding on equivalence trials is based on two studies which pose serious implications for generalisability.
In addition, the number of trial participants was low in some cases resulting in wide confidence intervals which affected certainty of the effect estimate. On the other hand, a thorough literature review was conducted resulting in a number of studies which were not included in earlier reviews on this topic. Meta-analyses were performed separately for SMI and depression, and separately for clinical and psychosocial outcomes. Sensitivity analyses were conducted to control for mode of intervention delivery, length of follow-up and study quality.
Limitations in the strength of evidence and interpretation of findings
Evidence from three high-quality superiority trials showed small positive effects favouring peer-delivered interventions for quality of life and hope. However, for the majority of SMI and depression studies no effect of peer-delivered interventions could be found. This might be due to the low methodological quality of studies or the type of care which was delivered in the control group. In all superiority SMI and depression trials comprehensive outpatient community mental health care was provided in the control arm. As a result, in some cases, participants in the control group might have even received more social support than what was currently available in the community [30]. Thus, we may observe the lack of effect of peer interventions to add more benefit to an already comprehensive, person-centred care model.
There are some other interesting aspects shedding light on the current evidence of superiority peer trials. One was provided by Letourneau et al. [30] which is linked to the argument provided above. Letourneau et al. [30] reported that the perception of support in their depression trial’s control group was considerable. Authors speculated that it was the overall perception of support which had a stronger influence on patient outcomes than the support which was actually provided [7, 30]. This assumption stems from earlier work of Wethington and Kessler [32] who showed that the hypothetical resource availability provided by a group of people had a greater impact on adjustments to stressful life events than the actual measured support which was received. Also, peer interventions might not always be successful as a functional dyad between a peer and a patient may depend on personal characteristics of the two parties and therapeutic relationships may not have always been properly developed in some trials [7, 23, 30]. In one study for example, dropping peer sessions became a common habit among patients possibly due to internalised stigma [23]. However, this finding was reported in one trial only, and there is no further evidence that patients did not adhere to the intervention.
Implications for future research
There are several implications for future research. Firstly, it would greatly enhance the evidence on peer-delivered interventions if more equivalence trials were conducted in high-income countries (i.e. trials which compare for example a counselling intervention delivered by a peer with counselling delivered by a health professional without enhancing it by TAU) as we are still uncertain about the relative value of peer interventions vs. professional interventions. Such trials should include a strong economic evaluation to assess the possibility of equivalence at a lower cost. Clearly, such comparisons must pay close attention to the risks of harm.
Secondly, peer-delivered interventions identified for this review were all primarily support based, and none used peers in the role of co-therapists for the delivery of any kind of evidence-based psychotherapeutic treatment. Future research should explore the use of peers as co-therapists and report on the effectiveness of peers as providers of evidence-based psychological treatments.
Thirdly, generalisability is limited. The majority of studies were conducted in the USA and results are, therefore, only applicable to high-income countries. There is a need to test the effectiveness of peer-delivered interventions with a superiority trial in low resource settings where specialist human resources are limited and mental health care systems fragmented. These kinds of trials can then also inform the evidence base of superiority peer trials conducted in high-income settings. Moreover, utilising peers could provide an essential driver in low-income settings relieving the scarcity of human capital through task sharing. This is supported by evidence from low- and middle-income countries in which peers have shown to be effective providers of health care, facilitating mother and child programmes or care for non-communicable diseases and HIV/AIDS. In Nepal and India, for example, a community-based participatory intervention led by a peer significantly reduced neonatal mortality rates [33, 34] and improved depressive symptoms of mothers by 57 % over the duration of the trial [33]. Similarly, in Bangladesh and Uganda, a community-based peer counsellor significantly improved initiation and duration of exclusive breastfeeding practises among mothers [35], and helped mothers to identify and overcome common breastfeeding problems [36]. In Shanghai, a peer-led diabetes self-management programme which was implemented in rural communities effectively increased the duration of aerobic exercise among patients in the intervention group, and led to significant improvements of patient’s self-efficacy as well as their systolic blood pressure [37]. Peer education interventions for HIV prevention in low- and middle-income countries significantly reduced equipment sharing among injecting drug users and increased condom use [38]. These examples show that peer interventions in low- and middle-income countries in which health systems are under-resourced show promise and there is a need to examine their impact in the context of global mental health.
Fourth, as many trials had an overall high risk of bias and were poorly reported, there is a need for trials of peer-delivered interventions to systematically follow the CONSORT statement [39] for social and psychological interventions to improve quality of reporting for RCTs [40] so that the quality of the evidence can be improved. Inadequate reporting of peer trials might lead to biassed conclusions and biassed treatment effects [39].
Conclusion
This systematic review and meta-analysis synthesised the current evidence on the effectiveness of peer-delivered interventions on clinical and psychosocial outcomes for persons with SMI and depression. There is weak evidence that peers can have a positive impact on clinical and psychosocial outcomes in patients with SMI. However, we need more high-quality evidence from high-income countries, in particular equivalence trials and trials of peer-delivered evidence-based psychological treatments. Peers are still an untapped resource in global mental health and there is a need to explore the acceptability and effectiveness of peer-delivered mental health interventions in low- and middle-income countries as well. This may potentially introduce another type of human resource to address the great shortage of mental health care providers in the global context.
References
Davidson L et al (2012) Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry 11(2):123–128
Pitt V et al (2013) Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev 3:Cd004807
Simpson EL, House AO (2002) Involving users in the delivery and evaluation of mental health services: systematic review. BMJ 325(7375):1265
Dennis CL (2003) Peer support within a health care context: a concept analysis. Int J Nurs Stud 40(3):321–332
Borkman T (1976) Experiental knowledge: a new concept for the analysis of self-help groups. Social Service Rev 50:445–456
Giblin PT (1989) Effective utilisation and evaluation of indigenous health care workers. Public Health Rep 104:361–368
Dennis CL (2003) The effect of peer support on postpartum depression: a pilot randomized controlled trial. Can J Psychiatry 48(2):115–124
Davidson L et al (2006) Peer support among adults with serious mental illness: a report from the field. Schizophr Bull 32(3):443–450
Repper J, Carter T (2011) A review of the literature on peer support in mental health services. J Ment Health 20(4):392–411
Liberati A et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions, Version 5.1.0: The Cochrane Collaboration
Review Manager (RevMan) (2012) The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen
Weis R, Speridakos EC (2011) A meta-analysis of hope enhancement strategies in clinical and community settings. Psychol Well-Being Theory Res Pract 1(5). doi:10.1186/2211-1522-1-5
Cohen J (1988) Statistical power analysis in the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates, Mahwah
De Silva MJ et al (2013) Effect of psychosocial interventions on social functioning in depression and schizophrenia: meta-analysis. Br J Psychiatry 202(4):253–260
Forchuk C et al (2005) Therapeutic relationships: from psychiatric hospital to community. J Psychiatr Ment Health Nurs 12:556–564
Gates S (2005) Methodological guidelines, In: T.E.t.P.a.C. Group (ed) About the Cochrane Collaboration (Collaborative Review Groups)
Sterne JAC, Harbord RM (2004) Funnel plots in meta-analysis. Stata J 4:127–141
Cook JA et al (2012) Results of a randomized controlled trial of mental illness self-management using Wellness Recovery Action Planning. Schizophr Bull 38(4):881–891
Cook JA et al (2012) Randomized controlled trial of peer-led recovery education using Building Recovery of Individual Dreams and Goals through Education and Support (BRIDGES). Schizophr Res 136(1–3):36–42
Druss BG et al (2010) The Health and Recovery Peer (HARP) Program: a peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophr Res 118:264–270
van Gestel-Timmermans H et al (2012) Effects of a peer-run course on recovery from serious mental illness: a randomized controlled trial. Psychiatr Serv 63(1):54–60
Davidson L, Shahar G, Strayner DA (2004) Supported socialization for people with psychiatric disabilities: lessons from a randomized controlled trial. J Community Psychol 32(4):453–477
Greenfield TK et al (2008) A randomized trial of a mental health consumer-managed alternative to civil commitment for acute psychiatric crisis. Am J Community Psychol 42(1–2):135–144
Rivera JJ, Sullivan AM, Valenti SS (2007) Adding consumer-providers to intensive case management: does it improve outcome? Psychiatr Serv 58(6):802–809
Sells D et al (2008) Beyond generic support: incidence and impact of invalidation in peer services for clients with severe mental illness. Psychiatri serv (Washington, D.C.) 59:1322–1327. doi:10.1176/appi.ps.59.11.1322
Solomon P, Draine J (1995) One-year outcomes of a randomized trial of consumer case management. Eval Program Plan 18(2):117–127
Ludman EJ et al (2007) A pilot study of telephone care management and structured disease self-management groups for chronic depression. Psychiatr Serv 58(8):1065–1072
Dennis CL et al (2009) Effect of peer support on prevention of postnatal depression among high risk women: multisite randomised controlled trial. BMJ 338:a3064
Letourneau N et al (2011) Effect of home-based peer support on maternal-infant interactions among women with postpartum depression: a randomized, controlled trial. Int J Ment Health Nurs 20(5):345–357
Davidson L et al (1999) Peer support among individuals with severe mental illness: a review of the evidence. Clin Psychol Sci Pract 6(2):165–187
Wethington E, Kessler RC (1986) Perceived support, received support, and adjustment to stressful life events. J Health Soc Behav 27(1):78–89
Tripathy P et al (2010) Effect of a participatory intervention with women’s groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet 375(9721):1182–1192
Manandhar DS et al (2004) Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet 364(9438):970–979
Haider R et al (2000) Effect of community-based peer counsellors on exclusive breastfeeding practices in Dhaka, Bangladesh: a randomised controlled trial [see comments]. Lancet 356(9242):1643–1647
Nankundu J et al (2006) Community based peer counsellors for support of exclusive breastfeeding: experiences from rural Uganda. Int Breastfeed J 1:19
Liu S et al (2012) Effectiveness of using group visit model to support diabetes patient self-management in rural communities of Shanghai: a randomized controlled trial. BMC Public Health 12:1043
Medley A et al (2009) Effectiveness of peer education interventions for HIV prevention in developing countries: a systematic review and meta-analysis. AIDS Educ Prev 21(3):181–206
Altman DG et al (2001) The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 134(8):663–694
Montgomery P et al (2013) Developing a Reporting Guideline for Social and Psychological Intervention Trials. Am J Public Health 103(10):1741–1746
Acknowledgments
We are grateful to information scientist Jane Falconer for her help in designing the search strategy. Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under award number 1U19MH095687-01. Daniela Fuhr is funded by the National Institute of Mental Health. Tatiana Taylor Salisbury is partly funded by the MRC and Department for International Development, Mary De Silva is funded by an LSHTM/Wellcome Trust Fellowship, Nadja van Ginneken by a Wellcome Trust clinical PhD fellowship, and Vikram Patel by a Wellcome Trust Senior Research Fellowship in Clinical Science. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fuhr, D.C., Salisbury, T.T., De Silva, M.J. et al. Effectiveness of peer-delivered interventions for severe mental illness and depression on clinical and psychosocial outcomes: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol 49, 1691–1702 (2014). https://doi.org/10.1007/s00127-014-0857-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-014-0857-5