Abstract
Multiple sclerosis (MS) is a life-long, potentially debilitating disease of the central nervous system (CNS). MS is considered to be an immune-mediated disease, and the presence of autoreactive peripheral lymphocytes in CNS compartments is believed to be critical in the process of demyelination and tissue damage in MS. Although MS is not currently a curable disease, several disease-modifying therapies (DMTs) are now available, or are in development. These DMTs are all thought to primarily suppress autoimmune activity within the CNS. Each therapy has its own mechanism of action (MoA) and, as a consequence, each has a different efficacy and safety profile. Neurologists can now select therapies on a more individual, patient-tailored basis, with the aim of maximizing potential for long-term efficacy without interruptions in treatment. The MoA and clinical profile of MS therapies are important considerations when making that choice or when switching therapies due to suboptimal disease response. This article therefore reviews the known and putative immunological MoAs alongside a summary of the clinical profile of therapies approved for relapsing forms of MS, and those in late-stage development, based on published data from pivotal randomized, controlled trials.
Similar content being viewed by others
Given that multiple sclerosis (MS) is a lifelong and, as yet, incurable disease, the long-term safety and tolerability profiles of treatments are clearly important considerations in therapy selection. |
There are now several disease-modifying therapies (DMTs) available, or in late-stage clinical development, for the treatment of relapsing forms of MS in the US and the European Union (EU). |
Each DMT has its own mechanisms of action and, as a consequence, each has a different efficacy and safety profile. Understanding the immunological mechanisms and associated clinical profiles of each therapy for MS is important, in order to select and manage patients’ therapy appropriately. |
Few comparative head-to-head trials have been undertaken to assess the superiority or non-inferiority of one therapy over another, and there is a need for such evidence now that numerous treatments for relapsing MS are available. |
There is a need for treatment algorithms to help physicians and their patients decide on a therapy for optimal disease management. |
1 Introduction
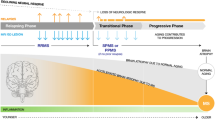
Multiple sclerosis (MS) is a chronic, inflammatory disease affecting the central nervous system (CNS) [1]. While the exact cause is unknown, extensive study of the pathology of MS has implicated autoimmune processes in disease progression. These are thought to be mediated by autoreactive lymphocytes that cross the blood–brain barrier (BBB) and enter the CNS where they cause localized inflammation resulting in demyelination, gliotic scarring, and axonal loss [2, 3]. According to this model, as the disease advances, and with repeated inflammatory episodes, CNS repair processes begin to fail, becoming less and less effective, and neurodegeneration results in progressive and irreversible disability [4].
An increased understanding of the pathophysiology of MS has allowed the development of new immunomodulating agents with unique mechanisms of action (MoA). The most effective drugs have tended to have the most profound effects on the immune system, which can result in treatment-limiting adverse events [5]. Clearly, it is important to weigh up the beneficial effects of specific drugs against the potential adverse events so that therapies can be prescribed in an informed manner and to the appropriate patients.
There are several disease-modifying therapies (DMTs) currently available, or in late-stage clinical development, for the treatment of relapsing forms of MS in the US and the European Union (EU). Interferon (IFN) β-1a and β-1b and glatiramer acetate (GA) administered by subcutaneous (SC) or intramuscular (IM) injection are the established first-line therapies for relapsing MS [6–15]. Natalizumab intravenous infusion has also been approved for nearly 10 years and is used mainly as a second-line therapy [16, 17]. Several oral drugs are also available. In 2010, fingolimod became the first oral drug to be approved for the treatment of relapsing forms of MS [18, 19]. More recently, oral teriflunomide [20] (2012) and dimethyl fumarate [21] (2013; US only) have also been approved. Alemtuzumab, administered as a course of infusions, was also recently approved within the EU [22] (2013). In addition, a number of experimental therapies are undergoing phase III clinical trials.
This paper reviews the MoA of the approved therapies and those in late-stage development for the treatment of relapsing MS (Table 1). The clinical efficacy of each therapy is also summarized, as well as the potential associated adverse effects and safety issues.
2 Parenteral Therapies
2.1 Interferon β-1a/b
2.1.1 Mechanism of Action and Immunological Effects
Type I IFNs are endogenous cytokines produced by eukaryotic cells in response to viral infections and related biological stimuli. Synthetic IFNs, synthesized via recombinant DNA technology in mammalian cells (known as IFNβ-1a) and via bacterial fermentation (known as IFNβ-1b), are used in the treatment of relapsing MS. The biological activity of IFN is mediated via interaction with specific cell surface receptors. Physiological and pathophysiological effects induced by IFNs are likely to reflect divergences in the downstream signaling induced by IFN type I-receptor binding and resulting pleiotropic transcriptional effects. As a result, the precise MoA of IFNs in MS is not yet understood. IFNs exert direct and indirect effects on lymphocytes, and may involve the expansion of immunomodulatory cells such as natural killer cells and T regulatory cells, inhibition of B-cell stimulatory capacity and secretion [23], and inhibition of the inflammasome [24]. IFNs also profoundly and directly influence CD8+ T-cell responses [25]. This T-cell subset predominates in MS lesions and is associated with permanent neurological deficits [26, 27].
It has been shown that IFNβ increases the production of anti-inflammatory cytokines and suppresses the production of proinflammatory cytokines. In an ex vivo study, the production of the anti-inflammatory cytokines interleukin (IL)-10 and IL-4 were enhanced significantly in the IFNβ-treated myelin basic protein-reactive T cells, while production of the proinflammatory cytokine, tumor necrosis factor (TNF)α, was unaffected [28]. Such preclinical data are supported by those from clinical studies. For example, in blood and cerebrospinal fluid (CSF) samples collected from patients with MS who were receiving treatment with IFNβ-1a, serum and CSF IL-10 levels increased with increasing treatment exposure [29]. Further studies showed that administration of IFNβ down-regulates expression of the proinflammatory cytokines IL-17 and osteopontin [30], and reduced serum IFNγ and TNFα in patients with MS, while increasing production of IL-10 [31].
The pharmacological actions of IFNβ described above have been attributed to its direct action on CD4+ T cells [30] and myeloid cells [32] through the type I IFN receptor, although IFNβ signaling with other cell types within the immune system is also thought to contribute to its therapeutic effects [33]. IFNβ is likely to have a limited direct effect on the CNS. The brain is relatively isolated from the immune system by the BBB, and it has not been established what doses of IFN would be needed to achieve physiologically relevant concentrations in CSF. It is possible that IFNs cross the BBB at sites of CNS inflammation. Alternatively, and not mutually exclusively, CNS effects of IFNs may be related to inhibition of inflammatory cell migration across the BBB [34].
2.1.2 Clinical Effects in Relapsing MS
Injectable IFNs have been the mainstay of MS treatment for around 20 years, and are frequently used as first-line therapy. Table 2 summarizes data regarding clinical efficacy (effect on disease relapses and disability progression) of the IFNβ formulations from randomized, placebo-controlled, phase III trials. The clinical efficacy in comparative randomized trials is summarized in Table 3. Meta-analyses show that IFNβ is associated with a significant effect on MS relapses and disability progression compared with placebo [38, 39]; however, the effect of IFNβ therapy on disability progression has been disputed, as a large-scale, retrospective study of prospectively collected data demonstrated that IFNβ was not associated with a reduction in disability progression [35–37]. A consideration relating to the efficacy of the IFNβ formulations is the potential for patients to produce neutralizing antibodies. Although the role of neutralizing antibodies is not fully understood, it is thought that they lead to treatment resistance and can therefore reduce treatment efficacy over the long term [38, 39].
All three forms of IFNβ are generally well tolerated. The most common adverse events are flu-like symptoms, headaches, and injection site reactions, as summarized in Table 4. However, due to the effect of IFNβ on circulating lymphocyte numbers, formulations are also associated with mild lymphopenia.
More recently, a formulation of IFNβ-1a conjugated to polyethylene glycol (PEG) was developed as a potential treatment for relapsing–remitting MS (RRMS). This pegylation process was designed to extend the half-life of IFNβ-1a and enable a less frequent dosing schedule. The ongoing phase III ADVANCE study (see Table 5 for full trial names) aims to determine the clinical efficacy of PEG-IFNβ-1a administered once every 2 weeks or every 4 weeks via SC injection in patients with relapsing MS [40].
2.2 Glatiramer Acetate
2.2.1 Mechanism of Action and Immunological Effects
GA was first approved as a daily injectable treatment for RRMS in 1996 and, like the IFNs, it is a frequently used first-line agent [10, 11]. More recently, a higher dose formulation (40 mg) administered three times per week has been approved in the US for use in patients with RRMS [41]. GA consists of a heterogeneous polypeptide mixture made of glutamic acid, lysine, alanine, and tyrosine that was designed to simulate myelin basic protein, one of the major myelin auto-antigens classically used to induce experimental autoimmune encephalomyelitis (EAE) in animal models, and also thought to be involved in MS.
The exact MoA of GA is not fully understood [42]; however, it appears to shift the GA-reactive lymphocyte population from a pro-inflammatory T helper (Th) 1 state to an anti-inflammatory Th2 state. In various studies, GA has also been shown to increase levels/expression of anti-inflammatory IL-10 and IL-4 cells, and decrease levels of proinflammatory TNF and IL-12 cells [23]. Daily usage appears to selectively promote trans-endothelial migration of Th2 cells across the BBB [43] and stimulate the release of anti-inflammatory cytokines [44]. There is no information regarding the absorption, distribution, metabolism, or excretion profiles of GA in humans as there is currently no direct and sensitive analytical method for measuring the compound in biological fluids. Therefore, it is also not known whether GA crosses the BBB.
A growing body of evidence suggests that GA leads to a broader immunomodulatory effect on cells of both the innate and adaptive immune system [23]. GA-mediated modulation of antigen-presenting cells (APCs) such as monocytes and dendritic cells, CD4+ Th cells, CD8+ T cells, Forkhead box P3+ regulatory T cells, natural killer cells, and antibody production by plasma cells have been reported [23]. In addition, most recent investigations indicate that GA treatment may also promote regulatory B-cell properties, with a reciprocal reduction in the expression of proinflammatory cytokines [45, 46]. T-cell-induced brain-derived neurotrophic factor (BDNF) secretion following GA administration has also been described in MS, EAE, and experimental cell lines [47]. However, the clinical implications of this are not fully understood.
2.2.2 Clinical Effects in Relapsing MS
The efficacy of GA in reducing relapses in patients with MS has been demonstrated in several randomized, controlled clinical trials (Tables 2, 3) and post hoc analyses [48]. The efficacy of GA on relapse reduction was similar to that of IFN therapy in the BECOME, BEYOND, and REGARD trials, with similar annualized relapse rates (ARRs) [49–51]. Combined GA and IFN therapy did not reduce the risk of relapse compared with GA therapy alone over 3 years in the CombiRX trial [52]. The most common adverse events associated with GA therapy are injection site reactions, vasodilation, and rash (summarized in Table 4). Following GA injection, an immediate systemic reaction can occur in some patients, leading to chest tightness, dyspnea, and bradycardia lasting up to 20 minutes, but this reaction is not considered to be life threatening [53]. Rates of discontinuation were similar to those for IFN formulations in clinical studies [49–51]. No new adverse events appeared in patients treated with a high-dose formulation of GA administered three times per week [41].
2.3 Mitoxantrone
2.3.1 Mechanism of Action and Immunological Effects
Mitoxantrone was approved in the US in 2000 for use in “patients with secondary progressive, progressive relapsing or worsening relapsing–remitting multiple sclerosis” [54]. It is a synthetic anthracenedione traditionally used as an anti-neoplastic agent. Mitoxantrone intercalates with the DNA of both proliferating and non-proliferating cells causing strand breaks, and also inhibits DNA repair via inhibition of topoisomerase II [55]. It is thought that the mechanism by which mitoxantrone exerts its therapeutic effect in MS is through inhibition of proliferation of B and T lymphocytes and macrophages [54]. Additionally, several other immunosuppressive effects have been described, such as decreased secretion of IFNγ, TNFα, and IL-2 [56].
2.3.2 Clinical Effects in Relapsing MS
Mitoxantrone is administered by intravenous infusion every 3 months at a dose that is body-weight dependent (12 mg/m2). Table 2 summarizes data regarding clinical efficacy on disease relapses and disability progression of mitoxantrone from the randomized, placebo-controlled, phase III MIMS trial [55]. Meta-analyses show that mitoxantrone is associated with a significant effect on MS relapses and disability progression compared with placebo [57].
The most common adverse events are nausea, vomiting, alopecia, and urinary tract infections, as summarized in Table 4 [54]. Cardiotoxicity, neutropenia, amenorrhea, which in some cases may be permanent, and the potential for late-occurring leukemia are the major safety concerns associated with mitoxantrone use [57].
2.4 Natalizumab
2.4.1 Mechanism of Action and Immunological Effects
Natalizumab is a recombinant humanized monoclonal antibody produced in murine myeloma cells [17]. Natalizumab is a selective adhesion molecule inhibitor; it binds specifically to α4-subunits of α4β1 and α4β7 integrins expressed on the surface of all white blood cells (WBCs), except neutrophils [58]. This inhibits α4-mediated adhesion of WBCs to their counter-receptors, including vascular cell adhesion molecule-1 (VCAM-1) [59], and reduces very late antigen-4 expression on all investigated immune cells, including B cells [60]. This produces a number of phenotypic changes in the immune composition of peripheral blood [61].
Natalizumab increases the percentage of activated leukocytes producing pro-inflammatory cytokines, which has been attributed to sequestration of activated lymphocytes in the peripheral circulation [62, 63]. The CD4/CD8 ratio is reduced with long-term therapy [64], and serum immunoglobulin (Ig) M and IgG levels decrease significantly with continued therapy [65]. Natalizumab also increases the number of circulating CD34+ hematopoietic progenitors by interfering with homing to bone marrow [66]. In addition, increases in peripheral natural killer cells have been observed with natalizumab treatment. This effect may play a role in its efficacy, but further investigation is required [23].
Through the disruption of various molecular interactions, natalizumab is believed to directly inhibit transmigration of leukocytes into the CNS and inflamed parenchymal tissue [59], thus reducing the formation of MS lesions. Treatment with natalizumab may also inhibit the ongoing inflammation mediated by leukocytes already present in the CNS by interrupting their interaction with the extracellular matrix proteins [67]. One study has shown that natalizumab can cross the BBB, although the full implications of this finding are yet to be determined [68].
2.4.2 Clinical Effects in Relapsing MS
Natalizumab intravenous infusion was approved as a treatment for RRMS in 2007, and is used mainly as a second-line therapy [16, 17]. The phase III, placebo-controlled AFFIRM study demonstrated the efficacy of natalizumab in reducing disease relapses and preventing disability progression [69], and subsequent meta-analyses confirmed these findings [70, 71]. At present, there are no direct head-to-head comparisons of natalizumab with other DMTs (Table 3), but the numerical differences in the findings seen in AFFIRM suggest this agent may be more effective than the IFNβs and GA in terms of reducing relapses (Table 2).
In a prospective, observational cohort study of 73 MS patients treated with natalizumab, development of antibodies to the agent occurred by week 24 in 58 % of the patients [72]. The majority of these patients reverted to an anti-natalizumab-negative status at follow-up. However, the persistence of anti-natalizumab antibodies in the minority of patients correlated with a reduction in serum natalizumab levels and decreased drug efficacy [72, 73].
The most common adverse events associated with natalizumab therapy are headache, fatigue, and respiratory tract infections (summarized in Table 4). The immune system effects of natalizumab may increase the risk of infections, including pneumonia, urinary tract infections, gastroenteritis, vaginal infections, tooth infections, tonsillitis, and herpes infections [17, 69].
Most notably, long-term exposure to natalizumab increases the risk of progressive multifocal leukoencephalopathy (PML), an opportunistic infection caused by the John Cunningham virus (JCV), which can reactivate in patients who are immunocompromised [74]. As of September 2013, over 120,500 patients worldwide had received natalizumab and, as of November 2013, there had been 418 confirmed post-marketing cases of PML among these individuals leading to 96 deaths (23 %) [75]. Risk factors for development of PML in natalizumab-treated MS patients include a positive anti-JCV antibody test, prior use of immunosuppressants, and exceeding 24 months of natalizumab treatment [76]. Presence of all three factors increases the risk of PML by about 20-fold compared with having a positive anti-JCV antibody test alone, and by over 100-fold compared with a negative test for JCV antibodies [77]. Given that anti-JCV antibodies are found in 50–60 % of the general population, healthcare providers are advised to stratify their patients to treatment according to anti-JCV status and other risk factors. Additionally, it is recommended that patients receiving natalizumab who test negative for anti-JCV antibodies should be retested every 6 months [76] as seroconversion rates are estimated to be between 2.0 % and 14.5 % per year [78, 79]. Immune reconstitution inflammatory syndrome after withdrawal of natalizumab has been observed in at least 90 % of patients with PML, leading to death in 29 % [17, 80, 81].
Due to the risk of infections following natalizumab therapy, it is suggested that a washout period may be required before switching from natalizumab to another immunomodulatory therapy [82]. The pharmacodynamic effects of natalizumab are reported to last for 12 weeks according to the European Summary of Product Characteristics, but some reports suggest that some effects may continue for as long as 6 months [83]. However, this must be balanced with the risk of severe relapse if treatment with the new agent is delayed for too long [78, 84–88]. Therefore, the optimal time to initiate a new therapy after natalizumab discontinuation requires further investigation, and should also be considered on an individual patient basis to maximize efficacy and reduce risk of disease relapse and residual natalizumab effects.
2.5 Alemtuzumab
2.5.1 Mechanism of Action and Immunological Effects
Alemtuzumab is a recombinant, DNA-derived, humanized monoclonal antibody that targets CD52, a cell surface protein predominantly found in B and T lymphocytes [89]. Alemtuzumab is administered by intravenous infusion once per year, and is currently approved for the treatment of B-cell chronic lymphocytic leukemia and has recently been approved in the EU as a therapy for RRMS [22]. Treatment with alemtuzumab results in a rapid and long-lasting depletion of lymphocyte populations, after which homeostatic reconstitution leads to alterations in cell subsets, causing long-lasting changes in adaptive immunity [90].
2.5.2 Clinical Effects in Relapsing MS
Results from two phase III trials involving alemtuzumab are available (Table 3). Both trials compared the efficacy of alemtuzumab against IFNβ-1a in the treatment of RRMS. Superiority of alemtuzumab over active comparator in terms of relapse reduction, reduced inflammatory lesion activity, and reduced rate of brain parenchymal fraction reduction (a measure of brain atrophy) was observed in both the CARE-MS I and CARE-MS II studies [91, 92]. CARE-MS II also demonstrated improvement in sustained disability progression versus IFNβ-1a [92], although a disability benefit according to the Expanded Disability Status Scale compared with IFNβ-1a was not seen in the CARE-MS I trial [91].
The most common adverse events associated with alemtuzumab were headache, diarrhea, and flu-like symptoms (summarized in Table 4). Infections were more frequent with alemtuzumab than with IFNβ; notably cutaneous herpes was more common despite prophylactic acyclovir. The most common infections in patients receiving alemtuzumab included upper respiratory and urinary tract infections, sinusitis, and herpes simplex infections. Infections were predominantly mild to moderate in severity and there were no treatment-related life-threatening or fatal infections [91, 92].
Approximately 16–19 % of alemtuzumab-treated patients developed an autoimmune thyroid-related adverse event and approximately 1 % developed a serious thyroid-related event. Approximately 1 % developed immune thrombocytopenic purpura, and patient monitoring for immune cytopenias and thyroid or renal disorders is required for all clinical trials of alemtuzumab in MS [91, 92].
Alemtuzumab treatment significantly depletes mononuclear and lymphocyte subsets. Studies have shown that CD4 cells are depleted for up to 5 years and CD8 cells for 2.5 years. Monocytes and B cells return to baseline levels within 3 months of stopping treatment [90, 93]. Presumably, the capacity for immune-cell reconstitution is age dependent, as it is well documented that thymic production of new T cells declines as part of the normal ageing process [94, 95], although appropriate studies have not been performed on patients older than 55 years [22]. Regardless, as a result of its prolonged effects on WBCs, it is likely that a washout period of several months, at least, may be required following cessation of alemtuzumab therapy, before starting another immunosuppressant treatment.
3 Orally Administered Therapies
3.1 Fingolimod
3.1.1 Mechanism of Action and Immunological Effects
Fingolimod is an orally administered, sphingosine 1-phosphate (S1P) receptor modulator used to treat relapsing forms of MS. It is a chemical derivative of myriocin, a metabolite of the fungus Isaria sinclairii, known for its anti-inflammatory properties [96].
Fingolimod reversibly redistributes lymphocytes into lymphoid tissue, whilst preserving lymphocyte function [97, 98]. By inducing internalization of S1P receptors (S1PRs) expressed on lymphocytes [99], fingolimod primarily inhibits egress of naïve and central memory lymphocytes from lymph nodes back into the circulation [100–102] and thereby prevents them from circulating to other tissues, including the CNS [98, 101]. However, effector memory lymphocytes, which are less dependent on S1P signaling for egress and do not regularly recirculate between lymphoid tissues, are less affected by fingolimod [101, 102]. These cells are mainly located in peripheral tissues and play a key role in preserving immunosurveillance [102].
Animal studies suggest that fingolimod does not impair the ability of lymphocytes (including the lymphocytes that are retained in the lymph nodes) to become activated, proliferate, and produce cytokines or antibodies [100]. The evidence suggests further that fingolimod does not inhibit humoral immunity to systemic viral infection, and does not suppress, or only modestly suppresses, the generation of virus-specific cytotoxic T cells in lymph nodes [102, 103]. Additionally, it has been demonstrated that fingolimod-treated individuals can mount vaccine-specific adaptive immune responses comparable to those of healthy controls [104, 105].
As well as its immunomodulatory effects, fingolimod may have a direct effect on the CNS as it can readily cross the BBB [18]. S1PRs are widely expressed on CNS-resident cells and have been reported to regulate several processes relevant to MS pathology. In animal models of encephalomyelitis, fingolimod, acting via S1PRs, reduced disease severity, restored motor function, and preserved brain tissue [106]. In a variety of different preclinical neurodegenerative models, fingolimod has been found to reduce astrogliosis, demyelination, and axonal loss [99, 101, 107], and protect from exocytotoxic insults, as well as potentially supporting neuroregenerative processes by enhancing recovery of myelin [108], restoring the function of neural cells [109], and increasing levels of neurotrophic factors, such as BDNF [110]. In addition, there is also preclinical evidence indicating that these effects may be independent of reductions in peripheral lymphocyte counts [107]. Recent evidence suggests S1P biology is altered in the CSF and on reactive astrocytes in white and grey matter lesions of MS patients [111–113].
3.1.2 Clinical Effects in Relapsing MS
In 2010, fingolimod became the first oral drug to be approved for the treatment of relapsing forms of MS [18, 19]. Fingolimod reduced relapses by 54 %, and delayed disability progression, lesion activity, and brain volume loss versus placebo over 2 years in the pivotal, randomized FREEDOMS clinical trial (Table 2) [114]. In a head-to-head phase III study of oral daily fingolimod versus IFNβ-1a IM in patients with MS (TRANSFORMS; Table 3), there were significantly greater reductions in relapse rate (52 % relative reduction), lesion activity, and brain volume loss with fingolimod than with IFNβ after 1 year [115]. In addition, meta-analyses indicate that fingolimod is more efficacious in reducing relapses than all IFNβ formulations and GA [116, 117]. The MoA of fingolimod likely accounts for its significant efficacy profile. The ability of fingolimod to readily cross the BBB, and potentially have direct effects within the CNS, may account, at least in part, for the consistently significant reductions (occurring within 6 months) in the progression of brain atrophy observed during all phase III pivotal trials.
The most common adverse events associated with fingolimod therapy are headache, flu-like symptoms, and diarrhea (summarized in Table 4). Fingolimod is generally well tolerated and discontinuation rates due to adverse events and severe adverse events were similar to discontinuation rates in placebo groups [114]. Two fatal herpetic infections occurred in TRANSFORMS in patients who received fingolimod at a higher-than-approved dose of 1.25 mg: one case each of herpes simplex virus encephalitis and disseminated primary varicella infection. The latter occurred in a patient without previous exposure to varicella who was also receiving high-dose corticosteroids for an MS relapse at the time of exposure to primary infection [115]. These cases are reported on a background of more than 71,000 patients treated with fingolimod in both the post-marketing and clinical-trial settings [118], and in a pooled population of patients from two phase III and one phase II studies and their extensions; serious infections were reported in 2.1 % of patients [119].
A core pharmacodynamic effect of fingolimod is a reversible reduction of the peripheral lymphocyte count to approximately 30 % of baseline values [19]. The reversible reduction in lymphocyte counts occurs without an overall increase in infections relative to placebo, suggesting that during fingolimod therapy, peripheral lymphocyte counts do not reflect immunocompetence [119]. The lymphocyte count recovers back to normal levels within 1–2 months after fingolimod treatment discontinuation, and a 6-week washout period is recommended [19].
Another expected and well characterized pharmacodynamic effect is observed at treatment initiation. This first-dose effect presents as a transient, mostly asymptomatic, and self-limiting decrease in heart rate. The transient nature of heart rate effects is explained by the initial functional agonism and subsequent rapid internalization of S1PRs on atrial myocytes [120]. Bradycardia was typically asymptomatic, observed within 6 hours of the first dose, and resolved with continued treatment. Hence, the EU label recommends a 6-hour monitoring period after the first dose and an electrocardiogram prior to treatment initiation [19]. Fingolimod is contraindicated in patients with certain pre-existing heart conditions, stroke, or who are taking certain anti-arrhythmic medications.
Other known adverse effects reported in association with the MoA of fingolimod are generally infrequent and have a known temporal profile, which allows for appropriate monitoring. This includes macular edema occurring in approximately 0.4 % of patients receiving fingolimod 0.5 mg and presenting within 3–4 months of treatment initiation (patients with a history of uveitis appear to have an increased risk), which generally resolved with or without treatment after drug discontinuation [121], and reversible elevation of liver enzymes, mainly occurring in the first 6–12 months of treatment [19].
3.2 Teriflunomide
3.2.1 Mechanism of Action and Immunological Effects
Teriflunomide is an active metabolite of leflunomide, an approved oral therapy for rheumatoid arthritis since 1998 [122]. In 2012, oral teriflunomide was approved for treatment of relapsing forms of MS [20]. The exact mechanism by which teriflunomide exerts its therapeutic effect in MS is not completely understood [123]. It is believed that the drug works by inhibiting dihydroorotate dehydrogenase (DHODH), a mitochondrial enzyme involved in de novo pyrimidine synthesis. By inhibiting DHODH and reducing DNA synthesis, teriflunomide has a cytostatic effect on proliferating T and B cells [124]. However, cellular salvage pathways for proliferation exist and allow slowly dividing T memory cells to sustain ongoing pyrimidine metabolism and to survive [125]. Teriflunomide was shown to interfere with the interaction of T cells and APCs, which is central to the immune response [126].
There is also evidence that teriflunomide blocks TNFα-induced activation of nuclear factor kappa B (NF-κB) [127], inhibits adhesion molecules and matrix metalloproteinases [128], and disrupts the interaction between T cells and APCs and integrin signaling during T-cell activation [129]. In vitro studies using Jurkat and cytotoxic T-lymphocyte line-4 cells have demonstrated the inhibition of tyrosine kinase pathways following teriflunomide administration [130]. Animal experiments with leflunomide have shown that some immunosuppressive effects can be reversed by uridine as a substitute for inhibited DHODH-dependent pyrimidine synthesis, whereas others cannot, thus attesting to the in vivo relevance of the compound’s interference with immune cell signaling [131].
3.2.2 Clinical Effects in Relapsing MS
Teriflunomide has been associated with significant efficacy (in terms of reducing relapses by approximately 30 % and delaying disability progression [14-mg dose only]) versus placebo in the pivotal, randomized TEMSO [132] and TOWER [133] clinical trials (Table 2). In addition, a head-to-head study has been conducted showing no superiority of oral daily teriflunomide versus IFNβ-1a SC in patients with MS (TENERE; Table 3).
The most common adverse events with teriflunomide are alopecia, diarrhea, and flu-like symptoms (summarized in Table 4). The increase in liver enzyme levels is of interest. As stated, teriflunomide is the active metabolite of leflunomide. Liver toxicity is one of the most serious safety concerns associated with leflunomide. In rare cases, leflunomide has been associated with severe hepatic injury leading to death in patients with rheumatoid arthritis. As a consequence, MS care providers should monitor liver function prior to and during treatment with teriflunomide [134].
A mean decrease in lymphocyte count of approximately 15 % and in platelet count of approximately 10 % was observed, but no overall increase in the risk of serious infections was reported in clinical trials with teriflunomide [132]. Fatal infections have been reported in the post-marketing setting in patients receiving leflunomide [134].
Teriflunomide is teratogenic in animal models and so women of childbearing potential must present a negative pregnancy test before starting the drug and use effective birth control during treatment [134].
Teriflunomide is eliminated slowly from plasma. Without an accelerated elimination procedure, it takes an average of 8 months to reach plasma concentrations <0.02 mg/L, although because of individual variations in drug clearance it may take as long as 2 years [134]. An accelerated elimination procedure could be used at any time after discontinuation of teriflunomide. Elimination can be accelerated by using either cholestyramine or oral activated charcoal powder for 11 days [134]. At the end of 11 days, both regimens successfully accelerated teriflunomide elimination, leading to a more than 98 % decrease in teriflunomide plasma concentrations.
3.3 Dimethyl Fumarate (BG-12)
3.3.1 Mechanism of Action and Immunological Effects
Dimethyl fumarate (DMF) is a methyl ester of fumaric acid. Early reports identified it as a potent cell radio-sensitizer. The large enhancement of radiation sensitivity was due to thiol depletion, thought to be responsible for radio resistance [135]. Fumaric acid esters have also been used successfully as psoriasis therapy since 1959 and are thought to have therapeutic potential for other dermatological and non-dermatological conditions [136].
The MoA by which DMF exerts its therapeutic effect in MS is not fully understood [137]. It has been proposed that fumarates may promote cytoprotection via the nuclear factor (erythroid-derived 2)-like 2 (Nrf2) transcription pathway [138]. DMF is rapidly metabolized to the metabolite, monomethyl fumarate (MMF). Both DMF and MMF have short half-lives, so DMF requires twice-daily administration [137]. DMF and MMF have been shown to activate the Nrf2 pathway in vitro and in vivo in animals and humans [137], with a corresponding increase in cellular redox potential, glutathione levels, adenosine triphosphate levels, mitochondrial membrane potential, and other anti-oxidative effects resulting in cytoprotective effects [138, 139]. It is worth noting that activation of the Nrf2 pathway has been implicated in tumorigenesis [140], although the clinical relevance of this in MS is unclear.
Other reported immunosuppressive effects of DMF include induction of the anti-inflammatory heme oxygenase protein via glutathione depletion [141], inhibition of cytokine-induced nuclear translocation of NF-κB apoptosis of stimulated T cells [142], and modulation of B-cell apoptosis and upregulation of monocyte superoxide anion production [143]. In vitro studies have indicated the role of DMF in promoting the Th2-associated cytokines IL-4 and IL-5 in stimulated T cells, while down-regulating Th1 responses and inhibiting expression of intracellular adhesion molecule-1, E-selectin, and VCAM-1 [144]. Additionally, DMF has been identified as a nicotinic acid receptor agonist in vitro [137], which may be linked to the flushing events observed in MS patients (Table 2) [145].
3.3.2 Clinical Effects in Relapsing MS
DMF was approved in 2013 for treatment of relapsing forms of MS [21, 146]. DMF has shown significant efficacy (in terms of reducing relapses by 53 %, delaying disability progression, and reducing the number of gadolinium-enhancing and new or enlarging T2-weighted hyperintense lesions) versus placebo in the DEFINE trial (Table 2) [147]. In another 2-year, phase III study with GA as a reference comparator (CONFIRM), DMF reduced inflammatory disease activity and did not significantly reduce disability progression [148].
The most common adverse events associated with DMF therapy are flushing, abdominal pain, and diarrhea (summarized in Table 4). The incidence of gastrointestinal events was higher early in the course of treatment (primarily in month 1) and usually decreased over time in patients treated with DMF versus placebo. A total of 5 and 6 % of patients in twice-daily and thrice-daily groups, respectively, discontinued DMF due to gastrointestinal events in DEFINE [147]. DMF has also been associated with elevation of hepatic transaminases (mostly <3 times the upper limit of normal) and transient increase in mean eosinophil counts was seen during the first 2 months of therapy [137].
In CONFIRM and DEFINE, mean lymphocyte counts decreased by approximately 30 % during the first year of treatment with DMF and then remained stable [137, 147, 148]. Guidance on a washout period between stopping DMF therapy and starting another MS therapy is not currently available. According to the US label, mean lymphocyte counts increased, but did not return to baseline, 4 weeks after stopping DMF [137]. The incidence of infections and serious infections was reported to be comparable to that with placebo; however, there have been a total of four reports of PML and one report of Kaposi’s sarcoma [149] in patients with psoriasis who were treated with fumarates (treatment with a mixture of DMF and the calcium, magnesium, and zinc salts of ethylhydrogen fumarate with the registered trade name of Fumaderm®) in the context of 180,000 patient-years of Fumaderm® treatment [149–151]. To date, there have been no reports of PML or Kaposi’s sarcoma among patients with MS treated with DMF [147, 148].
4 Therapies in Late-Stage Development
4.1 Laquinimod
4.1.1 Mechanism of Action and Immunological Effects
Laquinimod is a synthetic, experimental compound being investigated as an oral treatment for MS. Laquinimod is a successor to the discontinued experimental drug linomide [152]. Linomide was tested in phase III trials, but clinical development was terminated due to severe cardiovascular toxicity [152]. Chemical modification of the linomide structure has given laquinimod a favorable toxicological profile and improved potency in EAE animal models [153].
Laquinimod is thought to work by shifting the CD4+ phenotype from the proinflammatory Th1 pattern in favor of the Th2/Th3 pattern (increased IL-4 and IL-10 production) and inhibiting the infiltration of inflammatory cells into the CNS [23, 154]. Several groups have also shown that laquinimod reduces leukocyte migration into the CNS [153, 155]. Another potential MoA is the suppression of major histocompatibility complex class II antigen presentation and down-regulation of epitope spreading [156].
As well as these immunomodulatory effects, it has been postulated that laquinimod may confer a degree of neuroprotection. Treatment with laquinimod is associated with significantly higher levels of BDNF in the CNS [23]. In animal models, laquinimod crossed the BBB. In doing so, laquinimod might exert direct effects within the CNS, although it is not yet clear how this may occur, or indeed whether this has any relevance in a clinical setting [157].
4.1.2 Clinical Effects in Relapsing MS
In a phase III, randomized, placebo-controlled study in patients with RRMS (ALLEGRO), treatment with laquinimod led to a modest but significant reduction in the mean ARR, a significant reduction in disability progression, and a significantly reduced number of both gadolinium-enhancing and new or enlarging T2-weighted lesions compared with placebo (Table 2) [158]. In a second phase III, randomized, placebo- and IFNβ-1a IM-controlled study in patients with RRMS (BRAVO), laquinimod significantly reduced progression of disability and brain atrophy. In this study, laquinimod failed to reduce the ARR versus placebo in the primary analysis (Table 3). However, when the data were adjusted for baseline clinical factors associated with relapse rate that were imbalanced between treatment groups, the ARR in the placebo group increased to lead to a statistically significant advantage for laquinimod over placebo [159].
The most common adverse events associated with laquinimod therapy are headache, nasopharyngitis, and back pain (summarized in Table 4). In clinical trials, back pain, cough, headache, and depression appeared to occur more frequently with laquinimod than with placebo [158, 159]. In the phase III studies, most adverse events were similar to placebo in frequency [158, 159], although transient elevations of alanine aminotransferase ≥3 times the normal level were seen more frequently with laquinimod than placebo and IFNβ [158, 159].
4.2 Daclizumab
4.2.1 Mechanism of Action and Immunological Effects
Daclizumab is a humanized monoclonal antibody which binds to the α-subunit (CD25) of the IL-2 receptor expressed on activated T cells and CD4+CD25+FoxP3+ regulatory T cells [160]. This results in the inhibition of several IL-2-dependent T-cell functions, including antigen- and mitogen-induced proliferation, cytokine secretion by activated Th1 and Th2 lymphocytes, and interference with CD28-dependent CD40 ligand expression [161]. It has also been proposed that daclizumab results in expansion and activation of immunoregulatory CD56bright natural-killer cells, which are able to gain access to the CNS and suppress activation of pathogenic immune responses [162].
4.2.2 Clinical Effects in Relapsing MS
Daclizumab is administered by subcutaneous injection every 4 weeks. Phase II clinical trials showed that daclizumab, as add-on or monotherapy in RRMS, had a dose-dependent effect on reducing relapse rate, disability progression, and the number and volume of gadolinium-enhancing T1 and T2 lesions over 12 months [163, 164]. Adverse events were equally distributed across treatment groups; however, serious adverse events attributed to daclizumab treatment emerged. These were categorized into four main groups: infections, skin reactions, liver abnormalities, and autoimmune phenomena [160]. Phase III clinical trials in patients with RRMS are ongoing [165].
4.3 Ocrelizumab
4.3.1 Mechanism of Action and Immunological Effects
Ocrelizumab is a humanized, recombinant monoclonal antibody reactive against CD20, which is widely expressed on B cells [166]. It is administered as an intravenous infusion on days 1 and 15 at approximately 6-month intervals [167]. Treatment with ocrelizumab results in B-cell depletion [167], but the precise role of this activity in MS is not known.
4.3.2 Clinical Effects in Relapsing MS
A phase II clinical trial showed that ocrelizumab had a dose-dependent effect on reducing the number of gadolinium-enhancing T1 lesions over 24 weeks compared with placebo in patients with RRMS [167]. A similar proportion of patients had adverse events across treatment groups, although a higher proportion of patients receiving ocrelizumab had infusion-related adverse events than in the placebo group [167]. Phase III clinical trials in patients with RRMS are ongoing [168].
5 Discussion
Several injectable, and now oral, DMTs are currently available, or in late-stage clinical development, for the treatment of relapsing forms of MS. All of the therapies described in this review are believed to suppress autoreactive peripheral lymphocyte activity in CNS compartments, which remains a critical step in the process of demyelination and tissue damage in MS. Yet each therapy has its own MoA and, as a consequence, each has a different efficacy and safety profile. In some cases, the exact pharmacological mechanisms accounting for the therapeutic effects of an MS treatment remain unknown. For example, studies on IFN, GA, DMF, and laquinimod have demonstrated widespread effects within the immune system. Other therapies, such as natalizumab, fingolimod, teriflunomide, and alemtuzumab seem to exert a more direct effect on lymphocytes. Additionally, some therapies might have neuroprotective effects, although via differing mechanisms and with different levels of supporting evidence [23, 110, 169].
All the DMTs described here are able to reduce the risk of inflammatory disease activity, as assessed by relapse rate and magnetic resonance (MRI) lesion activity, compared with placebo. However, few comparative head-to-head trials have been undertaken to assess the superiority or non-inferiority of one therapy against another, and there is a need for such evidence now that numerous treatments for MS are available. Those trials that have been undertaken indicate that alemtuzumab and fingolimod provide greater efficacy than IFNβ [92, 115].
The ability of DMTs to reduce markers of disease activity early in the disease course is an important long-term efficacy consideration because the presence of these markers, such as MRI lesion burden and clinical parameters, correlate with severe disability in the long term [170–172]. Early identification of probable treatment response using these markers enables patients with a poor response to be switched to an alternative therapy at an early stage [170–172]. Additionally, brain atrophy has been shown to correlate with long-term disease progression [173]. In this regard, fingolimod is the only MS DMT to have demonstrated consistently reduced brain-volume loss (a measure of atrophy) across all of its phase III trials compared with placebo and IFNβ [114, 115].
Finally, the route of drug administration is usually a significant determinant of a patient’s therapy preference. IFNβ-1a and 1b and GA are administered by SC or IM injections; natalizumab and alemtuzumab are administered by intravenous infusion; fingolimod, teriflunomide, and laquinimod are administered orally once daily; and DMF twice daily. As such, deciding on an MS treatment pathway to match patients’ needs may also require physicians to evaluate the potential for a particular treatment regimen to affect patients’ long-term adherence to therapy, which in turn directly affects clinical outcomes, such as relapse rate [174].
6 Conclusions
Understanding the immunological mechanisms and associated clinical profiles of each therapy for MS is important, as treatment tailored to provide optimal efficacy for patients and potential adverse events can be readily identified and managed appropriately. In light of our evolving knowledge of the immunological mechanisms of some of the newer therapies for MS, there appears to be a need for the development of treatment algorithms to help physicians decide on the most effective treatment pathway from the earliest stage of MS, so that patients can benefit from high efficacy, high tolerability treatments throughout the course of their disease.
References
Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372:1502–17.
Frohman EM, Racke MK, Raine CS. Multiple sclerosis—the plaque and its pathogenesis. N Engl J Med. 2006;354:942–55.
Peterson LK, Fujinami RS. Inflammation, demyelination, neurodegeneration and neuroprotection in the pathogenesis of multiple sclerosis. J Neuroimmunol. 2007;184:37–44.
McQualter JL, Bernard CC. Multiple sclerosis: a battle between destruction and repair. J Neurochem. 2007;100:295–306.
Parfenov V, Schluep M, Du Pasquier R. Assessing risks of multiple sclerosis therapies. J Neurol Sci. 2013;332:59–65.
EMA. AVONEX Summary of product characteristics. 2007. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000102/WC500029425.pdf. Accessed 10 Dec 2013.
EMA. Rebif Summary of product characteristics. 2008. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000136/WC500048681.pdf. Accessed 10 Dec 2013.
EMA. Betaferon Summary of product characteristics. 2006. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000081/WC500053225.pdf. Accessed 10 Dec 2013.
EMA. Extavia Summary of product characteristics. 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000933/WC500034701.pdf. Accessed 10 Dec 2013.
MHRA. Copaxone Summary of product characteristics. 2006. http://www.mhra.gov.uk/home/groups/l-unit1/documents/websiteresources/con025676.pdf. Accessed 10 Dec 2013.
U.S. Food and Drug Administration. Copaxone US prescribing information. 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020622s057lbl.pdf. Accessed 10 Dec 2013.
U.S. Food and Drug Administration. Rebif US prescribing information. 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/103780s5140lbl.pdf. Accessed 10 Dec 2013.
Biogen Idec. Avonex US prescribing information. 2013. http://www.avonex.com/pdfs/guides/Avonex_Prescribing_Information.pdf. Accessed Oct 2013.
Novartis. Extavia US prescribing information. 2012. http://www.pharma.us.novartis.com/product/pi/pdf/extavia.pdf. Accessed 10 Dec 2013.
Bayer. Betaseron US prescribing information. 2013. http://labeling.bayerhealthcare.com/html/products/pi/Betaseron_PI.pdf. Accessed Oct 2013.
EMA. Tysabri European summary of product characteristics. 2011. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000603/WC500044686.pdf. Accessed 10 Dec 2013.
U.S. Food and Drug Administration. Tysabri US prescribing information. Revised January 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/125104s0576lbl.pdf. Accessed 10 Dec 2013.
EMA. Gilenya European summary of product characteristics. 2011. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002202/WC500104528.pdf. Accessed 10 Dec 2013.
U.S. Food and Drug Administration. Gilenya (fingolimod): revised US prescribing information. 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/022527s008lbl.pdf. Accessed 10 Dec 2013.
Sanofi. Aubagio US prescribing information. 2012. http://products.sanofi.us/aubagio/aubagio.pdf. Accessed 10 Dec 2013.
Biogen Idec. Tecfidera US prescribing information. 2013. http://www.tecfidera.com/pdfs/full-prescribing-information.pdf. Accessed Oct 2013.
EMA. Lemtrada Summary of product characteristics. 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003718/WC500150521.pdf. Accessed 10 Dec 2013.
Buzzard KA, Broadley SA, Butzkueven H. What do effective treatments for multiple sclerosis tell us about the molecular mechanisms involved in pathogenesis? Int J Mol Sci. 2012;13:12665–709.
Guarda G, Braun M, Staehli F, Tardivel A, Mattmann C, Forster I, et al. Type I interferon inhibits interleukin-1 production and inflammasome activation. Immunity. 2011;34:213–23.
Kolumam GA, Thomas S, Thompson LJ, Sprent J, Murali-Krishna K. Type I interferons act directly on CD8 T cells to allow clonal expansion and memory formation in response to viral infection. J Exp Med. 2005;202:637–50.
Booss J, Esiri MM, Tourtellotte WW, Mason DY. Immunohistological analysis of T lymphocyte subsets in the central nervous system in chronic progressive multiple sclerosis. J Neurol Sci. 1983;62:219–32.
Kuhlmann T, Lingfeld G, Bitsch A, Schuchardt J, Bruck W. Acute axonal damage in multiple sclerosis is most extensive in early disease stages and decreases over time. Brain. 2002;125:2202–12.
Kozovska ME, Hong J, Zang YC, Li S, Rivera VM, Killian JM, et al. Interferon beta induces T-helper 2 immune deviation in MS. Neurology. 1999;53:1692–7.
Rudick RA, Ransohoff RM, Lee JC, Peppler R, Yu M, Mathisen PM, et al. In vivo effects of interferon beta-1a on immunosuppressive cytokines in multiple sclerosis. Neurology. 1998;50:1294–300.
Chen M, Chen G, Nie H, Zhang X, Niu X, Zang YC, et al. Regulatory effects of IFN-beta on production of osteopontin and IL-17 by CD4+ T Cells in MS. Eur J Immunol. 2009;39:2525–36.
Mirandola SR, Hallal DE, Farias AS, Oliveira EC, Brandao CO, Ruocco HH, et al. Interferon-beta modifies the peripheral blood cell cytokine secretion in patients with multiple sclerosis. Int Immunopharmacol. 2009;9:824–30.
Prinz M, Schmidt H, Mildner A, Knobeloch KP, Hanisch UK, Raasch J, et al. Distinct and nonredundant in vivo functions of IFNAR on myeloid cells limit autoimmunity in the central nervous system. Immunity. 2008;28:675–86.
Schmidt H, Raasch J, Merkler D, Klinker F, Krauss S, Bruck W, et al. Type I interferon receptor signalling is induced during demyelination while its function for myelin damage and repair is redundant. Exp Neurol. 2009;216:306–11.
Dhib-Jalbut S, Marks S. Interferon-beta mechanisms of action in multiple sclerosis. Neurology. 2010;74(Suppl 1):S17–24.
Oliver BJ, Kohli E, Kasper LH. Interferon therapy in relapsing–remitting multiple sclerosis: a systematic review and meta-analysis of the comparative trials. J Neurol Sci. 2011;302:96–105.
Rice GP, Incorvaia B, Munari L, Ebers G, Polman C, D’Amico R, et al. Interferon in relapsing–remitting multiple sclerosis. Cochrane Database Syst Rev. 2001;CD002002.
Shirani A, Zhao Y, Karim ME, Evans C, Kingwell E, van der Kop ML, et al. Association between use of interferon beta and progression of disability in patients with relapsing–remitting multiple sclerosis. JAMA. 2012;308:247–56.
Sato DK, Nakashima I, Fukazawa T, Shimizu Y, Tomizawa Y, Yokoyama K, et al. Neutralizing antibodies are associated with a reduction of interferon-beta efficacy during the treatment of Japanese multiple sclerosis patients. Tohoku J Exp Med. 2012;228:85–92.
van der Voort LF, Gilli F, Bertolotto A, Knol DL, Uitdehaag BM, Polman CH, et al. Clinical effect of neutralizing antibodies to interferon beta that persist long after cessation of therapy for multiple sclerosis. Arch Neurol. 2010;67:402–7.
Clinicaltrials.gov. Efficacy and safety study of BIIB017 (ADVANCE). 2009. http://clinicaltrials.gov/ct2/show/NCT00906399?term=advance+multiples+sclerosis&rank=1. Accessed 14 Feb 2014.
Teva Neuroscience I. Copaxone US prescribing information. 2014. http://www.copaxone.com/Resources/pdfs/PrescribingInformation.pdf. Accessed 10 Feb 2014.
Copaxone (glatiramer acetate). US prescribing information. 2009. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020622s057lbl.pdf. Accessed 10 Dec 2013.
Prat A, Biernacki K, Antel JP. Th1 and Th2 lymphocyte migration across the human BBB is specifically regulated by interferon beta and copolymer-1. J Autoimmun. 2005;24:119–24.
Neuhaus O, Hartung HP. In search of a disease marker: the cytokine profile of primary progressive multiple sclerosis. Mult Scler. 2001;7:143–4.
Kala M, Rhodes SN, Piao WH, Shi FD, Campagnolo DI, Vollmer TL. B cells from glatiramer acetate-treated mice suppress experimental autoimmune encephalomyelitis. Exp Neurol. 2010;221:136–45.
Burger D, Molnarfi N, Weber MS, Brandt KJ, Benkhoucha M, Gruaz L, et al. Glatiramer acetate increases IL-1 receptor antagonist but decreases T cell-induced IL-1beta in human monocytes and multiple sclerosis. Proc Natl Acad Sci USA. 2009;106:4355–9.
Ziemssen T, Kumpfel T, Schneider H, Klinkert WE, Neuhaus O, Hohlfeld R. Secretion of brain-derived neurotrophic factor by glatiramer acetate-reactive T-helper cell lines: implications for multiple sclerosis therapy. J Neurol Sci. 2005;233:109–12.
Qizilbash N, Mendez I, Sanchez-de la Rosa R. Benefit-risk analysis of glatiramer acetate for relapsing–remitting and clinically isolated syndrome multiple sclerosis. Clin Ther. 2012;34(159–76):e5.
Cadavid D, Wolansky LJ, Skurnick J, Lincoln J, Cheriyan J, Szczepanowski K, et al. Efficacy of treatment of MS with IFNbeta-1b or glatiramer acetate by monthly brain MRI in the BECOME study. Neurology. 2009;72:1976–83.
O’Connor P, Filippi M, Arnason B, Comi G, Cook S, Goodin D, et al. 250 microg or 500 microg interferon beta-1b versus 20 mg glatiramer acetate in relapsing–remitting multiple sclerosis: a prospective, randomised, multicentre study. Lancet Neurol. 2009;8:889–97.
Mikol DD, Barkhof F, Chang P, Coyle PK, Jeffery DR, Schwid SR, et al. Comparison of subcutaneous interferon beta-1a with glatiramer acetate in patients with relapsing multiple sclerosis (the REbif vs Glatiramer Acetate in Relapsing MS Disease [REGARD] study): a multicentre, randomised, parallel, open-label trial. Lancet Neurol. 2008;7:903–14.
Lublin FD, Cofield SS, Cutter GR, Conwit R, Narayana PA, Nelson F, et al. Randomized study combining interferon and glatiramer acetate in multiple sclerosis. Ann Neurol. 2013;73:327–40.
Racke MK, Lovett-Racke AE, Karandikar NJ. The mechanism of action of glatiramer acetate treatment in multiple sclerosis. Neurology. 2010;74(Suppl 1):S25–30.
U.S. Food and Drug Administration. Mitoxantrone US prescribing information. 2010. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/019297s033s034lbl.pdf. Accessed 18 Feb 2013.
Hartung HP, Gonsette R, Konig N, Kwiecinski H, Guseo A, Morrissey SP, et al. Mitoxantrone in progressive multiple sclerosis: a placebo-controlled, double-blind, randomised, multicentre trial. Lancet. 2002;360:2018–25.
Morrissey SP, Le Page E, Edan G. Mitoxantrone in the treatment of multiple sclerosis. Int MS J. 2005;12:74–87.
Martinelli Boneschi F, Vacchi L, Rovaris M, Capra R, Comi G. Mitoxantrone for multiple sclerosis. Cochrane Database Syst Rev. 2013;5:CD002127.
Leger OJ, Yednock TA, Tanner L, Horner HC, Hines DK, Keen S, et al. Humanization of a mouse antibody against human alpha-4 integrin: a potential therapeutic for the treatment of multiple sclerosis. Hum Antib. 1997;8:3–16.
Rice GP, Hartung HP, Calabresi PA. Anti-alpha4 integrin therapy for multiple sclerosis: mechanisms and rationale. Neurology. 2005;64:1336–42.
Putzki N, Baranwal MK, Tettenborn B, Limmroth V, Kreuzfelder E. Effects of natalizumab on circulating B cells, T regulatory cells and natural killer cells. Eur Neurol. 2010;63:311–7.
Skarica M, Eckstein C, Whartenby KA, Calabresi PA. Novel mechanisms of immune modulation of natalizumab in multiple sclerosis patients. J Neuroimmunol. 2011;235:70–6.
Kivisakk P, Healy BC, Viglietta V, Quintana FJ, Hootstein MA, Weiner HL, et al. Natalizumab treatment is associated with peripheral sequestration of proinflammatory T cells. Neurology. 2009;72:1922–30.
Jilek S, Jaquiery E, Hirsch HH, Lysandropoulos A, Canales M, Guignard L, et al. Immune responses to JC virus in patients with multiple sclerosis treated with natalizumab: a cross-sectional and longitudinal study. Lancet Neurol. 2010;9:264–72.
Marousi S, Karkanis I, Kalamatas T, Travasarou M, Paterakis G, Karageorgiou CE. Immune cells after prolonged natalizumab therapy: implications for effectiveness and safety. Acta Neurol Scand. 2013;128:e1–5.
Selter RC, Biberacher V, Grummel V, Buck D, Eienbröker C, Oertel WH, et al. Natalizumab treatment decreases serum IgM and IgG levels in multiple sclerosis patients. Mult Scler. 2013;19:1454–61.
Saure C, Warnke C, Zohren F, Schroeder T, Bruns I, Cadeddu RP, et al. Natalizumab and impedance of the homing of CD34+ hematopoietic progenitors. Arch Neurol. 2011;68:1428–31.
Bayless KJ, Meininger GA, Scholtz JM, Davis GE. Osteopontin is a ligand for the alpha4beta1 integrin. J Cell Sci. 1998;111(Pt 9):1165–74.
Sehr T, Hainke U, Thomas K, Schultheiss T, Marggraf M, Dartsch S, et al. Natalizumab beyond blood–brain-barrier: CSF concentration and saturation. In: 5th Joint triennial congress of the European and Americas Committees for Treatment and Research in Multiple Sclerosis. Amsterdam, The Netherlands; 2011.
Polman CH, O’Connor PW, Havrdova E, Hutchinson M, Kappos L, Miller DH, et al. A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med. 2006;354:899–910.
Pucci E, Giuliani G, Solari A, Simi S, Minozzi S, Di Pietrantonj C, et al. Natalizumab for relapsing remitting multiple sclerosis. Cochrane Database Syst Rev. 2011;CD007621.
Nikfar S, Rahimi R, Rezaie A, Abdollahi M. A meta-analysis on the efficacy and tolerability of natalizumab in relapsing multiple sclerosis. Arch Med Sci. 2010;6:236–44.
Vennegoor A, Rispens T, Strijbis EM, Seewann A, Uitdehaag BM, Balk LJ, et al. Clinical relevance of serum natalizumab concentration and anti-natalizumab antibodies in multiple sclerosis. Mult Scler. 2013;19:593–600.
Pilz G, Harrer A, Oppermann K, Wipfler P, Golaszewski S, Afazel S, et al. Molecular evidence of transient therapeutic effectiveness of natalizumab despite high-titre neutralizing antibodies. Mult Scler. 2012;18:506–9.
Hunt D, Giovannoni G. Natalizumab-associated progressive multifocal leucoencephalopathy: a practical approach to risk profiling and monitoring. Pract Neurol. 2012;12:25–35.
Biogen-Idec. Natalizumab-associated PML update: March 2013. 2013. http://www.biogenidec-international.com/tysabri.aspx?ID=4763. Accessed Apr 2013.
Sorensen PS, Bertolotto A, Edan G, Giovannoni G, Gold R, Havrdova E, et al. Risk stratification for progressive multifocal leukoencephalopathy in patients treated with natalizumab. Mult Scler. 2012;18:143–52.
Bloomgren G, Richman S, Hotermans C, Subramanyam M, Goelz S, Natarajan A, et al. Risk of natalizumab-associated progressive multifocal leukoencephalopathy. N Engl J Med. 2012;366:1870–80.
Fernandez O. Best practice in the use of natalizumab in multiple sclerosis. Ther Adv Neurol Disord. 2013;6:69–79.
Outteryck O, Zéphir H, Salleron J, Ongagna JC, Etxeberria A, Collongues N, et al. JC-virus seroconversion in multiple sclerosis patients receiving natalizumab. Mult Scler. 2013 [Epub ahead of print].
Vermersch P, Kappos L, Gold R, Foley JF, Olsson T, Cadavid D, et al. Clinical outcomes of natalizumab-associated progressive multifocal leukoencephalopathy. Neurology. 2011;76:1697–704.
Metz I, Radue EW, Oterino A, Kumpfel T, Wiendl H, Schippling S, et al. Pathology of immune reconstitution inflammatory syndrome in multiple sclerosis with natalizumab-associated progressive multifocal leukoencephalopathy. Acta Neuropathol. 2012;123:235–45.
Rinaldi F, Seppi D, Calabrese M, Perini P, Gallo P. Switching therapy from natalizumab to fingolimod in relapsing–remitting multiple sclerosis: clinical and magnetic resonance imaging findings. Mult Scler. 2012;18:1640–3.
Vellinga MM, Castelijns JA, Barkhof F, Uitdehaag BM, Polman CH. Postwithdrawal rebound increase in T2 lesional activity in natalizumab-treated MS patients. Neurology. 2008;70:1150–1.
Berger JR, Centonze D, Comi G, Confavreux C, Cutter G, Giovannoni G, et al. Considerations on discontinuing natalizumab for the treatment of multiple sclerosis. Ann Neurol. 2010;68:409–11.
Killestein J, Vennegoor A, Strijbis EM, Seewann A, van Oosten BW, Uitdehaag BM, et al. Natalizumab drug holiday in multiple sclerosis: poorly tolerated. Ann Neurol. 2010;68:392–5.
Miravalle A, Jensen R, Kinkel RP. Immune reconstitution inflammatory syndrome in patients with multiple sclerosis following cessation of natalizumab therapy. Arch Neurol. 2011;68:186–91.
West TW, Cree BA. Natalizumab dosage suspension: are we helping or hurting? Ann Neurol. 2010;68:395–9.
West TW, Killestein J, Fox RJ. Natalizumab discontinuation: an increasingly tricky proposition. Eur J Neurol. 2012;19:663–4.
Xia MQ, Hale G, Lifely MR, Ferguson MA, Campbell D, Packman L, et al. Structure of the CAMPATH-1 antigen, a glycosylphosphatidylinositol-anchored glycoprotein which is an exceptionally good target for complement lysis. Biochem J. 1993;293(Pt 3):633–40.
Cox AL, Thompson SA, Jones JL, Robertson VH, Hale G, Waldmann H, et al. Lymphocyte homeostasis following therapeutic lymphocyte depletion in multiple sclerosis. Eur J Immunol. 2005;35:3332–42.
Cohen JA, Coles AJ, Arnold DL, Confavreux C, Fox EJ, Hartung HP, et al. Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing–remitting multiple sclerosis: a randomised controlled phase 3 trial. Lancet. 2012;380:1819–28.
Coles AJ, Twyman CL, Arnold DL, Cohen JA, Confavreux C, Fox EJ, et al. Alemtuzumab for patients with relapsing multiple sclerosis after disease-modifying therapy: a randomised controlled phase 3 trial. Lancet. 2012;380:1829–39.
Klotz L, Meuth SG, Wiendl H. Immune mechanisms of new therapeutic strategies in multiple sclerosis—a focus on alemtuzumab. Clin Immunol. 2012;142:25–30.
Mackall CL, Gress RE. Pathways of T-cell regeneration in mice and humans: implications for bone marrow transplantation and immunotherapy. Immunol Rev. 1997;157:61–72.
Aspinall R, Andrew D. Thymic involution in aging. J Clin Immunol. 2000;20:250–6.
Fujita T, Inoue K, Yamamoto S, Ikumoto T, Sasaki S, Toyama R, et al. Fungal metabolites. Part 11. A potent immunosuppressive activity found in Isaria sinclairii metabolite. J Antibiot (Tokyo). 1994;47:208–15.
Pinschewer DD, Ochsenbein AF, Odermatt B, Brinkmann V, Hengartner H, Zinkernagel RM. FTY720 immunosuppression impairs effector T cell peripheral homing without affecting induction, expansion, and memory. J Immunol. 2000;164:5761–70.
Chun J, Hartung HP. Mechanism of action of oral fingolimod (FTY720) in multiple sclerosis. Clin Neuropharmacol. 2010;33:91–101.
Brinkmann V. FTY720 (fingolimod) in multiple sclerosis: therapeutic effects in the immune and the central nervous system. Br J Pharmacol. 2009;158:1173–82.
Mehling M, Brinkmann V, Antel J, Bar-Or A, Goebels N, Vedrine C, et al. FTY720 therapy exerts differential effects on T cell subsets in multiple sclerosis. Neurology. 2008;71:1261–7.
Brinkmann V, Billich A, Baumruker T, Heining P, Schmouder R, Francis G, et al. Fingolimod (FTY720): discovery and development of an oral drug to treat multiple sclerosis. Nat Rev Drug Discov. 2010;9:883–97.
Pinschewer DD, Brinkmann V, Merkler D. Impact of sphingosine 1-phosphate modulation on immune outcomes. Neurology. 2011;76:S15–9.
Walsh KB, Marsolais D, Welch MJ, Rosen H, Oldstone MB. Treatment with a sphingosine analog does not alter the outcome of a persistent virus infection. Virology. 2010;397:260–9.
Mehling M, Hilbert P, Fritz S, Durovic B, Eichin D, Gasser O, et al. Antigen-specific adaptive immune responses in fingolimod-treated multiple sclerosis patients. Ann Neurol. 2011;69:408–13.
Boulton C, Meiser K, David OJ, Schmouder R. Pharmacodynamic effects of steady-state fingolimod on antibody response in healthy volunteers: a 4-week, randomized, placebo-controlled, parallel-group, multiple-dose study. J Clin Pharmacol. 2012;52:1879–90.
Groves A, Kihara Y, Chun J. Fingolimod: direct CNS effects of sphingosine 1-phosphate (S1P) receptor modulation and implications in multiple sclerosis therapy. J Neurol Sci. 2013;328:9–18.
Choi JW, Gardell SE, Herr DR, Rivera R, Lee CW, Noguchi K, et al. FTY720 (fingolimod) efficacy in an animal model of multiple sclerosis requires astrocyte sphingosine 1-phosphate receptor 1 (S1P1) modulation. Proc Natl Acad Sci USA. 2011;108:751–6.
Jackson SJ, Giovannoni G, Baker D. Fingolimod modulates microglial activation to augment markers of remyelination. J Neuroinflamm. 2011;8:76.
Balatoni B, Storch MK, Swoboda EM, Schonborn V, Koziel A, Lambrou GN, et al. FTY720 sustains and restores neuronal function in the DA rat model of MOG-induced experimental autoimmune encephalomyelitis. Brain Res Bull. 2007;74:307–16.
Deogracias R, Yazdani M, Dekkers MP, Guy J, Ionescu MC, Vogt KE, et al. Fingolimod, a sphingosine-1 phosphate receptor modulator, increases BDNF levels and improves symptoms of a mouse model of Rett syndrome. Proc Natl Acad Sci USA. 2012;109:14230–5.
Brana C, Frossard MJ, Pescini Gobert R, Martinier N, Boschert U, Seabrook TJ. Immunohistochemical detection of sphingosine-1-phosphate receptor 1 and 5 in human multiple sclerosis lesions. Neuropathol Appl Neurobiol. 2013 [Epub ahead of print].
Kulakowska A, Zendzian-Piotrowska M, Baranowski M, Kononczuk T, Drozdowski W, Gorski J, et al. Intrathecal increase of sphingosine 1-phosphate at early stage multiple sclerosis. Neurosci Lett. 2010;477:149–52.
van Doorn R, Nijland PG, Dekker N, Witte ME, Lopes-Pinheiro MA, van Het Hof B, et al. Fingolimod attenuates ceramide-induced blood–brain barrier dysfunction in multiple sclerosis by targeting reactive astrocytes. Acta Neuropathol. 2012;124:397–410.
Kappos L, Radue EW, O’Connor P, Polman C, Hohlfeld R, Calabresi P, et al. A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N Engl J Med. 2010;362:387–401.
Cohen JA, Barkhof F, Comi G, Hartung HP, Khatri BO, Montalban X, et al. Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N Engl J Med. 2010;362:402–15.
Del Santo F, Maratea D, Fadda V, Trippoli S, Messori A. Treatments for relapsing–remitting multiple sclerosis: summarising current information by network meta-analysis. Eur J Clin Pharmacol. 2012;68:441–8.
Roskell NS, Zimovetz EA, Rycroft CE, Eckert BJ, Tyas DA. Annualized relapse rate of first-line treatments for multiple sclerosis: a meta-analysis, including indirect comparisons versus fingolimod. Curr Med Res Opin. 2012;28:767–80.
Novartis. Gilenya World Watch. 2013. http://www.gilenyaworldwatch.com/English.html. Accessed 10 Dec 2013.
Francis G, Kappos L, O’Connor P, Collins W, Tang D, Mercier F, et al. Temporal profile of lymphocyte counts and relationship with infections with fingolimod therapy. Mult Scler. 2014;20:471–80.
Cohen JA, Chun J. Mechanisms of fingolimod’s efficacy and adverse effects in multiple sclerosis. Ann Neurol. 2011;69:759–77.
Zarbin MA, Jampol LM, Jager RD, Reder AT, Francis G, Collins W, et al. Ophthalmic evaluations in clinical studies of fingolimod (FTY720) in multiple sclerosis. Ophthalmology. 2013;120:1432–9.
Maddison P, Kiely P, Kirkham B, Lawson T, Moots R, Proudfoot D, et al. Leflunomide in rheumatoid arthritis: recommendations through a process of consensus. Rheumatology (Oxford). 2005;44:280–6.
Palmer AM. Teriflunomide, an inhibitor of dihydroorotate dehydrogenase for the potential oral treatment of multiple sclerosis. Curr Opin Investig Drugs. 2010;11:1313–23.
Cherwinski HM, Cohn RG, Cheung P, Webster DJ, Xu YZ, Caulfield JP, et al. The immunosuppressant leflunomide inhibits lymphocyte proliferation by inhibiting pyrimidine biosynthesis. J Pharmacol Exp Ther. 1995;275:1043–9.
Tanasescu R, Evangelou N, Constantinescu CS. Role of oral teriflunomide in the management of multiple sclerosis. Neuropsychiatr Dis Treat. 2013;9:539–53.
Xu X, Blinder L, Shen J, Gong H, Finnegan A, Williams JW, et al. In vivo mechanism by which leflunomide controls lymphoproliferative and autoimmune disease in MRL/MpJ-lpr/lpr mice. J Immunol. 1997;159:167–74.
Manna SK, Aggarwal BB. Immunosuppressive leflunomide metabolite (A77 1726) blocks TNF-dependent nuclear factor-kappa B activation and gene expression. J Immunol. 1999;162:2095–102.
Kraan MC, Reece RJ, Barg EC, Smeets TJ, Farnell J, Rosenburg R, et al. Modulation of inflammation and metalloproteinase expression in synovial tissue by leflunomide and methotrexate in patients with active rheumatoid arthritis. Findings in a prospective, randomized, double-blind, parallel-design clinical trial in thirty-nine patients at two centers. Arthritis Rheum. 2000;43:1820–30.
Zeyda M, Poglitsch M, Geyeregger R, Smolen JS, Zlabinger GJ, Horl WH, et al. Disruption of the interaction of T cells with antigen-presenting cells by the active leflunomide metabolite teriflunomide: involvement of impaired integrin activation and immunologic synapse formation. Arthritis Rheum. 2005;52:2730–9.
Xu X, Williams JW, Bremer EG, Finnegan A, Chong AS. Inhibition of protein tyrosine phosphorylation in T cells by a novel immunosuppressive agent, leflunomide. J Biol Chem. 1995;270:12398–403.
Pinschewer DD, Ochsenbein AF, Fehr T, Zinkernagel RM. Leflunomide-mediated suppression of antiviral antibody and Tcell responses: differential restoration by uridine. Transplantation. 2001;72:712–9.
O’Connor P, Wolinsky JS, Confavreux C, Comi G, Kappos L, Olsson TP, et al. Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N Engl J Med. 2011;365:1293–303.
Confavreux C, O’Connor P, Comi G, Freedman MS, Miller AE, Olsson TP, et al. Oral teriflunomide for patients with relapsing multiple sclerosis (TOWER): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:247–56.
Aubagio (teriflunomide). US prescribing information. 2013. http://www.aubagio.com. Accessed 10 Dec 2013.
Held KD, Epp ER, Clark EP, Biaglow JE. Effect of dimethyl fumarate on the radiation sensitivity of mammalian cells in vitro. Radiat Res. 1988;115:495–502.
Meissner M, Valesky EM, Kippenberger S, Kaufmann R. Dimethyl fumarate—only an anti-psoriatic medication? J Dtsch Dermatol Ges. 2012;10:793–801.
Tecfidera (dimethyl fumarate). US prescribing information. 2013. http://www.tecfidera.com. Accessed 10 Dec 2013.
Linker RA, Lee DH, Ryan S, van Dam AM, Conrad R, Bista P, et al. Fumaric acid esters exert neuroprotective effects in neuroinflammation via activation of the Nrf2 antioxidant pathway. Brain. 2011;134:678–92.
Scannevin RH, Chollate S, Jung MY, Shackett M, Patel H, Bista P, et al. Fumarates promote cytoprotection of central nervous system cells against oxidative stress via the nuclear factor (erythroid-derived 2)-like 2 pathway. J Pharmacol Exp Ther. 2012;341:274–84.
DeNicola GM, Karreth FA, Humpton TJ, Gopinathan A, Wei C, Frese K, et al. Oncogene-induced Nrf2 transcription promotes ROS detoxification and tumorigenesis. Nature. 2011;475:106–9.
Lehmann JC, Listopad JJ, Rentzsch CU, Igney FH, von Bonin A, Hennekes HH, et al. Dimethylfumarate induces immunosuppression via glutathione depletion and subsequent induction of heme oxygenase 1. J Invest Dermatol. 2007;127:835–45.
Moharregh-Khiabani D, Blank A, Skripuletz T, Miller E, Kotsiari A, Gudi V, et al. Effects of fumaric acids on cuprizone induced central nervous system de- and remyelination in the mouse. PLoS One. 2010;5:e11769.
Moharregh-Khiabani D, Linker RA, Gold R, Stangel M. Fumaric acid and its esters: an emerging treatment for multiple sclerosis. Curr Neuropharmacol. 2009;7:60–4.
Vandermeeren M, Janssens S, Borgers M, Geysen J. Dimethylfumarate is an inhibitor of cytokine-induced E-selectin, VCAM-1, and ICAM-1 expression in human endothelial cells. Biochem Biophys Res Commun. 1997;234:19–23.
Hanson J, Gille A, Zwykiel S, Lukasova M, Clausen BE, Ahmed K, et al. Nicotinic acid- and monomethyl fumarate-induced flushing involves GPR109A expressed by keratinocytes and COX-2-dependent prostanoid formation in mice. J Clin Invest. 2010;120:2910–9.
EMA. Tecfidera summary of opinion (initial authorisation) 2013. http://www.ema.europa.eu/docs/en_GB/document_library/Summary_of_opinion_-_Initial_authorisation/human/002601/WC500140695.pdf. Accessed 10 Feb 2014.
Gold R, Kappos L, Arnold DL, Bar-Or A, Giovannoni G, Selmaj K, et al. Placebo-controlled phase 3 study of oral BG-12 for relapsing multiple sclerosis. N Engl J Med. 2012;367:1098–107.
Fox RJ, Miller DH, Phillips JT, Hutchinson M, Havrdova E, Kita M, et al. Placebo-controlled phase 3 study of oral BG-12 or glatiramer in multiple sclerosis. N Engl J Med. 2012;367:1087–97.
Philipp S, Kokolakis G, Hund M, Witte E, Witte K, Kunz S, et al. Immunological changes in psoriasis patients under long-term treatment with fumaric acid esters: risk of Kaposi sarcoma occurrence? Eur J Dermatol. 2013;23:339–43.
Sweetser MT, Dawson KT, Bozic C. Manufacturer’s response to case reports of PML. N Engl J Med. 2013;368:1659–61.
Biogen Idec. Important letter to healthcare professionals: Fumaderm ® initial/Fumaderm® Avoid the risk of opportunistic infections by adhering to regular laboratory controls and other warnings during therapy. 2013. http://www.bfarm.de/SharedDocs/Risikoinformationen/DE/RHB/2013/rhb-fumaderm.pdf?__blob=publicationFile&v=3. Accessed Feb 2014.
Tan IL, Lycklama à Nijeholt GJ, Polman CH, Adèr HJ, Barkhof F. Linomide in the treatment of multiple sclerosis: MRI results from prematurely terminated phase-III trials. Mult Scler. 2000;6:99–104.
Brunmark C, Runstrom A, Ohlsson L, Sparre B, Brodin T, Astrom M, et al. The new orally active immunoregulator laquinimod (ABR-215062) effectively inhibits development and relapses of experimental autoimmune encephalomyelitis. J Neuroimmunol. 2002;130:163–72.
Yang JS, Xu LY, Xiao BG, Hedlund G, Link H. Laquinimod (ABR-215062) suppresses the development of experimental autoimmune encephalomyelitis, modulates the Th1/Th2 balance and induces the Th3 cytokine TGF-beta in Lewis rats. J Neuroimmunol. 2004;156:3–9.
Wegner C, Stadelmann C, Pfortner R, Raymond E, Feigelson S, Alon R, et al. Laquinimod interferes with migratory capacity of T cells and reduces IL-17 levels, inflammatory demyelination and acute axonal damage in mice with experimental autoimmune encephalomyelitis. J Neuroimmunol. 2010;227:133–43.
Gurevich M, Gritzman T, Orbach R, Tuller T, Feldman A, Achiron A. Laquinimod suppress antigen presentation in relapsing–remitting multiple sclerosis: in-vitro high-throughput gene expression study. J Neuroimmunol. 2010;221:87–94.
Bruck W, Zamvil SS. Laquinimod, a once-daily oral drug in development for the treatment of relapsing–remitting multiple sclerosis. Expert Rev Clin Pharmacol. 2012;5:245–56.
Comi G, Jeffery D, Kappos L, Montalban X, Boyko A, Rocca MA, et al. Placebo-controlled trial of oral laquinimod for multiple sclerosis. N Engl J Med. 2012;366:1000–9.
Vollmer TL, Sorensen PS, Arnold DL. A placebo-controlled and active comparator phase III trial (BRAVO) for relapsing–remitting multiple sclerosis. In: 5th Joint triennial congress of the European and Americas Committees for Treatment and Research in Multiple Sclerosis. Amsterdam, The Netherlands; 2011.
Milo R. The efficacy and safety of daclizumab and its potential role in the treatment of multiple sclerosis. Ther Adv Neurol Disord. 2014;7:7–21.
McDyer JF, Li Z, John S, Yu X, Wu CY, Ragheb JA. IL-2 receptor blockade inhibits late, but not early, IFN-gamma and CD40 ligand expression in human T cells: disruption of both IL-12-dependent and -independent pathways of IFN-gamma production. J Immunol. 2002;169:2736–46.
Bielekova B, Richert N, Herman ML, Ohayon J, Waldmann TA, McFarland H, et al. Intrathecal effects of daclizumab treatment of multiple sclerosis. Neurology. 2011;77:1877–86.
Gold R, Giovannoni G, Selmaj K, Havrdova E, Montalban X, Radue EW, et al. Daclizumab high-yield process in relapsing–remitting multiple sclerosis (SELECT): a randomised, double-blind, placebo-controlled trial. Lancet. 2013;381:2167–75.
Wynn D, Kaufman M, Montalban X, Vollmer T, Simon J, Elkins J, et al. Daclizumab in active relapsing multiple sclerosis (CHOICE study): a phase 2, randomised, double-blind, placebo-controlled, add-on trial with interferon beta. Lancet Neurol. 2010;9:381–90.
Clinicaltrials.gov. Safety and efficacy study of daclizumab high yield process to treat relapsing–remitting multiple sclerosis (SELECT). 2006. http://clinicaltrials.gov/ct2/show/NCT00390221?term=Daclizumab&rank=11. Accessed 14 Feb 2014.
Glennie MJ, French RR, Cragg MS, Taylor RP. Mechanisms of killing by anti-CD20 monoclonal antibodies. Mol Immunol. 2007;44:3823–37.
Kappos L, Li D, Calabresi PA, O’Connor P, Bar-Or A, Barkhof F, et al. Ocrelizumab in relapsing–remitting multiple sclerosis: a phase 2, randomised, placebo-controlled, multicentre trial. Lancet. 2011;378:1779–87.
Clinicaltrials.gov. A study of ocrelizumab in comparison with interferon beta-1a (Rebif) in patients with relapsing multiple sclerosis. 2010. http://clinicaltrials.gov/show/NCT01247324. Accessed 14 Feb 2014.
Azoulay D, Mausner-Fainberg K, Urshansky N, Fahoum F, Karni A. Interferon-beta therapy up-regulates BDNF secretion from PBMCs of MS patients through a CD40-dependent mechanism. J Neuroimmunol. 2009;211:114–9.
Bermel RA, You X, Foulds P, Hyde R, Simon JH, Fisher E, et al. Predictors of long-term outcome in multiple sclerosis patients treated with interferon beta. Ann Neurol. 2013;73:95–103.
Goodin DS, Traboulsee A, Knappertz V, Reder AT, Li D, Langdon D, et al. Relationship between early clinical characteristics and long term disability outcomes: 16 year cohort study (follow-up) of the pivotal interferon beta-1b trial in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2012;83:282–7.
Rio J, Castillo J, Rovira A, Tintore M, Sastre-Garriga J, Horga A, et al. Measures in the first year of therapy predict the response to interferon beta in MS. Mult Scler. 2009;15:848–53.
Popescu V, Agosta F, Hulst HE, Sluimer IC, Knol DL, Sormani MP, et al. Brain atrophy and lesion load predict long term disability in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2013;84:1082–91.
Steinberg SC, Faris RJ, Chang CF, Chan A, Tankersley MA. Impact of adherence to interferons in the treatment of multiple sclerosis: a non-experimental, retrospective, cohort study. Clin Drug Investig. 2010;30:89–100.
Brown KA. Factors modifying the migration of lymphocytes across the blood–brain barrier. Int Immunopharmacol. 2001;1:2043–62.
Johnson KP, Brooks BR, Cohen JA, Ford CC, Goldstein J, Lisak RP, et al. Copolymer 1 reduces relapse rate and improves disability in relapsing–remitting multiple sclerosis: results of a phase III multicenter, double-blind placebo-controlled trial. The Copolymer 1 Multiple Sclerosis Study Group. Neurology. 1995;45:1268–76.
Jacobs LD, Cookfair DL, Rudick RA, Herndon RM, Richert JR, Salazar AM, et al. Intramuscular interferon beta-1a for disease progression in relapsing multiple sclerosis. The Multiple Sclerosis Collaborative Research Group (MSCRG). Ann Neurol. 1996;39:285–94.
The PRISMS Study Group. Randomised double-blind placebo-controlled study of interferon beta-1a in relapsing/remitting multiple sclerosis. PRISMS (Prevention of Relapses and Disability by Interferon beta-1a Subcutaneously in Multiple Sclerosis) Study Group. Lancet. 1998;352:1498–504.
The IFNB Multiple Sclerosis Study Group. Interferon beta-1b is effective in relapsing–remitting multiple sclerosis. I. Clinical results of a multicenter, randomized, double-blind, placebo-controlled trial. The IFNB Multiple Sclerosis Study Group. Neurology. 1993;43:655–61.
Koch-Henriksen N, Sorensen PS, Christensen T, Frederiksen J, Ravnborg M, Jensen K, et al. A randomized study of two interferon-beta treatments in relapsing–remitting multiple sclerosis. Neurology. 2006;66:1056–60.
Panitch H, Goodin DS, Francis G, Chang P, Coyle PK, O’Connor P, et al. Randomized, comparative study of interferon beta-1a treatment regimens in MS: The EVIDENCE Trial. Neurology. 2002;59:1496–506.
Durelli L, Verdun E, Barbero P, Bergui M, Versino E, Ghezzi A, et al. Every-other-day interferon beta-1b versus once-weekly interferon beta-1a for multiple sclerosis: results of a 2-year prospective randomised multicentre study (INCOMIN). Lancet. 2002;359:1453–60.
Vermersch P, Czlonkowska A, Grimaldi LM, Confavreux C, Comi G, Kappos L, et al. A multicenter, randomized, parallel-group, rater-blinded study comparing the effectiveness and safety of teriflunomide and subcutaneous interferon beta-1a in patients with relapsing multiple sclerosis. In: 4th Cooperative Meeting of the Consortium of Multiple Sclerosis Centers and Americas Committee for Treatment and Research in MS. San Diego, California; 2012.
Vermersch P, Czlonkowska A, Grimaldi LM, Confavreux C, Comi G, Kappos L, et al. Teriflunomide versus subcutaneous interferon beta-1a in patients with relapsing multiple sclerosis: a randomised, controlled phase 3 trial. Mult Scler. 2013 [Epub ahead of print].
Acknowledgments
This article represents the opinion of the authors in their respective domain of expertise. The authors interpreted the literature, critically revised content for important intellectual aspects, and approved the content for publication. Oxford Pharmagenesis™ Ltd provided literature searches and technical writing support. Funding support and review for accuracy of scientific data was provided by Novartis Pharma AG, Basel, Switzerland.
Conflict of interest
R. Du Pasquier has served on scientific advisory boards for Biogen Idec, Merck Serono, Teva, and Novartis; and has received funding for travel or speaker honoraria from Abbott, Biogen Idec, Teva, Merck Serono, Bayer Schering Pharma, and ViiV. D. Merkler and D. D. Pinschewer have received funding under a research agreement with Novartis Pharma.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Du Pasquier, R.A., Pinschewer, D.D. & Merkler, D. Immunological Mechanism of Action and Clinical Profile of Disease-Modifying Treatments in Multiple Sclerosis. CNS Drugs 28, 535–558 (2014). https://doi.org/10.1007/s40263-014-0160-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-014-0160-8