Abstract
Alzheimer’s disease (AD) is the most common form of dementia, which completely lacks a viable, long-term therapeutic intervention. This is partly due to an incomplete understanding of AD etiology and the possible confounding factors associated with its genotypic and phenotypic heterogeneity. Cerebral amyloid angiopathy (CAA) is a common, yet frequently overlooked, pathology associated with AD. CAA manifests with deposition amyloid-beta (Aβ) within the smooth muscle layer of cerebral arteries and arterioles. The role of Aβ in AD and CAA pathophysiology has long been controversial. Although it has demonstrated toxicity at super-physiological levels in vitro, Aβ load does not necessarily correlate with cognitive demise in humans. In this review, we describe the contributions of CAA to AD pathophysiology and important pathomechanisms that may lead to vascular fragility and hemorrhages. Additionally, we discuss the effect of Aβ on smooth muscle cell phenotype and viability, especially in terms of the complement cascade.
Similar content being viewed by others
Introduction
While memory loss is the most commonly known symptom of Alzheimer’s disease (AD), the disease is also marked by steady decline in all aspects of cognitive function including disruptions of personality, ability to communicate, sensory processing, and basic self-care [1]. Though AD is the most common form of dementia, almost century after being discovered, there are still no viable long-term therapeutic interventions. This may be due in part to an incomplete understanding of AD etiology and possible confounding factors associated with its genotypic and phenotypic heterogeneity. Alarmingly, demographic projections indicate that as the population ages over the next few decades, a rapid increase in the number of individuals presenting with AD is expected [2]. The lack of treatment and growing population at risk for AD demand a reexamination of the premises that have driven research thus far.
Why a New Paradigm?
The most widely accepted theory of AD etiology is known as the Amyloid Cascade Hypothesis, which states that overproduction and extracellular aggregation of the amyloid-beta (Aβ) peptide is the fountainhead of AD. These extracellular Aβ aggregates act to increase neuronal kinase activity and results in phosphorylation of the microtubule associated protein tau [3]. Hyperphosphorylation of tau induces formation of intracellular aggregates known as neurofibrillary tangles and alters intracellular transport along the microtubule tracks [4]. This in turn abolishes neuronal communication, resulting in cell death in a spatially conserved pattern and producing deficits in networks that subserve memory and cognition [5]. Aggregation of Aβ and tau are well-established pathophysiological characteristics of AD brain tissue at autopsy. It is also known that in familial forms of AD, mutations in amyloid precursor protein (APP), Presinilin 1 or Presinilin 2 accelerate Aβ accumulation [6]. Presinilins function as part of the gamma secretase protein complex, one of three proteolytic enzymes responsible for cleaving APP into Aβ or non-amyloidogenic peptides. Autopsy samples from brain parenchyma of patients with familial AD, which account for less than 5 % of all AD cases, present with Aβ and Tau accumulation similar to sporadic AD [7, 8]. Additionally, since the APP gene is located on chromosome 21, individuals with Down’s syndrome (trisomy 21) invariably develop AD-like dementia [9]. However, it is highly uncertain to what degree familial AD and Down’s syndrome recapitulate the initial stages of sporadic AD, which accounts for the vast majority of AD [2]. This is the core of the growing debate surrounding the Amyloid Cascade Hypothesis: Is the place of Aβ aggregation at the origin of AD or a downstream effect from an earlier insult [10]? Additionally, and of considerable concern, multiple recent immunotherapy clinical trials that target and clear Aβ have failed to reverse cognitive loss and, in some cases, have accelerated it [11, 12]. A full analysis of the arguments involved in the question of Aβ as a cause or effect is beyond the scope of this review; however, we will focus on a commonly overlooked aspect of amyloid pathology in patients with Alzheimer’s disease which may contribute to disease onset and severity.
CAA: Alzheimer’s Silent Partner?
While the pathological hallmark of AD consists of extracellular Aβ deposits, cerebral amyloid angiopathy (CAA) manifests with Aβ deposition in the walls of cerebral arteries and arterioles [13]. Specifically, Aβ is deposited in the adventitia and media of the involved arterioles. The order in which the vessels of various brain regions are affected tends to follow a general pattern. Most frequently, arteries of the leptomeninges are first to show signs of pathology, followed shortly by penetrating arterioles in the neocortical grey matter [14]. Vessels to the posterior aspects of the brain are especially impacted, most severely in the occipital lobe but also in the parietal region [15–19]. The frontal cortex has also been reported as a primary site of CAA pathology [20]. The next stage of CAA is characterized by Aβ accumulation in vessels of the olfactory cortex, hippocampus, and cerebellum. Finally, the third stage demonstrates involvement of deep grey and white matter [21, 22]. Histologically, though Aβ distribution in CAA follows a regionally specific path of cortical arterioles, within each vessel, the distribution of Aβ can be patchy and focal, with adjacent histological sections demonstrating heterogeneous degrees of Aβ accumulation. These Aβ deposits can also be classified into three stages based on severity [23]. Initially, Aβ accumulates in the adventitia of affected vessels and Aβ begins to intercalate between smooth muscle cells (SMCs) in the media. Classified as mild CAA, at this stage, Aβ is restricted to the tunica media without SMC death. Moderate CAA is defined by the replacement of SMCs by Aβ and thickening of the media without disruption of the blood–brain barrier. As SMCs are replaced by Aβ, the vessel loses the ability to respond to dynamic changes in blood flow and grows increasingly fragile. Severe CAA denotes extensive Aβ deposition with fragmentation and/or double-barreling of the vessel wall, fibrinoid necrosis, and aneurysm formation [23]. This loss of vessel integrity often results in blood extravasation to the perivascular space.
Moderate to severe CAA is a common comorbidity with AD, identified at autopsy in 75–98 % of AD patients [24, 25]. The role of Aβ in AD and CAA pathophysiology has long been controversial. Although it may have toxic effects at super-physiological levels, Aβ load does not necessarily correlate with cognitive demise in humans [26]. However, it is known that Aβ deposition in CAA is a major contributor to vascular fragility and hemorrhages of various sizes [27]. Very small brain bleeds, or microbleeds, were once thought rare and silent. Recently, it was found that brain microbleeds (BMBs) appear as small, spherical, hypointense foci in magnetic resonance susceptibility-weighted imaging (SWI) [28]. This has allowed for antemortem clinical analysis of microbleed prevalence. One or more BMBs are found in 16–32 % of individuals with AD, but only 3–6 % of healthy adults [29–35]. Even the smallest bleed can have devastating consequences for the neurons within and surrounding the hemorrhage.
Extensive neuronal death within the core of the hemorrhage results from a variety of insults including oxidative stress from the breakdown of heme and free iron metabolism through the Fenton reaction [36, 37]. Additionally, due to the relatively immune privileged state of the brain parenchyma, introduction of novel antigens also elicits a local immune response from microglia, astrocytes, and migrating peripheral immune cells. Together, these result in increased production of complement factors, interleukin 1β, and nitrous oxide [38]. Through perivascular propagation of these inflammatory byproducts, nearby blood vessels are also damaged, further weakening them and increasing the risk of additional bleeding [39]. Indeed, increasing vessel fragility can lead to complete rupture and result in a hemorrhagic stroke. Often, health practitioners are unaware that a patient has CAA until he or she presents with a hemorrhagic stroke into the brain tissue, a devastating event known as intracerebral hemorrhage (ICH).
Clinical analysis of these patients describes probable CAA with supporting pathology, probable CAA, or possible CAA. The former is established only by availability of evacuated hematoma or cortical biopsy with demonstrated congophilic Aβ staining in the absence of other diagnostic lesions [40]. Probable and possible CAA diagnoses are made in patients aged ≥55 years presenting with cortical hemorrhage or microbleed upon patient interview and gradient-echo magnetic resonance imaging (MRI) or computed tomography evidence of one or more lobar hemorrhages in the absence of other hemorrhage etiology [41]. Based on the limitations of current diagnostic methodologies, it will be important for future exploration to focus on genetic and molecular markers that identify patients harboring vascular Aβ pathology.
CAA and the Risk of ICH
Identification of patients with CAA is of paramount consequence due to the association between cerebral microbleeds and frank hemorrhages and the administration of anticoagulant therapy in this population [42, 43]. Alarmingly, even regular use of aspirin, a mild anticoagulant, was found to elevate the risk of ICH in AD [44]. Even without the use of anticoagulants, AD patients have increased risk of hemorrhagic stroke compared to their non-demented peers, despite no increase in the risk of ischemic stroke or stroke overall [45]. ICH is the most deadly type of stroke. Accounting for 19 % of all strokes, ICH has a survival rate of 48–50 % at 30 days and only 38 % live to 1 year post-stroke [46–48]. Those that survive often suffer extensive loss of function and diminished quality of life, even compared to peers that have experienced ischemic stroke [49]. ICH commonly results from small vessel hypertension and manifests in the deep nuclei, cerebellum and pons [50]. Interestingly, ICH in normotensive patients often localizes in a lobar distribution, particularly in the temporal lobe, a region highly susceptible to both CAA and AD [51–53]. These normotensive patients have been shown to harbor CAA pathology in vessels that rupture [50]. A potential tool for identifying patients at risk from ICH is MRI through the SWI signal void caused by iron deposits from microbleeds. Higher prevalence of BMBs correlate with elevated risk of nontraumatic intracerebral hemorrhage (47–56 %) compared to microbleeds present with ischemic stroke (18–28 %) [32]. Microbleeds are damaging to the brain and diagnostic tools or therapeutic interventions would be best administered prior to vessel rupture. This underscores the need to elucidate the mechanisms of ICH in AD with CAA, especially in light of recent pharmacological and genotypic risk factors.
From Brain to Blood: A Switch in Aβ Clearance
Normally, Aβ efflux from the brain parenchyma is mediated by low-density lipoprotein receptor-related protein 1 (LRP-1) when interacting with its ligands alpha-2-macroglobulin (α2M) and apolipoprotein E (APOE) [54, 55], while the receptor for advanced glycation endproducts (RAGE) mediates its influx from peripheral circulation [56]. LRP-1 was decreased on SMCs isolated from patients clinically and pathologically diagnosed with AD. Depressed LRP-1 follows overexpression of myocardin and serum response factor which together downregulate LRP-1 via activation of sterol regulatory element binding protein-2 (SREBP2) [57, 58]. Both myocardin and serum response factor increase due to hypoxia. Hypoperfusion of multiple brain regions is linked to both the development and progression of AD [59, 60]. The result is that cerebrovascular SMCs switch to a non-Aβ clearance phenotypic. Interestingly, there is a disparity between familial and sporadic AD in the spatial accumulation of Aβ plaques around the cerebral vasculature. Specifically, in sporadic AD, there is a spatial association between Aβ plaques in the brain and associated blood vessels near parenchymal plaques. This is not seen in familial AD cases [61]. A leading hypothesis for accumulation of Aβ at the vessel wall is an imbalance between Aβ production and clearance; with decreased clearance as the changing variable in late-onset AD. Together, these suggest a local, non-genetic mechanism upstream of vascular Aβ deposition that could play a major role in initiating CAA.
A separate route of Aβ clearance occurs through nonspecific bulk flow of brain interstitial fluid (ISF). The brain lacks a lymphatic system comparable to the rest of the body, so ISF must travel by retrograde periarterial transport through the Virchow–Robin spaces (VRS). The VRS comprise a functional anatomic compartment associated with penetrating cortical arteries, in which the pia mater at the cortical surface forms a network of channels along the abluminal surface of the artery walls in the subarachnoid space [62–64]. Once solutes, including Aβ, reach the vascular compartment by bulk flow, it is theorized that they are transported up the vessel wall in the VRS via retrograde, pulsatile motion generated through contraction and expansion of the artery [65]. Based on tracer studies in mice, solutes are channeled along the basement membrane between SMCs in the arterial media of cortical arterioles and leptomeningeal arteries [66] down to the Circle of Willis [67]. Similarly, the distribution of Aβ intercalated between adjacent SMCs has been shown in human postmortem tissue [68]. However, at the skull base, solutes drain into the cervical lymphatics before entering venous circulation, which may explain the lack of CAA on the large subarachnoid arteries [69].
The contribution of perivascular drainage to CAA is not yet fully understood. Bulk flow and perivascular drainage are very slow [70] and only responsible for about 10–15 % of Aβ clearance, while the majority is transcytosed across the blood–brain barrier [71]. Drainage could thus be a compensatory mechanism when other routes fail, (such as loss of LRP-1) which, when overloaded, results in CAA and backup of Aβ into the parenchyma. Based on the theoretical model of perivascular flow [65], aged arteries effected by arteriosclerosis or inflammation would become rigid, disrupting their contractile function and thus impeding perivascular flow.
The amyloid cascade hypothesis posits that it is Aβ itself that causes the demise of SMCs. In a transgenic (TgCRND8) mouse model, it was observed that Aβ itself causes these changes in SMCs in cortical arteries [72]. While this may be true in transgenic animals with Swedish and Indiana APP mutations, wild type Aβ fails to show the same degree of neurotoxic effect on primary human SMCs in vitro, as do Dutch and Flemish mutant forms [73, 74]. Specifically, cultured human cerebrovascular SMCs exposed to wild type Aβ show very little change in morphology or viability [73, 74]. Simply increasing the load of wildtype Aβ to physiological disease-state levels is not sufficient to cause cytotoxicity. This begs the question, what entity induces SMC toxicity and vascular fragility if not Aβ? We hypothesize elements of the innate immune system may provide an explanation for vascular fragility.
Complement Cascade: A Link Between Aβ and SMC Death?
The Aβ toxicity observed in vitro may in large part be due to complement cascade activation. Complement, a potent inflammatory cascade, can cause robust cell death if allowed to propagate unchecked. This antimicrobial cascade may be activated by any of three pathways: the Classical Pathway, mediated by C1q assembly to C1 at antigen:antibody complexes on the pathogen surface; the Mannose-Binding Lectin (MBL) Pathway, initiated by direct binding of MBL to the pathogen surface; or the Alternative Pathway, initiated by spontaneous hydrolysis of C3 at the pathogen surface. All three pathways converge at C3 convertase, an enzyme that cleaves complement component 3 (C3) into C3a and C3b. C3b itself is utilized to form additional C3 convertase assemblies. C3 convertase amplifies the cascade and C3b accumulates on the cell membrane. Normally, this accumulation of C3b mediates phagocytosis of an infected or pathogenic cell. However, if C3b density continues to increase, C5 convertase will spontaneously assemble and initiate the terminal lytic pathway of the complement cascade. Membrane attack complex (MAC) is the result. It begins as C5 convertase cleaves C5 into C5b and C5a. C5b binds covalently to the cell membrane and mediates assembly of C6, C7, and C8. Together, these induce insertion and polymerization of multiple C9 monomers, forming the aptly named MAC, a transmembrane pore that punctures and kills the target cell.
There is longstanding evidence for complement activation by Aβ in vivo. Both classical and alternative complement activation products have been found in senile plaques from AD patients [75, 76]. In AD brain tissue, C1q colocalized with Aβ despite a lack of staining for immunoglobulin, the main activator of C1q [77]. It is important to note that anti-Aβ immunotherapy utilizes immunoglobulin that targets Aβ. Assuming that the immunoglobulin is able to activate C1q, this could provide a potential mechanism for the accelerated neurological decline seen in some clinical trials [78]. The overlap of Aβ and C1q in AD patients is also found in the leptomengial and cortical vessels that stain positive for Aβ [79]. Furthermore, C4b (a component of C3 convertase) is also present in Aβ plaques, indicating that C1 is fully assembled and functional. This is supported in vitro, where it is observed that Aβ directly activates C1q [77]. However, early complement activation alone is insufficient to induce cell death. For that, MAC is a prime suspect.
Like complement components from the early cascade, MAC was also found in autopsy samples from AD patients [26, 79–81]. Interestingly, very little MAC was observed in identical brain regions of high pathology controls, which were identified by significant parenchymal Aβ accumulation without concurrent cognitive loss [26]. In AD, MAC is found together with plaques in both the brain parenchyma and blood vessels [26, 79]. At the cellular level, MAC was found at dystrophic neuritis and colocalized to the periphery of myelin near Aβ plaques [80]. In vitro evidence reveals that Aβ is a sufficient to directly and fully activate the complement cascade, inducing formation of MAC [80, 82, 83]. Further analysis shows that the MAC is active and depresses viability in neuronal cell cultures (NT2) [82]. Primary human AD brain as well as SH-SY5Y cells (a neuroblastoma line differentiates into neuron-like cells upon treatment with retinoic acid) exposed to Aβ in culture express mRNA for all complement proteins (C1q, C2, C3, C4, C5, C6, C7, C8, and C9). Furthermore, SH-SY5Y express protein for components C1q, C3 and C9 [84]. A similar effect is seen in the vasculature. Postmortem-derived cerebrovascular SMCs express mRNA for all components of the complement cascade, except C3. However, C3 and C6 mRNA are elevated by introduction of aggregated Aβ [85]. Under the same conditions, Western blot analysis demonstrated expression of C1r, C1s, C3, C4, C6, C7, C8, and C9 by primary cerebrovascular smooth muscle. Upon treatment with Aβ, C3 protein expression is elevated compared to untreated controls. We speculate that these sources of complement components would be most significant prior to the point at which CAA disrupts the endotheilium. Once the blood–brain barrier is compromised, the cascade components abundant in the circulating plasma will be readily activated by exposed Aβ plaques in the vessel wall.
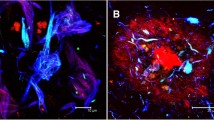
Work from our lab has demonstrated increased C3b levels in occipital lobe parenchyma of AD patients with CAA compared to AD patients without CAA and pathological controls [86]. This increase in C3b was accompanied by a differential binding of Aβ to microglial CD11b and was observed predominantly in patients with CAA [86]. We postulated that this mechanism could result in the increased levels of MAC and Aβ seen on SMCs in CAA. In conjunction with these findings, we also found that the previously discovered AD [87] and CAA [88] risk variant in the CR1 gene (rs6656401) was significantly enriched in patients with CAA compared to those without CAA [86]. The CR1 gene codes for complement receptor 1 (CR1), which is a transmembrane receptor for C3b/C4b, both cleaving complement components and inhibiting their action. CR1 polymorphisms may alter the appropriate protein function and push the complement activation phenotype even further towards MAC deposition. It remains to be determined if complement generation is intended as a protective response; and if so, what factors induce a shift to pathogenesis. Given that SMCs express complement proteins, microglia are observed to deposit C3b along with Aβ, and Aβ itself is sufficient to activate complement, SMCs in CAA-afflicted vessels would be particularly vulnerable to complement attack and lysis.
The potent cytolytic effects of MAC necessitate protective countermeasures on somatic cells. Bystander tissue is generally protected from MAC by constitutive expression of various complement inhibitors. Among these is CD59 (Protectin), a glycoprotein that blocks polymerization of C9 and thus inhibits formation of MAC. Protectin mRNA and protein is decreased in the hippocampus and frontal cortex of AD compared with age-matched non-demented controls. In SH-SY5Y neuronal cultures, Protectin mRNA is diminished in a dose-dependent manner by exposure to Aβ [81]. Furthermore, inhibition of Protectin significantly exacerbates the deleterious effects of Aβ alone in neuron cultures [84]. In blood vessels from patients with AD and CAA, Protectin is not upregulated despite high levels of MAC deposition [86]. This, together with the observation that Aβ induces expression of complement proteins, invites further investigation into the role of complement and MAC in the consequences to smooth muscle observed with CAA and AD.
Conclusions
As demographic trends point to a rapidly growing population afflicted with AD, the means to stop or even slow disease progression remain elusive. To find a therapeutic intervention, it may soon be necessary to break with old paradigms and pursue new avenues of inquiry. As a common AD comorbidity, CAA may be such an avenue. By achieving a deeper understanding of AD with CAA, and the interplay of complement and Aβ, novel therapeutic targets may be discovered. As an additional point of interest, this could also facilitate removal of such patients from clinical trials using therapies that might exacerbate the CAA phenotype including anticoagulants [42, 43, 89] and Aβ immunotherapy [78] (1) to reduce the risk of complications and (2) to remove potential confounding variables that may alter clinical trial outcomes. To ignore CAA, with so high an incidence in AD and so great a potential consequence if left unaddressed, is to ignore a direction of inquiry that is potentially rich in targets for therapeutic intervention.
Abbreviations
- Aβ:
-
Amyloid beta
- AD:
-
Alzheimer’s disease
- APP:
-
Amyloid precursor protein
- BMB:
-
Brain microbleed
- C3:
-
Complement component 3
- CAA:
-
Cerebral amyloid angiopathy
- ICH:
-
Intracerebral hemorrhage
- MAC:
-
Membrane attack complex
- SMC:
-
Smooth muscle cell
References
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack Jr CR, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging—Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–9. doi:10.1016/j.jalz.2011.03.005.
Alzheimer’s A. Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2012;8(2):131–68. doi:10.1016/j.jalz.2012.02.001.
Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297(5580):353–6. doi:10.1126/science.1072994.
Terry RD, Masliah E, Salmon DP, Butters N, DeTeresa R, Hill R, et al. Physical basis of cognitive alterations in Alzheimer’s disease: synapse loss is the major correlate of cognitive impairment. Ann Neurol. 1991;30(4):572–80. doi:10.1002/ana.410300410.
Palop JJ, Mucke L. Amyloid-beta-induced neuronal dysfunction in Alzheimer’s disease: from synapses toward neural networks. Nat Neurosci. 2010;13(7):812–8. doi:10.1038/nn.2583.
Waring SC, Rosenberg RN. Genome-wide association studies in Alzheimer disease. Arch Neurol. 2008;65(3):329–34. doi:10.1001/archneur.65.3.329.
Campion D, Dumanchin C, Hannequin D, Dubois B, Belliard S, Puel M, et al. Early-onset autosomal dominant Alzheimer disease: prevalence, genetic heterogeneity, and mutation spectrum. Am J Human Genet. 1999;65(3):664–70. doi:10.1086/302553.
Nochlin D, van Belle G, Bird TD, Sumi SM. Comparison of the severity of neuropathologic changes in familial and sporadic Alzheimer’s disease. Alzheimer Dis Assoc Disord. 1993;7(4):212–22.
Glenner GG, Wong CW. Alzheimer’s disease and Down’s syndrome: sharing of a unique cerebrovascular amyloid fibril protein. Biochem Biophys Res Commun. 1984;122(3):1131–5.
Castello MA, Soriano S. Rational heterodoxy: cholesterol reformation of the amyloid doctrine. Ageing Res Rev. 2012;12(1):282–8. doi:10.1016/j.arr.2012.06.007.
Doody RS, Raman R, Farlow M, Iwatsubo T, Vellas B, Joffe S, et al. A phase 3 trial of semagacestat for treatment of Alzheimer’s disease. New Engl J Med. 2013;369(4):341–50. doi:10.1056/NEJMoa1210951.
Tayeb HO, Murray ED, Price BH, Tarazi FI. Bapineuzumab and solanezumab for Alzheimer’s disease: is the ‘amyloid cascade hypothesis’ still alive? Exp Opin Biol Ther. 2013;13(7):1075–84. doi:10.1517/14712598.2013.789856.
Vinters HV. Cerebral amyloid angiopathy. A critical review. Stroke. 1987;18(2):311–24.
Preston SD, Steart PV, Wilkinson A, Nicoll JA, Weller RO. Capillary and arterial cerebral amyloid angiopathy in Alzheimer’s disease: defining the perivascular route for the elimination of amyloid beta from the human brain. Neuropathol Appl Neurobiol. 2003;29(2):106–17.
Tomonaga M. Cerebral amyloid angiopathy in the elderly. J Am Geriatr Soc. 1981;29(4):151–7.
Vinters HV, Gilbert JJ. Cerebral amyloid angiopathy: incidence and complications in the aging brain: II. The distribution of amyloid vascular changes. Stroke. 1983;14(6):924–8.
Pfeifer LA, White LR, Ross GW, Petrovitch H, Launer LJ. Cerebral amyloid angiopathy and cognitive function: the HAAS autopsy study. Neurology. 2002;58(11):1629–34.
Attems J, Quass M, Jellinger KA, Lintner F. Topographical distribution of cerebral amyloid angiopathy and its effect on cognitive decline are influenced by Alzheimer disease pathology. J Neurol Sci. 2007;257(1–2):49–55. doi:10.1016/j.jns.2007.01.013.
Attems J. Sporadic cerebral amyloid angiopathy: pathology, clinical implications, and possible pathomechanisms. Acta Neuropathol. 2005;110(4):345–59. doi:10.1007/s00401-005-1074-9.
Masuda J. Incidence of cerebral amyloid angiopathy in autopsy cases in Hisayama, Japan. Nihon Ronen Igakkai Zasshi Jpn J Geriatr. 1985;22(2):138–43.
Thal DR, Ghebremedhin E, Orantes M, Wiestler OD. Vascular pathology in Alzheimer disease: correlation of cerebral amyloid angiopathy and arteriosclerosis/lipohyalinosis with cognitive decline. J Neuropathol Exp Neurol. 2003;62(12):1287–301.
Mann DM, Pickering-Brown SM, Takeuchi A, Iwatsubo T. Members of the familial Alzheimer’s disease pathology study G. Amyloid angiopathy and variability in amyloid beta deposition is determined by mutation position in presenilin-1-linked Alzheimer’s disease. Am J Pathol. 2001;158(6):2165–75.
Vonsattel JP, Myers RH, Hedley-Whyte ET, Ropper AH, Bird ED, Richardson Jr EP. Cerebral amyloid angiopathy without and with cerebral hemorrhages: a comparative histological study. Ann Neurol. 1991;30(5):637–49. doi:10.1002/ana.410300503.
Ellis RJ, Olichney JM, Thal LJ, Mirra SS, Morris JC, Beekly D, et al. Cerebral amyloid angiopathy in the brains of patients with Alzheimer’s disease: the CERAD experience. Part XV. Neurology. 1996;46(6):1592–6.
Jellinger KA, Attems J. Incidence of cerebrovascular lesions in Alzheimer’s disease: a postmortem study. Acta Neuropathol. 2003;105(1):14–7. doi:10.1007/s00401-002-0634-5.
Lue LF, Brachova L, Civin WH, Rogers J. Inflammation, A beta deposition, and neurofibrillary tangle formation as correlates of Alzheimer’s disease neurodegeneration. J Neuropathol Exp Neurol. 1996;55(10):1083–8.
Greenberg SM, O’Donnell HC, Schaefer PW, Kraft E. MRI detection of new hemorrhages: potential marker of progression in cerebral amyloid angiopathy. Neurology. 1999;53(5):1135–8.
Kirsch W, McAuley G, Holshouser B, Petersen F, Ayaz M, Vinters HV, et al. Serial susceptibility weighted MRI measures brain iron and microbleeds in dementia. J Alzheimers Dse. 2009;17(3):599–609. doi:10.3233/JAD-2009-1073.
Roob G, Lechner A, Schmidt R, Flooh E, Hartung HP, Fazekas F. Frequency and location of microbleeds in patients with primary intracerebral hemorrhage. Stroke. 2000;31(11):2665–9.
Hanyu H, Tanaka Y, Shimizu S, Takasaki M, Fujita H, Kaneko N, et al. Cerebral microbleeds in Binswanger’s disease: a gradient-echo T2*-weighted magnetic resonance imaging study. Neurosci Lett. 2003;340(3):213–6.
Nakata Y, Shiga K, Yoshikawa K, Mizuno T, Mori S, Yamada K, et al. Subclinical brain hemorrhages in Alzheimer’s disease: evaluation by magnetic resonance T2*-weighted images. Ann N Y Acad Sci. 2002;977:169–72.
Cordonnier C, Al-Shahi Salman R, Wardlaw J. Spontaneous brain microbleeds: systematic review, subgroup analyses and standards for study design and reporting. Brain. 2007;130(Pt 8):1988–2003. doi:10.1093/brain/awl387.
Jeerakathil T, Wolf PA, Beiser A, Massaro J, Seshadri S, D’Agostino RB, et al. Stroke risk profile predicts white matter hyperintensity volume: the Framingham study. Stroke. 2004;35(8):1857–61. doi:10.1161/01.STR.0000135226.53499.85.
Tsushima Y, Tanizaki Y, Aoki J, Endo K. MR detection of microhemorrhages in neurologically healthy adults. Neuroradiology. 2002;44(1):31–6.
Roob G, Schmidt R, Kapeller P, Lechner A, Hartung HP, Fazekas F. MRI evidence of past cerebral microbleeds in a healthy elderly population. Neurology. 1999;52(5):991–4.
Lara FA, Kahn SA, da Fonseca AC, Bahia CP, Pinho JP, Graca-Souza AV, et al. On the fate of extracellular hemoglobin and heme in brain. J Cereb Blood Flow Metab. 2009;29(6):1109–20. doi:10.1038/jcbfm.2009.34.
Schrag M, Mueller C, Oyoyo U, Smith MA, Kirsch WM. Iron, zinc and copper in the Alzheimer’s disease brain: a quantitative meta-analysis. Some insight on the influence of citation bias on scientific opinion. Prog Neurobiol. 2011;94(3):296–306. doi:10.1016/j.pneurobio.2011.05.001.
Brambilla R, Couch Y, Lambertsen KL. The effect of stroke on immune function. Mol Cell Neurosci. 2013;53:26–33. doi:10.1016/j.mcn.2012.08.011.
Rosand J, Muzikansky A, Kumar A, Wisco JJ, Smith EE, Betensky RA, et al. Spatial clustering of hemorrhages in probable cerebral amyloid angiopathy. Ann Neurol. 2005;58(3):459–62. doi:10.1002/ana.20596.
Greenberg SM, Vonsattel JP. Diagnosis of cerebral amyloid angiopathy. Sensitivity and specificity of cortical biopsy. Stroke. 1997;28(7):1418–22.
Knudsen KA, Rosand J, Karluk D, Greenberg SM. Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria. Neurology. 2001;56(4):537–9.
Biffi A, Halpin A, Towfighi A, Gilson A, Busl K, Rost N, et al. Aspirin and recurrent intracerebral hemorrhage in cerebral amyloid angiopathy. Neurology. 2010;75(8):693–8. doi:10.1212/WNL.0b013e3181eee40f.
Vernooij MW, Haag MD, van der Lugt A, Hofman A, Krestin GP, Stricker BH, et al. Use of antithrombotic drugs and the presence of cerebral microbleeds: the Rotterdam scan study. Arch Neurol. 2009;66(6):714–20. doi:10.1001/archneurol.2009.42.
Thoonsen H, Richard E, Bentham P, Gray R, van Geloven N, De Haan RJ, et al. Aspirin in Alzheimer’s disease: increased risk of intracerebral hemorrhage: cause for concern? Stroke. 2010;41(11):2690–2. doi:10.1161/STROKEAHA.109.576975.
Tolppanen AM, Lavikainen P, Solomon A, Kivipelto M, Soininen H, Hartikainen S. Incidence of stroke in people with Alzheimer disease: a national register-based approach. Neurology. 2013;80(4):353–8. doi:10.1212/WNL.0b013e31827f08c5.
Dennis MS, Burn JP, Sandercock PA, Bamford JM, Wade DT, Warlow CP. Long-term survival after first-ever stroke: the Oxfordshire Community Stroke Project. Stroke. 1993;24(6):796–800.
Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2(1):43–53.
Sacco S, Marini C, Toni D, Olivieri L, Carolei A. Incidence and 10-year survival of intracerebral hemorrhage in a population-based registry. Stroke. 2009;40(2):394–9. doi:10.1161/STROKEAHA.108.523209.
Cadilhac DA, Dewey HM, Vos T, Carter R, Thrift AG. The health loss from ischemic stroke and intracerebral hemorrhage: evidence from the North East Melbourne Stroke Incidence Study (NEMESIS). Health Qual Life Outcomes. 2010;8:49. doi:10.1186/1477-7525-8-49.
Massaro AR, Sacco RL, Mohr JP, Foulkes MA, Tatemichi TK, Price TR, et al. Clinical discriminators of lobar and deep hemorrhages: the Stroke Data Bank. Neurology. 1991;41(12):1881–5.
Itoh Y, Yamada M, Hayakawa M, Otomo E, Miyatake T. Cerebral amyloid angiopathy: a significant cause of cerebellar as well as lobar cerebral hemorrhage in the elderly. J Neurol Sci. 1993;116(2):135–41.
Mesker DJ, Poels MM, Ikram MA, Vernooij MW, Hofman A, Vrooman HA, et al. Lobar distribution of cerebral microbleeds: the Rotterdam scan study. Arch Neurol. 2011;68(5):656–9. doi:10.1001/archneurol.2011.93.
Sepulcre J, Sabuncu MR, Becker A, Sperling R, Johnson KA. In vivo characterization of the early states of the amyloid-beta network. Brain. 2013;136(Pt 7):2239–52. doi:10.1093/brain/awt146.
Deane R, Wu Z, Sagare A, Davis J, Du Yan S, Hamm K, et al. LRP/amyloid beta-peptide interaction mediates differential brain efflux of Abeta isoforms. Neuron. 2004;43(3):333–44. doi:10.1016/j.neuron.2004.07.017.
Kanekiyo T, Liu CC, Shinohara M, Li J, Bu G. LRP1 in brain vascular smooth muscle cells mediates local clearance of Alzheimer’s amyloid-beta. J Neurosci. 2012;32(46):16458–65. doi:10.1523/JNEUROSCI.3987-12.2012.
Deane R, Du Yan S, Submamaryan RK, LaRue B, Jovanovic S, Hogg E, et al. RAGE mediates amyloid-beta peptide transport across the blood–brain barrier and accumulation in brain. Nat Med. 2003;9(7):907–13. doi:10.1038/nm890.
Chow N, Bell RD, Deane R, Streb JW, Chen J, Brooks A, et al. Serum response factor and myocardin mediate arterial hypercontractility and cerebral blood flow dysregulation in Alzheimer’s phenotype. Proc Natl Acad Sci U S A. 2007;104(3):823–8. doi:10.1073/pnas.0608251104.
Bell RD, Deane R, Chow N, Long X, Sagare A, Singh I, et al. SRF and myocardin regulate LRP-mediated amyloid-beta clearance in brain vascular cells. Nat Cell Biol. 2009;11(2):143–53. doi:10.1038/ncb1819.
Huang C, Wahlund LO, Svensson L, Winblad B, Julin P. Cingulate cortex hypoperfusion predicts Alzheimer’s disease in mild cognitive impairment. BMC Neurol. 2002;2:9.
Johnson NA, Jahng GH, Weiner MW, Miller BL, Chui HC, Jagust WJ, et al. Pattern of cerebral hypoperfusion in Alzheimer disease and mild cognitive impairment measured with arterial spin-labeling MR imaging: initial experience. Radiology. 2005;234(3):851–9. doi:10.1148/radiol.2343040197.
Armstrong RA, Cairns NJ, Patel R, Lantos PL, Rossor MN. Relationships between beta-amyloid (A beta) deposits and blood vessels in patients with sporadic and familial Alzheimer’s disease. Neurosci Lett. 1996;207(3):171–4.
Krahn V. The pia mater at the site of the entry of blood vessels into the central nervous system. Anat Embryol (Berl). 1982;164(2):257–63.
Hutchings M, Weller RO. Anatomical relationships of the pia mater to cerebral blood vessels in man. J Neurosurg. 1986;65(3):316–25. doi:10.3171/jns.1986.65.3.0316.
Zhang ET, Inman CB, Weller RO. Interrelationships of the pia mater and the perivascular (Virchow-Robin) spaces in the human cerebrum. J Anat. 1990;170:111–23.
Schley D, Carare-Nnadi R, Please CP, Perry VH, Weller RO. Mechanisms to explain the reverse perivascular transport of solutes out of the brain. J Theor Biol. 2006;238(4):962–74. doi:10.1016/j.jtbi.2005.07.005.
Carare RO, Bernardes-Silva M, Newman TA, Page AM, Nicoll JA, Perry VH, et al. Solutes, but not cells, drain from the brain parenchyma along basement membranes of capillaries and arteries: significance for cerebral amyloid angiopathy and neuroimmunology. Neuropathol Appl Neurobiol. 2008;34(2):131–44. doi:10.1111/j.1365-2990.2007.00926.x.
Szentistvanyi I, Patlak CS, Ellis RA, Cserr HF. Drainage of interstitial fluid from different regions of rat brain. Am J Physiol. 1984;246(6 Pt 2):F835–44.
Soontornniyomkij V, Choi C, Pomakian J, Vinters HV. High-definition characterization of cerebral beta-amyloid angiopathy in Alzheimer’s disease. Hum Pathol. 2010;41(11):1601–8. doi:10.1016/j.humpath.2010.04.011.
Cserr HF, Knopf PM. Cervical lymphatics, the blood–brain barrier and the immunoreactivity of the brain: a new view. Immunol Today. 1992;13(12):507–12. doi:10.1016/0167-5699(92)90027-5.
Bell RD, Sagare AP, Friedman AE, Bedi GS, Holtzman DM, Deane R, et al. Transport pathways for clearance of human Alzheimer’s amyloid beta-peptide and apolipoproteins E and J in the mouse central nervous system. J Cereb Blood Flow Metab. 2007;27(5):909–18. doi:10.1038/sj.jcbfm.9600419.
Shibata M, Yamada S, Kumar SR, Calero M, Bading J, Frangione B, et al. Clearance of Alzheimer’s amyloid-ss(1–40) peptide from brain by LDL receptor-related protein-1 at the blood–brain barrier. J Clin Invest. 2000;106(12):1489–99. doi:10.1172/JCI10498.
Dorr A, Sahota B, Chinta LV, Brown ME, Lai AY, Ma K, et al. Amyloid-beta-dependent compromise of microvascular structure and function in a model of Alzheimer’s disease. Brain. 2012;135(Pt 10):3039–50. doi:10.1093/brain/aws243.
Wang Z, Natte R, Berliner JA, van Duinen SG, Vinters HV. Toxicity of Dutch (E22Q) and Flemish (A21G) mutant amyloid beta proteins to human cerebral microvessel and aortic smooth muscle cells. Stroke. 2000;31(2):534–8.
Davis J, Van Nostrand WE. Enhanced pathologic properties of Dutch-type mutant amyloid beta-protein. Proc Natl Acad Sci U S A. 1996;93(7):2996–3000.
McGeer PL, Akiyama H, Itagaki S, McGeer EG. Activation of the classical complement pathway in brain tissue of Alzheimer patients. Neurosci Lett. 1989;107(1–3):341–6.
Eikelenboom P, Hack CE, Rozemuller JM, Stam FC. Complement activation in amyloid plaques in Alzheimer’s dementia. Virchows Archiv B Cell Pathol Mol Pathol. 1989;56(4):259–62.
Rogers J, Schultz J, Brachova L, Lue LF, Webster S, Bradt B, et al. Complement activation and beta-amyloid-mediated neurotoxicity in Alzheimer’s disease. Res Immunol. 1992;143(6):624–30.
Racke MM, Boone LI, Hepburn DL, Parsadainian M, Bryan MT, Ness DK, et al. Exacerbation of cerebral amyloid angiopathy-associated microhemorrhage in amyloid precursor protein transgenic mice by immunotherapy is dependent on antibody recognition of deposited forms of amyloid beta. J Neurosci. 2005;25(3):629–36. doi:10.1523/JNEUROSCI.4337-04.2005.
Verbeek MM, Otte-Holler I, Veerhuis R, Ruiter DJ, De Waal RM. Distribution of A beta-associated proteins in cerebrovascular amyloid of Alzheimer’s disease. Acta Neuropathol. 1998;96(6):628–36.
Webster S, Lue LF, Brachova L, Tenner AJ, McGeer PL, Terai K, et al. Molecular and cellular characterization of the membrane attack complex, C5b-9, in Alzheimer’s disease. Neurobiol Aging. 1997;18(4):415–21.
Yang LB, Li R, Meri S, Rogers J, Shen Y. Deficiency of complement defense protein CD59 may contribute to neurodegeneration in Alzheimer’s disease. J Neurosci. 2000;20(20):7505–9.
Brandt J, Pippin J, Schulze M, Hansch GM, Alpers CE, Johnson RJ, et al. Role of the complement membrane attack complex (C5b-9) in mediating experimental mesangioproliferative glomerulonephritis. Kidney Int. 1996;49(2):335–43.
Cadman ED, Puttfarcken PS. Beta-amyloid peptides initiate the complement cascade without producing a comparable effect on the terminal pathway in vitro. Exp Neurol. 1997;146(2):388–94. doi:10.1006/exnr.1997.6540.
Shen Y, Sullivan T, Lee CM, Meri S, Shiosaki K, Lin CW. Induced expression of neuronal membrane attack complex and cell death by Alzheimer’s beta-amyloid peptide. Brain Res. 1998;796(1–2):187–97.
Walker DG, Dalsing-Hernandez JE, Lue LF. Human postmortem brain-derived cerebrovascular smooth muscle cells express all genes of the classical complement pathway: a potential mechanism for vascular damage in cerebral amyloid angiopathy and Alzheimer’s disease. Microvasc Res. 2008;75(3):411–9. doi:10.1016/j.mvr.2007.10.004.
Zabel M, Schrag M, Crofton A, Tung S, Beaufond P, Van Ornam J, et al. A shift in microglial beta-amyloid binding in Alzheimer’s disease is associated with cerebral amyloid angiopathy. Brain Pathol. 2012. doi:10.1111/bpa.12005.
Lambert JC, Heath S, Even G, Campion D, Sleegers K, Hiltunen M, et al. Genome-wide association study identifies variants at CLU and CR1 associated with Alzheimer’s disease. Nat Genet. 2009;41(10):1094–9. doi:10.1038/ng.439.
Biffi A, Shulman JM, Jagiella JM, Cortellini L, Ayres AM, Schwab K, et al. Genetic variation at CR1 increases risk of cerebral amyloid angiopathy. Neurology. 2012;78(5):334–41. doi:10.1212/WNL.0b013e3182452b40.
Biffi A, Plourde A, Shen Y, Onofrio R, Smith EE, Frosch M, et al. Screening for familial APP mutations in sporadic cerebral amyloid angiopathy. PloS ONE. 2010;5(11):e13949. doi:10.1371/journal.pone.0013949.
Conflict of Interest
This article does not contain any studies with human or animal subjects. Tanya Cupino and Matthew Zabel declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cupino, T.L., Zabel, M.K. Alzheimer’s Silent Partner: Cerebral Amyloid Angiopathy. Transl. Stroke Res. 5, 330–337 (2014). https://doi.org/10.1007/s12975-013-0309-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-013-0309-7