Abstract
The androgen receptor (AR) is expressed in a majority of ovarian carcinomas, but its role in disease development remains unclear. In this study, AR and a novel AR molecular chaperone called small glutamine-rich tetratricopeptide repeat-containing protein alpha (SGTA) were investigated to assess their potential role in ovarian carcinogenesis. First, an AR and SGTA-positive ovarian cancer cell line was identified to examine whether SGTA influenced AR subcellular localization. Next, relative protein levels of AR and SGTA were measured in two sets of clinical samples: (1) 46 serous ovarian carcinomas (stages I–IV), 9 serous borderline tumors, and 11 benign ovarian tumors; and (2) 24 patient-matched stage III primary and metastatic serous ovarian tumors. Ablation of SGTA protein in OVCAR3 cells significantly increased AR nuclear localization under basal (p ≤ 0.001) and androgen-stimulated (p ≤ 0.001) conditions. In the first clinical set, AR levels were significantly lower in early- (I/II) and late-stage (III/IV) cancers compared with benign (p ≤ 0.001) but not borderline ovarian tumors. SGTA alone did not discriminate between groups but the AR/SGTA ratio was significantly lower in carcinomas and borderline tumors compared with benign tumors (p ≤ 0.001 and 0.015, respectively). In the second clinical set, matched primary and metastatic serous ovarian cancers did not significantly differ for any parameter measured. Collectively, our results suggest that SGTA can influence AR signaling in ovarian cancer cells and that AR signaling capacity may be reduced with the development but not metastatic progression of serous ovarian cancer.
Similar content being viewed by others
Introduction
Ninety percent of human ovarian cancers arise in the ovarian epithelium, and these cancers are the major cause of death from gynecological malignancies [2]. Unfortunately, neither disease-specific symptoms nor effective screening methodologies exist for ovarian cancer. Therefore, the majority of cases are diagnosed with advanced disease and despite aggressive treatment, the 5-year survival rate is less than 30 % [5]. Poor prognosis results from late detection, lack of targeted therapies for advanced disease, and patient relapse with chemoresistant disease [5]. For these reasons, a better understanding of the molecular pathogenesis of ovarian cancer is of critical importance to improve detection and provide new therapeutic targets that may increase patient survival.
Increasing epidemiological evidence suggests an association between androgen hormones and ovarian cancer risk [9, 10, 12, 27, 37]. In vitro studies have shown that androgen treatment of cultured ovarian surface epithelial cells increases cellular proliferation [1, 29, 35]. Additionally, a study in rodents has demonstrated that treatment with testosterone stimulated growth of ovarian surface epithelial cells [30]. Direct androgen action is mediated through the androgen receptor (AR), a hormone-activated transcription factor that is present in up to 90 % of ovarian cancers [1, 6, 8, 14, 15, 19, 31, 33]. Immunoreactive AR is also present in the ovarian surface epithelium and fimbrae of the fallopian tube, both considered to be potential precursor sites of ovarian cancer development [28]. Thus, the AR may play a role in the pathogenesis of ovarian cancer and may have potential for therapeutic targeting [24]. To date, evidence suggests that AR levels may be higher in benign compared with malignant ovarian epithelial cells [6, 18], and higher levels of AR have been associated with improved patient survival in 154 cases of epithelial ovarian cancer [23]. However, whether AR levels differ among the stages of ovarian cancer or differ between a primary tumor and metastatic lesion has yet to be investigated.
The AR is a member of the nuclear receptor superfamily and is subclassed with other steroid hormone receptors including the estrogen (ER) and progesterone receptors (PR) [22]. Unlike ER and PR, the AR predominantly resides in the cytoplasm of the cell as a heterocomplex comprising chaperone heat shock proteins (Hsp70 and Hsp90) and various co-chaperone proteins until adequately stimulated by ligand to enter the nucleus where it can perform its role as a transcription factor [25]. The cytoplasmic-nuclear shuttling of the AR can act as a critical control mechanism for AR function, mediated at least in part by cytoplasmic co-chaperone proteins. Recently, small glutamine-rich tetratricopeptide repeat-containing protein alpha (SGTA) has been identified as an AR co-chaperone protein that can restrain receptor entry into the nucleus of prostate cancer cells until adequate stimulation by AR-specific ligands [4]. The latter study also demonstrated that the ratio of AR to SGTA was abnormally high in the metastases of the AR-dependent disease, prostate cancer [4]. Theoretically, an abnormally high AR/SGTA ratio overrides the restraining capacity of SGTA and promotes AR action by facilitating nuclear entry in the presence of low levels of ligand or by nonspecific ligands. Thus, if present, SGTA may also regulate AR sub-cellular localization in ovarian cancer cells and thereby influence cellular responses to androgens. To date, SGTA expression has not been investigated in female tissues or with respect to ovarian cancer. Therefore, this study aimed to determine if SGTA is expressed in ovarian tissues, whether SGTA influences subcellular localization of AR in an ovarian context, and whether there are differences in the relative levels of AR, SGTA, or the AR/SGTA expression ratio, in pathological ovarian tissues representing different types or stages of disease, with the view to identifying factors that may influence ovarian carcinogenesis.
Materials and Methods
Immunoblotting and Immunocytochemistry
The prostate cancer cell line, C42B, and the ovarian serous cancer cell lines, OVCAR3 and SKOV3, were maintained in RPMI 1640 medium supplemented with 5 % (v/v) fetal bovine serum (FBS).
For immunoblotting, OVCAR3, SKOV3, and C42B cells were plated in 6-well plates (1 × 105 cells/well) in appropriate media containing 5 % steroid-deplete FBS. The next day, cells were treated with vehicle control (ethanol (EtOH)) or 10 nM dihydrotestosterone (DHT; Sigma Aldrich, USA) for 24 h. Cells were lysed in RIPA buffer containing a complete protease inhibitor cocktail (Roche). Protein concentrations were determined using a standard Bradford assay and protein lysates (20 μg) were subjected to PAGE (10 % gel concentration) followed by protein transfer to a nitrocellulose membrane. Membranes were blocked with 3 % skim milk powder in TBS plus Tween 20 before overnight incubation (4 °C) with AR (1/1,000 dilution; N20, Santa Cruz Biotechnologies) or SGTA (1/1,000 dilution; Proteintech Group Inc., IL) primary antibodies. Immunoreactivity was detected using the goat anti-rabbit horseradish peroxidase-conjugated secondary antibody (1:2,000; Dako Corporation, Denmark) and visualization was achieved by enhanced chemiluminescence (Amersham). α-tubulin (1:20,000; Millipore, Ca) was used as the loading control. Western blots were repeated in two independent experiments.
For immunocytochemistry, OVCAR3 cells were plated at a density of 5 × 104/well into 8-well chamber slides (Nuclon™ Lab-Tek II Chamber slide with cover No. 154534, RS Glass Slide, Naperville, IL). Twenty-four hours after seeding, cells were transfected (in duplicate) with 5 nM of SGTA siRNA (s12783, Applied Biosystems) or nonspecific control (Silencer® Select Negative Control No. 1, Applied Biosystems) in oligofectamine (Invitrogen) for 48 h. Slides were then treated for 24 h with 10 nM DHT or vehicle control (EtOH). Slides were fixed in 4 % paraformaldehyde for 10 min at RT, methanol for 3 min at −20 °C, acetone for 1 min at −20 °C, and 0.3 % hydrogen peroxidase for 5 min at room temperature. Slides were incubated with SGTA antibody (diluted 1:2,500) or AR antibody (diluted 1/1,000). Visualization of AR and SGTA was achieved as per immunohistochemical protocol described above. The Video Image Analysis system (described below) was then used to measure the percentage of AR-positive nuclei. Briefly, 10–20 images of OVCAR3 cells at ×20 magnification were captured per replicate for each treatment. The percentage of positive nuclei were then determined for each individual image and the mean for all images/treatment were graphed.
Tissue Cohorts
Archival ovarian tissue samples and relevant clinical data that represented women who had undergone gynecological surgery at the Royal Adelaide Hospital, Adelaide, SA, were obtained for this study following approval by the ethics committees of the University of Adelaide and Royal Adelaide Hospital. Histopathologic diagnosis and staging was determined based on the International Federation of Gynecology and Obstetrics guidelines [3]. To enable high-throughput immunohistochemistry and to minimize staining variation across different sections and samples, cores were taken from formalin-fixed paraffin-embedded ovarian tissue blocks and used to create two tissue microarrays (TMA) as follows:
-
Sample set 1
This TMA was constructed using triplicate cores (1 mm) from 46 cases of serous epithelial ovarian carcinomas and 9 serous borderline tumors. In addition, 11 cases of benign ovarian cystadenoma were collected to serve as a comparative group. The benign cystadenoma tissue samples were used as whole tissue sections and not constructed into a TMA. Patient characteristics for sample set 1 are summarized in Table 1.
Table 1 Summary of patient characteristics -
Sample set 2
This TMA was constructed using triplicate cores (1 mm) of patient-matched stage III primary and omental metastatic epithelial cancer regions from 24 cases. Patient characteristics are summarized in Table 1.
Immunohistochemical Detection
TMA sections and whole tissue sections were processed according to a standard immunohistochemical protocol as previously described [4]. Briefly, sections were incubated in 0.3 % hydrogen peroxide for 5 min, followed by heat-mediated antigen retrieval in 10 mM of sodium citrate buffer (pH 6.5) using a pressure cooker (125 °C for 5 min and 90 °C for 10 min) and overnight exposure (4 °C) to the AR (1/200 dilution; N20) or SGTA (1/2,000 dilution) primary antibodies. Visualization of AR and SGTA was achieved with a standard immunoperoxidase reaction using biotinylated anti-rabbit antibody (1:400; DAKO Corp., Carpinteria, CA), streptavidin-horseradish peroxidase complex (1:500; DAKO), and diaminobenzidine tetrahydrochloride. Human prostate tissue was used as a positive control for AR and SGTA immunostaining, and omission of the primary antibody was used as a negative control. Antibody specificity was further confirmed by Western blot (described above) in which a single band at the expected size was produced for SGTA (34 kDa) and AR (110 kDa) using both ovarian and prostate cell line lysates.
Video Image Analysis
Video image capture and immunohistochemistry quantification was performed as reported previously [32] using a color image analysis system (VideoPro 32, Leading Edge P/L, Marion, SA, Australia). Approximately 10 images of tumor regions per core, or whole tissue section, were collected at a magnification of ×400 and images were edited to isolate epithelium for quantification. Mean integrated optical density (MIOD; average intensity of immunoreactivity per unit area = concentration; arbitrary units) for AR or SGTA was determined for each image. MIOD values were determined for total AR and nuclear AR, the latter as an approximate measure of ligand-activated protein. The MIOD values from images representing one patient were averaged for each antigen and used for statistical analysis.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences version 16.0 for Windows (IBM Corporation, Somers, NY). For sample set 1, cancer stages were combined into two groups: early (stages I and II) and late (stages III and IV). To evaluate differences across groups, the Kruskal–Wallis one-way analysis of variance test was used. The Mann–Whitney U t test was used to assess differences in levels of AR and SGTA between two groups. Spearman’s correlation was used to determine correlation between AR and SGTA levels. Statistical significance for all analyses was set at p < 0.05.
Results
Effect of an Altered AR/SGTA Ratio on AR Subcellular Localization in Ovarian Cells
AR and SGTA proteins were both evident by immunoblotting in the serous ovarian cancer cell line, OVCAR3, and the C42B prostate cancer cell line, used as a positive control (Fig. 1a). SGTA protein was also detected in another ovarian cancer cell line, SKOV3, but this cell line had no detectable levels of AR protein by Western blot, in agreement with previous studies that reported low to undetectable levels of AR in SKOV3 cells [11, 18]. Treatment with 10 nM DHT increased the AR protein levels in the C42B and OVCAR3 cell lines, but still no AR band was detected for SKOV3. Treatment with DHT had no significant effect on SGTA levels in any of the three cell lines.
a Analysis of AR and SGTA in ovarian cancer cell lines. Western blot analysis of SGTA reveals a single band at 34 kDa in protein lysates derived from serous ovarian tumor cell lines (OVCAR3 and SKOV3) and a prostate cancer cell line (C42B). Treatment with dihydrotestosterone (DHT; 10 nM) for 24 h increased immunoreactive AR protein levels but did not alter immunoreactive SGTA protein levels. α-tubulin was used as a loading control. Western blot is a representative example of two experiments. b SGTA mediates AR subcellular localization in OVCAR3 cells. Under control conditions (cells transfected for 48 h with nonspecific siRNA (siN.S.)), SGTA is cytoplasmic (white arrow) and AR is predominantly cytoplasmic with some AR nuclear (black arrow) localization observed. In cells transfected with SGTA-specific siRNA (siSGTA), SGTA levels are visually reduced and AR is predominantly localized to the nucleus of the cells (black arrow), even in the absence of DHT. Magnification at ×200. c Representative images (∼20 images/treatment) of siSGTA and siN.S. transfected cells from duplicate samples were analyzed to measure percentage of AR-positive nuclei. Cells transfected with siSGTA had significantly greater AR-positive nuclei compared with control (siN.S.) in both the absence and presence of DHT (Mann–Whitney U test (in both cases), p ≤ 0.001). Data are presented as the mean percentage (±SEM) of AR nuclear positivity for each treatment (0 and 10 nM) of DHT
To determine the effect of an altered AR/SGTA ratio on AR subcellular localization in an ovarian context, OVCAR3 cells were transfected with SGTA-specific or nonspecific control siRNA (siSGTA or siN.S., respectively) and treated with or without 10 nM DHT. Under control conditions (siN.S.), SGTA and AR were predominantly localized in the cytoplasm and treatment with DHT induced nuclear translocation of the AR (Fig. 1b, left panels). However, in cells transfected with siSGTA, SGTA protein levels were significantly reduced compared with siN.S. control-treated cells, and this corresponded with an increased level of nuclear AR in the absence and presence of hormone (Fig. 1b, right panels). Quantification of the percentage of AR-positive nuclei revealed that in both the presence and absence of DHT, the percentage of AR-positive nuclei was significantly increased following reduction of SGTA protein (Fig. 1c; Mann–Whitney U test, in both cases p ≤ 0.001). SGTA knockdown increased AR-positive nuclei by 2.9-fold under basal and by 1.9-fold under androgen-stimulated conditions. These data are consistent with the ability of SGTA to restrain nuclear translocation of AR in an ovarian context.
AR and SGTA Immunostaining in Serous Epithelial Ovarian Cancers
AR and SGTA were both expressed in benign and malignant epithelia of ovarian lesions (Fig. 2a). Of the 55 malignant and 15 benign tumors, the majority demonstrated moderate to strong staining for AR and SGTA, with less than 5 % of samples presenting with extremely weak positive staining for either antigen. As expected, immunoreactive AR was observed in the cytoplasm and nucleus of the epithelial compartments of the cancers at all stages and in all borderline and benign tumors. In contrast, only nuclear AR immunoreactivity was observed in stromal cells. As observed in the prostate, immunoreactive SGTA was predominantly evident in the cytoplasmic compartment of epithelial cells and was absent in stromal fibroblasts. The few SGTA-positive cells observed within the stroma have a rounded appearance and are very likely to be invading cancer cells (Fig. 2a, black arrows); however, this requires confirmation by assessing the ability of SGTA to co-localize with an epithelial protein marker, such as cytokeratin. The presence of cytoplasmic AR in ovarian epithelial cells that also contained cytoplasmic SGTA is consistent with the ascribed ability of SGTA to restrain nuclear entry of the AR [4]. This is further supported by the lack of cytoplasmic AR in stromal fibroblasts that lack SGTA and display only nuclear localization of AR.
Immunohistochemical staining of AR and SGTA in serous epithelial benign and ovarian cancer samples. Images (×400 magnification) are representative examples from individual patient samples that correspond to AR (left) and SGTA (right) immunostaining in the epithelium of a malignant tumors (early and late stages), borderline tumors, and benign disease and b primary and matched metastatic tissues from an individual patient. Black arrowheads indicate epithelial cells that have invaded the stroma and are positive for SGTA in the cytoplasm
Comparison of Nuclear AR and SGTA Levels in Ovarian Tumors
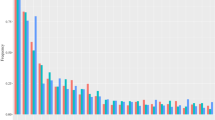
Total cellular and nuclear specific AR immunostaining was measured across the ovarian tissue groups. Since the statistical comparisons were qualitatively similar with either measurement, for simplicity only nuclear AR data are presented below for the AR and AR/SGTA ratio analyses. Nuclear AR levels were significantly different between the ovarian tissue groups (Fig. 3a; p = 0.001, Kruskal–Wallis test). Post-hoc analysis revealed that nuclear AR levels in early- and late-stage malignant tumors were significantly lower compared with levels in benign ovarian tumors (Mann–Whitney U test, in both cases p ≤ 0.001). In addition, nuclear AR levels in late-stage serous tumors were significantly lower compared with borderline serous tumors (Mann–Whitney U test, p = 0.029). However, nuclear AR levels were not different between the two nonmalignant groups or the two malignant groups (Mann–Whitney U test, p = 0.095 and 0.240, respectively). The median SGTA level across the four tissue groups was relatively constant (Fig. 3b), and no significant differences were observed among the different tissue groups (p = 0.635, Kruskal–Wallis test).
Quantitation of nuclear AR and SGTA levels in malignant versus benign disease. MIOD levels for a nuclear AR and b SGTA in benign, borderline, early stage, and late stage of ovarian cancer. Box plots show the median MIOD level (horizontal line), the 25th and 75th percentiles (box), 10th and 90th percentiles (whiskers), and outliers (dots). AR levels were significantly lower in early and late stages tumors compared with benign tumors (in both cases, p = ≤ 0.001). AR levels in late-stage tumors were also significantly lower compared with borderline (p = 0.029). Nuclear AR and SGTA were significantly correlated in c all samples and (d) individually for borderline, early-stage, and late-stage tumors (Spearman’s correlation, r = 0.800, p = 0.010; r = 0.713, p ≤ 0.001; and r = 0.832, p ≤ 0.001, respectively) but not benign (r = 0.555, p = 0.077). The nuclear AR/SGTA ratio was calculated for each sample and is represented in (e). Early- and late-stage tumors as well as borderline tumors had a significantly lower nuclear AR/SGTA ratio compared with benign (p ≤ 0.001, ≤0.001, and 0.015, respectively). The nuclear AR/SGTA ratio in late-stage tumors was also significantly lower compared with borderline (p = 0.043). a Significant compared with benign. b Significant compared with borderline
The levels of AR and SGTA were found to be positively correlated within ovarian tissues (Fig. 3c; r = 0.735 and p ≤ 0.001), which further supports a potential biological relationship between AR and SGTA. This correlation remained significant when borderline, early- and late-stage cancer groups were analyzed individually (Fig. 3d; r = 0.800, p = 0.010; r = 0.713, p ≤ 0.001; and r = 0.832, p ≤ 0.001, respectively) but was a trend in benign tumors (r = 0.555, p = 0.077). To assess the relationship between AR and SGTA in the cohorts, the AR/SGTA ratio was calculated for each individual patient sample. Early- and late-stage malignant serous tumors as well as borderline serous tumors had significantly lower AR/SGTA ratios compared with the benign tumor group (Fig. 3e; Mann–Whitney U test, p = ≤ 0.001, and ≤0.001, 0.015, respectively). Since an increased AR/SGTA ratio induced by SGTA knockdown in OVCAR3 cells resulted in higher levels of AR in nucleus, a reduced AR/SGTA ratio would theoretically lead to less nuclear localization of AR in tumor cells. In support of this concept, the ratio of nuclear AR/total cellular AR expression was also significantly reduced in both malignant groups and borderline tumors compared with benign tumors (Fig. 5a; Mann–Whitney U test, p = 0.002, ≤0.001, and 0.006, respectively).
Comparison of AR and SGTA Levels in Matched Primary and Metastatic Cancers
Representative images of AR and SGTA in the matched primary and metastatic ovarian tumor samples are depicted in Fig. 2b. Similar to sample set 1, nuclear AR and SGTA levels tended toward correlation in primary and were significantly correlated in metastatic disease (Fig. 4c; r = 0.405, p = 0.085 and r = 0.637, p = 0.003, respectively). However, no significant differences in levels of nuclear AR, SGTA, or the AR/SGTA ratio were found between primary and metastatic tumors (Fig. 4a, b, and d). Furthermore, no significant difference was found in the ratios of nuclear to total AR in primary versus metastatic tumors (Fig. 5b).
Quantitation of AR and SGTA levels in primary and matched metastatic ovarian disease. MIOD levels of a nuclear AR and b SGTA in primary and metastatic ovarian cancer. The nuclear AR levels were not significantly different between primary and metastatic samples (Mann–Whitney U test, p = 0.439). Nuclear AR and SGTA were significantly correlated in the c whole set and d metastatic subgroup (r = 0.559, p ≤ 0.001 and r = 0.637, p = 0.003, respectively) but not primary alone (r = 0.405, p = 0.085). e The nuclear AR/SGTA ratio was calculated for each sample, but no significant difference was observed between primary and metastatic cancer (Mann–Whitney U test, p = 0.630)
The ratio of nuclear AR/total AR in primary and metastatic ovarian cancer lesions. a The nuclear AR/total AR ratio was significantly lower in borderline, early-stage, and late-stage tumors compared with benign tumors (p = 0.006, 0.002, and ≤0.001, respectively). b The nuclear AR/total AR ratio was not altered between primary and metastatic tumors (Mann–Whitney U test, p = 0.287)
Discussion
There is growing evidence for a role of AR signaling in ovarian carcinogenesis. However, despite AR being detected in over 90 % of ovarian tumors, few studies have investigated if AR levels are altered at different stages of primary cancer or in primary versus a metastatic disease state. In addition, modulators of AR action such as the co-chaperone SGTA have not previously been assessed with respect to ovarian carcinogenesis. Herein, we observed moderate to strong SGTA expression in the epithelial compartment of benign and malignant ovarian tissues, and in two epithelial ovarian cancer cell lines, which represents the first report of SGTA expression in an ovarian cancer context. SGTA restrained nuclear entry of the AR in an AR-positive serous ovarian cancer cell line, similar to what has been observed in a prostate cancer cell line [4]. Cytoplasmic AR was only evident in SGTA-positive ovarian epithelia, which supports the concept that SGTA can play a role in controlling intracellular movement of AR in benign or malignant ovarian epithelial cells in vivo. The ratio of AR/SGTA was generally lower in ovarian cancers compared with nonmalignant ovarian tissues, the opposite to what has been observed in a prostate context [4]. While SGTA plays a role in restricting AR nuclear localization in ovarian cancer cells, its expression does not appear to differ among disease states, indicating that the in vivo influence of this protein depends on the relative level of AR in the tissue. Collectively, these findings suggest that an attenuation of AR expression and nuclear localization is associated with a malignant status of ovarian epithelial cells.
Our observation that AR levels were significantly lower in malignant compared with non-malignant ovarian tumors was consistent with a study by Cardillo et al. [6] that reported a similar, but nonsignificant, reduction of AR in malignant compared with nonmalignant ovarian tumors. In the latter study, benign and borderline tumors were pooled into one nonmalignant group, but we kept these as separate comparative variables as they are different disease entities. We did not find any differences between these two groups of benign lesions with respect to AR and SGTA when analyzed as separate variables, but the AR/SGTA ratio was significantly reduced in the borderline compared with benign tumors, indicating that AR signaling may play a role in distinguishing these two disease entities. A low AR/SGTA ratio may influence AR subcellular localization in borderline tumors and thereby alter AR transcriptional activity, but this requires further investigation. Based on current clinicopathological and molecular genetic analyses, low- and high-grade serous carcinomas have two distinct pathways of disease progression and borderline tumors are considered precursors of low grade ovarian carcinomas [16, 17, 26, 34]. As very few low-grade serous ovarian carcinomas are detected clinically we were unable to acquire sufficient numbers to determine whether alterations in the AR/SGTA ratio are evident in progression from a borderline lesion to a low-grade serous carcinoma.
The various stages of ovarian cancer denote different states of disease spread whereby the early stages (I/II) are characterized by disease confined to the ovary and pelvic organs, while the late stages (III/IV) involve metastases in the peritoneum, lymph nodes, or organs distant to the peritoneal cavity. Collectively, the data from both clinical cohorts indicate that the parameters of AR signaling that we measured do not appear to be altered during different stages of disease spread, including progression from organ confined to a metastatic disease state. However, it is interesting that both OVCAR3 and SKOV3 ovarian cancer cell lines expressed SGTA but only OVCAR3 possessed AR expression. While both are metastatic derivatives, SKOV3 cells have a more aggressive phenotype than OVCAR3 cells [36] and a differential sensitivity to the chemotoxic agent cisplatin [20]. A limitation of our study is that we were unable to examine the influence of AR, SGTA or the AR/SGTA ratio on patient outcome due to the small cohort size. However, it is feasible that these variables influence ovarian tumor responses to therapeutic treatments, as AR expression has been shown to influence response to chemotherapy in breast cancer [7, 21]. Like ovarian cancer, the AR is frequently expressed in breast cancers and high AR expression is predictive of better survival outcomes [13].
An increased number of AR-positive nuclei were observed in OVCAR3 cells following knockdown of SGTA protein under both basal and androgen stimulated conditions. In effect, the knockdown increased the AR/SGTA ratio. By comparison, the malignant and borderline clinical samples investigated herein had a reduced AR/SGTA ratio compared with benign samples, which should theoretically be associated with a reduced potential for AR nuclear localization. In support of this concept, the ratio of nuclear AR to total cellular AR was significantly decreased in the malignant and borderline samples compared with the benign samples, suggesting that the lower AR/SGTA ratio resulted in increased retention of AR in the cytoplasm. Buchanan et al. [4] showed that decreasing the AR/SGTA protein ratio in the prostate cancer cell line, PC3, decreased both the basal and ligand-induced transcriptional activity of the AR. Whether a reduced AR/SGTA ratio attenuates AR transcriptional activity in ovarian cancer tissues remains to be determined. We attempted to identify a marker of this activity in the OVCAR3 cell line via analyses of candidate AR-regulated genes based on our work in breast and prostate cancer cell lines, but this proved unsuccessful and ovary specific markers of AR activity need yet to be identified, preferably via genome-wide transcriptional analyses.
In conclusion, these data have increased knowledge of AR and SGTA expression in ovarian carcinogenesis and highlighted the need for further investigation of AR signaling in female endocrine-related cancers, particularly as potential biomarkers of chemotherapeutic response or as therapeutic targets.
References
Ahonen MH, Zhuang YH, Aine R, Ylikomi T, Tuohimaa P (2000) Androgen receptor and vitamin D receptor in human ovarian cancer: growth stimulation and inhibition by ligands. Int J Cancer 86(1):40–46
Auersperg N, Edelson MI, Mok SC, Johnson SW, Hamilton TC (1998) The biology of ovarian cancer. Semin Oncol 25(3):281–304
Benedet JL, Bender H, Jones H 3rd, Ngan HY, Pecorelli S (2000) FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet 70(2):209–262
Buchanan G, Ricciardelli C, Harris JM, Prescott J, Zoe Chiao-Li Y, Jia L, Butler LM et al (2007) Control of androgen receptor signaling in prostate cancer by the cochaperone small glutamine rich tetratricopeptide repeat containing protein {alpha}. Cancer Res 67(20):10087–10096
Cannistra SA (2004) Cancer of the ovary. N Engl J Med 351(24):2519–2529
Cardillo MR, Petrangeli E, Aliotta N, Salvatori L, Ravenna L, Chang C, Castagna G (1998) Androgen receptors in ovarian tumors: correlation with oestrogen and progesterone receptors in an immunohistochemical and semiquantitative image analysis study. J Exp Clin Cancer Res 17(2):231–237
Castellano I, Allia E, Accortanzo V, Vandone AM, Chiusa L, Arisio R, Durando A et al (2010) Androgen receptor expression is a significant prognostic factor in estrogen receptor positive breast cancers. Breast Cancer Res Treat 124(3):607–617. doi:10.1007/s10549-010-0761-y
Chadha S, Rao BR, Slotman BJ, van Vroonhoven CC, van der Kwast TH (1993) An immunohistochemical evaluation of androgen and progesterone receptors in ovarian tumors. Hum Pathol 24(1):90–95
Cottreau CM, Ness RB, Modugno F, Allen GO, Goodman MT (2003) Endometriosis and its treatment with danazol or lupron in relation to ovarian cancer. Clin Cancer Res 9(14):5142–5144
Dizon DS, Tejada-Berges T, Koelliker S, Steinhoff M, Granai CO (2006) Ovarian cancer associated with testosterone supplementation in a female-to-male transsexual patient. Gynecol Obstet Invest 62(4):226–228
Evangelou A, Jindal SK, Brown TJ, Letarte M (2000) Down-regulation of transforming growth factor beta receptors by androgen in ovarian cancer cells. Cancer Res 60(4):929–935
Hage JJ, Dekker JJ, Karim RB, Verheijen RH, Bloemena E (2000) Ovarian cancer in female-to-male transsexuals: report of two cases. Gynecol Oncol 76(3):413–415
Hickey TE, Robinson JL, Carroll JS, Tilley WD (2012) Minireview: the androgen receptor in breast tissues: growth inhibitor, tumor suppressor, oncogene? Mol Endocrinol 26(8):1252–1267. doi:10.1210/me.2012-1107me.2012-1107
Ilekis JV, Connor JP, Prins GS, Ferrer K, Niederberger C, Scoccia B (1997) Expression of epidermal growth factor and androgen receptors in ovarian cancer. Gynecol Oncol 66(2):250–254. doi:10.1006/gyno.1997.4764
Kuhnel R, Delemarre JF, Rao BR, Stolk JG (1987) Correlation of multiple steroid receptors with histological type and grade in human ovarian cancer. Int J Gynecol Pathol 6(3):248–256
Kurman RJ, McConnell TG (2010) Precursors of endometrial and ovarian carcinoma. Virchows Arch 456(1):1–12. doi:10.1007/s00428-009-0824-9
Kurman RJ, Shih Ie M (2011) Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer—shifting the paradigm. Hum Pathol 42(7):918–931. doi:10.1016/j.humpath.2011.03.003
Lau KM, Mok SC, Ho SM (1999) Expression of human estrogen receptor-alpha and -beta, progesterone receptor, and androgen receptor mRNA in normal and malignant ovarian epithelial cells. Proc Natl Acad Sci USA 96(10):5722–5727
Lee P, Rosen DG, Zhu C, Silva EG, Liu J (2005) Expression of progesterone receptor is a favorable prognostic marker in ovarian cancer. Gynecol Oncol 96(3):671–677. doi:10.1016/j.ygyno.2004.11.010
Leong CT, Ong CK, Tay SK, Huynh H (2007) Silencing expression of UO-44 (CUZD1) using small interfering RNA sensitizes human ovarian cancer cells to cisplatin in vitro. Oncogene 26(6):870–880. doi:10.1038/sj.onc.1209836
Loibl S, Muller BM, von Minckwitz G, Schwabe M, Roller M, Darb-Esfahani S, Ataseven B et al (2011) Androgen receptor expression in primary breast cancer and its predictive and prognostic value in patients treated with neoadjuvant chemotherapy. Breast Cancer Res Treat 130(2):477–487. doi:10.1007/s10549-011-1715-8
Mangelsdorf DJ, Thummel C, Beato M, Herrlich P, Schütz G, Umesono K, Blumberg B et al (1995) The nuclear receptor superfamily: the second decade. Cell 83(6):835–839
Nodin B, Zendehrokh N, Brandstedt J, Nilsson E, Manjer J, Brennan DJ, Jirstrom K (2010) Increased androgen receptor expression in serous carcinoma of the ovary is associated with an improved survival. J Ovarian Res 3:14. doi:10.1186/1757-2215-3-14
Papadatos-Pastos D, Dedes KJ, de Bono JS, Kaye SB (2011) Revisiting the role of antiandrogen strategies in ovarian cancer. Oncologist 16(10):1413–1421. doi:10.1634/theoncologist.2011-0164theoncologist.2011-0164
Prescott J, Coetzee GA (2006) Molecular chaperones throughout the life cycle of the androgen receptor. Cancer Lett 231(1):12–19
Ricciardelli C, Oehler MK (2009) Diverse molecular pathways in ovarian cancer and their clinical significance. Maturitas 62(3):270–275. doi:10.1016/j.maturitas.2009.01.001
Schildkraut JM, Schwingl PJ, Bastos E, Evanoff A, Hughes C (1996) Epithelial ovarian cancer risk among women with polycystic ovary syndrome. Obstet Gynecol 88(4 Pt 1):554–559
Scully RE (1995) Pathology of ovarian cancer precursors. J Cell Biochem Suppl 23:208–218
Sheach LA, Adeney EM, Kucukmetin A, Wilkinson SJ, Fisher AD, Elattar A, Robson CN, Edmondson RJ (2009) Androgen-related expression of G-proteins in ovarian cancer. Br J Cancer 101(3):498–503. doi:10.1038/sj.bjc.6605153
Silva EG et al (1997) The induction of benign epithelial neoplasms of the ovaries of guinea pigs by testosterone stimulation: a potential animal model. Mod Pathol 10(9):879–883
Slotman BJ, Kuhnel R, Rao BR, Dijkhuizen GH, de Graaff J, Stolk JG (1989) Importance of steroid receptors and aromatase activity in the prognosis of ovarian cancer: high tumor progesterone receptor levels correlate with longer survival. Gynecol Oncol 33(1):76–81. doi:0090-8258(89)90607-0
Tilley WD, Lim-Tio SS, Horsfall DJ, Aspinall JO, Marshall VR, Skinner JM (1994) Detection of discrete androgen receptor epitopes in prostate cancer by immunostaining: measurement by color video image analysis. Cancer Res 54(15):4096–4102
van Doorn HC, Burger CW, van der Valk P, Bonfrer HM (2000) Oestrogen, progesterone, and androgen receptors in ovarian neoplasia: correlation between immunohistochemical and biochemical receptor analyses. J Clin Pathol 53(3):201–205
Vang R, Shih Ie M, Kurman RJ (2009) Ovarian low-grade and high-grade serous carcinoma: pathogenesis, clinicopathologic and molecular biologic features, and diagnostic problems. Adv Anat Pathol 16(5):267–282. doi:10.1097/PAP.0b013e3181b4fffa00125480-200909000-00001
Wang Y, Yang J, Gao Y, Dong LJ, Liu S, Yao Z (2007) Reciprocal regulation of 5alpha-dihydrotestosterone, interleukin-6 and interleukin-8 during proliferation of epithelial ovarian carcinoma. Cancer Biol Ther 6(6):864–871
Ween MP, Lokman NA, Hoffmann P, Rodgers RJ, Ricciardelli C, Oehler MK (2011) Transforming growth factor-beta-induced protein secreted by peritoneal cells increases the metastatic potential of ovarian cancer cells. Int J Cancer 128(7):1570–1584. doi:10.1002/ijc.25494
Wiegratz I, Jung-Hoffmann C, Kuhl H (1995) Effect of two oral contraceptives containing ethinylestradiol and gestodene or norgestimate upon androgen parameters and serum binding proteins. Contraception 51(6):341–346
Acknowledgments
The authors thank Helen Hughes for collection of archival tissue blocks, Dr. Shalini Jindal for assessment of pathology, and Dr. Aleksandra Ochnick for TMA construction. This study was supported by funds from the National Health and Medical Research Committee of Australia via a postdoctoral fellowship to TEH (No. 465428) and a project grant to WDT and TEH (No. 453628).
Conflict of Interest
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Butler, M.S., Ricciardelli, C., Tilley, W.D. et al. Androgen Receptor Protein Levels Are Significantly Reduced in Serous Ovarian Carcinomas Compared with Benign or Borderline Disease but Are Not altered by Cancer Stage or Metastatic Progression. HORM CANC 4, 154–164 (2013). https://doi.org/10.1007/s12672-013-0135-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-013-0135-0