Abstract
Background
Severe acute pancreatitis (SAP) is a disease with high morbidity and mortality. We undertook a study of patients with SAP admitted to the intensive care unit (ICU) of a tertiary referral hospital.
Methods
Between 2002 and 2007, 50 patients with SAP were admitted in our intensive care unit (ICU). Data were collected from their medical records and their clinical profile, course and outcome were retrospectively analyzed. Patients were categorized into survivor and nonsurvivor groups, and were further classified based on interventions such as percutaneous drainage and surgical necrosectomy.
Results
SAP contributed 5 % of total ICU admissions during the study period. Median age of survivors (n = 20) was 34 against 44 years in nonsurvivors (n = 30). Median Acute Physiology and Chronic Health Evaluation (APACHE) II score in nonsurvivors was 16.5 (8–32) vs. 12.5 (5–20) in survivors (p = 0.002). Patients with APACHE II score ≥12 had mortality >80 % compared to 23 % with score <12 (p < 0.001). Median Sequential Organ Failure Assessment (SOFA) scores on admission and on days 3, 7, 14, and 21 were significantly higher in nonsurvivors compared to survivors (p < 0.05). Mean (SD) intraabdominal pressure was 23 (3.37) mmHg in nonsurvivors vs. 19.05 (2.51) in survivors (p < 0.05). Patients with renal failure had significant mortality (p < 0.001). Length of ICU stay, requirement for vasopressor, total parenteral nutrition, and the amount of blood and blood product transfusions differed significantly between patients with and without intervention.
Conclusions
APACHE II and SOFA scores and other clinical data correlated with outcome in SAP admitted to ICU.
Similar content being viewed by others
Introduction
Acute pancreatitis (AP) in 80 % patients is a mild self-limiting disease that may require brief hospitalization [1]. However, 20 % patients may develop a severe form, characterized by multiple organ dysfunction [1], unpredictable course, and associated complications, which warrant an admission to intensive care unit (ICU).
In this 5-year audit, we outline the demography, etiology, prognostic indices, severity, outcome, and interventions required for the management of severe AP (SAP) in a tertiary care medical surgical ICU, highlighting the resource-intensive nature of this catastrophic illness.
Methods
Data collection
Data were collected from the medical records of the ICU of a tertiary care referral hospital in North India from 2002 to 2007, after prior approval from the Institute’s ethics committee. We identified 50 consecutive patients with SAP out of the 1,015 patients admitted to our ICU during this period. Data from individual case records included age, sex, comorbid illness, etiology, and the duration of SAP. Admission variables included vitals (heart rate, respiratory rate, temperature, blood pressure) and urine output. Severity ICU scores calculated were Acute Physiology and Chronic Health Evaluation (APACHE) II and Sequential Organ Failure Assessment (SOFA). Hematology, chemistry, coagulation, arterial blood gas, and lactate levels were the relevant laboratory variables measured. Computed tomographic images for the assessment of necrosis and collections were retrieved. Data regarding therapeutic interventions during the ICU stay included fluid resuscitation (first 72 h), vasopressor use, mechanical ventilation, renal replacement therapy (RRT), mode of delivery and type of nutrition, percutaneous drainage (PCD), and surgical necrosectomy. The course of illness and outcome measures of discharge or death from ICU were noted.
Definitions
Patients of AP associated with organ failure and/or local complications such as necrosis, abscess, or pseudocyst were considered to have SAP as per the Atlanta criteria [2]. Severity assessment was done by APACHE II score [3], SOFA score [4], and computed tomographic necrosis. Systemic inflammatory response syndrome (SIRS) was assessed as per the standard definition [5]. Organ dysfunction was defined according to the recommendations of the consensus conference of American College of Chest Physicians/Society of Critical Care Medicine in 1991 [6].
Management
All patients admitted to the ICU were monitored hemodynamically with invasive arterial, central venous catheterization and in some with pulmonary artery catheter (PAC). Contrast-enhanced computed tomography (CECT) was done to confirm and/or stage the pancreatitis and for any planned diagnostic, radiological, or surgical intervention, usually following clinical deterioration. It was done routinely in all patients within the first 2 weeks of SAP, unless contraindicated or if it was already available prior to the ICU admission. All patients had nasogastric tubes or nasojejunal tubes for the administration of enteral nutrition (EN). Organ-supportive measures such as mechanical invasive ventilation for respiratory failure and RRT for acute kidney injury (AKI) were instituted whenever required. Patients requiring prolonged ventilation (>7 days) underwent percutaneous dilatation tracheostomy.
Categorization of study population
Elective ICU admissions were defined as patients from within the hospital who had at least once been reviewed by our critical care outreach team before being transferred to our ICU, while patients from within or outside our hospital who were received by our ICU without prior review by our outreach team or were brought in a state of emergency (pulse less and/or gasping) were considered as emergency admissions. All patients were grouped into survivors and nonsurvivors and were further classified into intervention and nonintervention groups. Patients who underwent either PCD or surgical necrosectomy were included in the intervention group, while the remaining patients were considered under the nonintervention group.
Statistical analysis
Data were expressed as mean (SD) or median or percentage. Continuous data were compared using the paired t test while parametric data were compared using the chi square test; a p-value of <0.05 was considered significant. Statistical analysis was done with the SPSS (Inc., Chicago, IL, USA) version 14 for windows.
Results
Demographics and mortality
SAP accounted for 50 of 1,015 (approximately 5 %) admissions during the study period. Of these, 30 patients (60 %) succumbed to the illness. The demography, etiology, comorbidities, day of onset of SAP at the time of ICU admission, and the duration of ICU stay were similar among survivors and nonsurvivors (Table 1). Mortality among elective admissions was 53 % (20/38) compared to 83 % (10/12) among emergency admissions. Ten of 30 (33 %) deaths occurred early (before 2 weeks) and 20 (66.7 %) occurred late (beyond 2 weeks).
Organ dysfunction and prognostication scores
Organ involvement at admission, either dysfunction (SOFA 1–2) or failure (SOFA 3–4), was found in decreasing order as follows: respiratory (62 %), cardiovascular (52 %), renal (38 %), coagulation (12 %), hepatic (4 %), and neurological (4 %). All patients had multiorgan dysfunction or failure during their ICU stay. Higher mortality was observed in patients who had renal involvement; 56.3 % (17/30) vs. 10 % (2/20) in survivors (p = 0.001) (Table 1). Renal dysfunction and the requirement of dialysis was observed in 57 % of nonsurvivors as against 10 % of survivors (p < 0.001). RRT, either intermittent hemodialysis (IHD) or continuous renal replacement therapy (CRRT), was used depending upon the clinical status of the patient. Continuous veno venous hemodialysis (CVVHD) was the preferred modality of RRT. Mechanical invasive ventilation was used in 90 % (45/50) of our patients; 75 % (15/20) of survivors and 100 % (30/30) of nonsurvivors required this type of ventilation. Noninvasive ventilation (NIV) was used in one patient but failed. Ventilation-free days were significantly higher in survivors compared to that in nonsurvivors [10 (1–88) vs. 0 (0–18), respectively; p < 0.001] (Table 1). The median APACHE II score (Table 2) at admission was 12.5 in survivors and 16.5 among nonsurvivors (p = 0.002). This difference remained even at the end of 24 h (p < 0.001). While the APACHE II score decreased by a median of 1 point in survivors, it remained unchanged in nonsurvivors (p = 0.037). APACHE II score of ≥12 at admission was associated with mortality of 78 % as against 27.7 % in those with scores <12 (p < 0.001) (Table 2). Median SOFA scores on admission and serial median SOFA scores were higher in nonsurvivors (p < 0.05) (Table 2, Fig. 1).
Intraabdominal pressure
From the end of 2006, we had started to measure and monitor intravesical pressure via the Foley’s catheter as a measure of intraabdominal pressure (IAP). Mean IAP (n = 17) on admission and maximum during the ICU stay was significantly higher among nonsurvivors (p < 0.05) (Table 2).
Pancreatic necrosis and infection
CT images could be retrieved in only 36 patients (72 %); of these, computed tomographic necrosis was evident in 30, whereas pancreatic swelling without necrosis was evident in six patients. In eight patients CT images were not available for interpretation, in three, CECT could not be carried out because of progressively deteriorating AKI, and in another three, transportation outside ICU was deemed too unsafe because of severe hemodynamic instability, and these patients succumbed even before a CECT could be undertaken. The number of survivors and nonsurvivors was 2, 4; 5, 2; 0, 7; and 1, 9 in patients with necrosis <30 %, 30 % to 50 %, 50 % to 75 %, and >75 %, respectively (p = 0.010). Sixteen patients out of 22 (72.7 %) nonsurvivors against 1 of 8 (12.5 %) survivors had >50 % necrosis (p < 0.009) (Table 1). Nine of 10 patients with >75 % necrosis (90 %) died compared to 4 of 6 (66.6 %) with <30 % necrosis.
The intervention radiologist conducted the diagnostic and or therapeutic drainage under the guidance of ultrasonography (USG) and/or CT in patients with evidence of pancreatic or extra-pancreatic collections. Culture of these samples and those obtained during necrosectomy along with percutaneous drain (PCD) cultures of the first 24 h were the only ones considered for analysis during this study. Infected (culture positive) necrosis was present in 25 of the 30 (84.5 %) patients with evidence of necrosis. Nineteen among the 25 with infected necrosis succumbed to their illness (p = 0.59). The isolates were of Escherichia coli (23.3 %), Pseudomonas (21.9 %), Enterococcus (20.5 %), Acinetobacter (12.3 %), Citrobacter (12.3 %), and Klebsiella (9.6 %). Fungus was not isolated from any of the samples.
Fluid resuscitation and vasopressors
Initial fluid resuscitation was with crystalloids (normal saline, ringer lactate) or colloid (20 % albumin) to maintain hemodynamics and urine output >0.5 mL kg−1 h−1. If hemodynamic instability persisted despite fluid resuscitation, the administration of vasoactive drugs such as nor-adrenaline was initiated. The requirement of initial fluid resuscitation (first 72 h) was significantly higher among nonsurvivors as compared to survivors (8.0 ± 4.0 vs. 5.3 ± 4.0; p = 0.013). All nonsurvivors required nor-adrenaline, as against 5 out of 20 (25 %) survivors. Higher dose of nor-adrenaline (>1.5 μgm kg−1 min−1) was required only among the nonsurvivors (p < 0.001).
Nutrition
Initially, the nutritional support was enteral through a nasogastric (NG) or nasojejunal (NJ) tube unless feed intolerance (defined as ≥1 gastric residual volume of ≥250 mL) was observed whereby total parenteral nutrition (TPN) was commenced. Feeding jejunostomy (FJ) was preferred for patients undergoing necrosectomy, but the decision was left to the discretion of the gastro-surgeon. TPN was used in nonsurvivors for a median of 9 (1–29) days vs. 4 (2–12) days in survivors (p = 0.003). Eighty percent (40/50) of our patients required both enteral and parenteral support. EN or TPN was used alone in 14 % and 6 % patients, respectively. EN was given via NG tube in 42 % and NJ tube in 37 % while 21 % required both. Four patients had feeding jejunostomy performed during surgical necrosectomy.
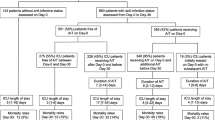
Percutaneous and surgical interventions
USG- or CT-guided fine needle aspiration (FNA) or percutaneous drainage (PCD) of pancreatic or peripancreatic collection with relevant cultures was done in patients who either developed a new worsening or did not show progressive improvement in their clinical condition. Multiple PCD catheters, each with a minimum diameter of 12–14 French and multiple side ports were inserted by Seldinger technique. Up sizing, repositioning or reinsertion of PCDs was done by serial dilatation as and when required. Catheters were flushed daily with saline, 8–12 hourly. Surgical necrosectomy was done if deterioration in clinical course occurred despite repositioning, replacement, up sizing or placement of a new PCD, and other conservative supportive management. The categorization of patients on the basis of interventions is schematically represented in Fig. 2. Thirty-two (64 %) patients required intervention, of which PCD or surgery alone was sufficient in 34.4 % (11/32) and 28.1 % (9/32), respectively. Both PCD and surgery were required in 37.5 % (12/32) patients. Significantly higher percentage of patients with CT necrosis ≥50 % required interventions. Patients who underwent intervention required a longer duration of vasopressor support (median 10 vs. 6.5 days; p = 0.026) and parenteral nutrition [8.5 (1–29) vs. 4 (1–12) days; p = 0.008] (Table 3). Mortality was 75 % (24/32) in the intervention group as against 33.3 % (6/18) in the nonintervention group (p = 0.04). Demography, etiology, severity scores, fluid resuscitation in the first 24 h, and days of EN were similar in both the groups (Table 3). Transfusion requirements were also documented for the study population. The intervention group required a median of 36 (2–259) units of transfusions as against 9 (1–66) in the nonintervention group (p = 0.004); among the blood products, this difference achieved significance for packed red blood cells (PRBCs), random donor platelet (RDP), and fresh frozen plasma (FFP) (Table 3). Bleeding occurred as a result of underlying coagulopathy or as a result of interventions. Bleeding as a complication of PCD was minimal and easily controllable. However, in three patients, digital subtraction angiography (DSA) had to be done as minimal bleeding persisted despite correction of coagulopathy. Bleeding further increased after necrosectomy, and it caused hemodynamic instability in five patients, of which three had to be re-explored and in two DSA along with instillation of anticoagulant substance was done to stop the bleeding. The requirement for transfusion was similar among survivor and nonsurvivors (data not shown).
Discussion
This audit presents the characteristics, prognostication factors, interventions, and outcome of SAP patients admitted to a medical–surgical ICU. APACHE II/SOFA score, the presence of IAH, as well as extent and the presence of infected necrosis were some of the adverse prognostic factors. Multisystem organ failure in SAP contributes to the high morbidity and mortality. The management of SAP in ICU is resource intensive as a result of frequent radiological and/or surgical interventions along with the aggressive organ-support measures needed over prolonged periods.
Demographics and mortality
In this study, SAP accounted for 5 % of admissions as against a study from UK where it contributed to 1.3 % of total ICU admissions [7]. Numerous studies [8, 9] have reported mortality rate of SAP from 16.3 % to 53.6 %. In our study mortality rate was 60 %. High mortality in our series is attributed to the severity of illness of patients included, as ours is a referral hospital. Considerable variation exists with regard to the timing of death [10, 11]. Early deaths are generally attributed to organ failure, while late deaths are usually caused by infected necrosis or complications of sterile necrosis. A majority of deaths in our study were in the late period, as reported [12, 13] in other studies too. Gallstones and alcohol contributed equally as the etiology in our patients, similar to other studies [14, 15]. As in previous studies [16, 17], gender and etiology had no prognostic significance.
Organ dysfunction and prognostication scores
Patients with organ failure at admission have a higher mortality than those without it [12, 13, 18, 19]. The development of organ failure during ICU stay is also associated with a similar or higher mortality [12, 13, 18, 19]. Both multisystem organ failure [18] and sustained organ failure (lasting more than 48 h) [12] have the highest mortalities (≥36 %). The mortality in the absence of organ failure is nil [18], with single organ failure it is 3 % (range 0–8) [13, 18], while with multisystem organ failure it is 47 % (range 28 % to 69 %) [5, 13, 18], as was also found in our study. Pulmonary dysfunction is a major component of multiorgan failure and contributes to early mortality in patients with SAP [8]. Respiratory dysfunction was the most frequent systemic complication, similar to the study that reviewed the evolution of AP cases in ICU [20]. Mechanical lung ventilation was required in 90 % of our patients. Lung protective mechanical ventilation strategy was utilized for all patients in respiratory failure. Reported incidence of acute renal failure (ARF) in AP is up to 42 % [21], with a mortality of 50 % [22]. However, in SAP it is as high as 81 % [23, 24] as against 90 % observed in our study.
The assessment of severity in SAP often utilizes APACHE II [3] and SOFA [25] scores. In our study we found a significantly higher APACHE II score among nonsurvivors, both at admission and after 24 h, similar to other studies [12, 16, 25–29]. A study comparing prognostic scores in AP reported that APACHE II generated within the first 24 h had a positive predictive value of only 43 % and negative predictive value of 86 % for SAP as compared to the 48 h Ranson score of 48 % and 93 %, respectively [17]. A significant marginal improvement in scores after 24 h in survivors was seen in our study. There was a sharp cutoff at 12 between survival and death. However, the ability of APACHE II score to stratify patients for disease severity is limited. Inability to show sharp cutoff between interstitial and necrotizing pancreatitis, on the one hand, and between sterile and infected necrosis [18], on the other hand, have been reported. In our study, an APACHE II score of ≥12 was a bad prognostic factor.
SOFA score performed better than other severity scores, with additional advantages of easy applicability and timely assessment [25]. In our study, admission SOFA and serial weekly SOFA scores were significantly higher among the nonsurvivors.
Intraabdominal pressure
Recent studies have focused on the role of intraabdominal hypertension (IAH)/abdominal compartment syndrome (ACS) in patients of SAP in ICU [29, 30]. Numerous studies have found an association between IAH and the development of multiple organ dysfunction, leading to higher mortality [19, 31]. IAP was significantly raised in nonsurvivors, similar to another study [32]. Early identification of patients at risk and implementation of preventive strategies can halt progression of IAH to ACS [33]. Incorporation of both operative and nonoperative strategies to reduce IAP improved survival in IAH/ACS [34]. Routine monitoring of IAP in SAP is suggested because of ACS’s prognostic and therapeutic consequences [29]. PCD is indicated in IAH/ACS, but laparotomy with or without laparostomy is to be considered when IAP is ≥20 despite PCD [35].
Pancreatic necrosis and infection
Necrosis and collections are important local complications included in the CT severity index (CTSI) [25]. Though the presence and extent of necrosis are risk factors for disease severity and outcome, they alone are rarely life threatening in the absence of infection or organ failure [36, 37]. Reported mortality in infected necrosis is in the range of 40 % to 70 % while, it was 76 % in our study [38]. Increasing mortality with increasing extent of necrosis observed in our study is as previously reported [39]. Literature regarding correlation between the extent and or presence of infected necrosis with organ failure and mortality [18, 27, 40, 41] is rather conflicting. Studies both in favor and against are well reported.
Escherichia coli were the most common species isolated. The use of antibiotic prophylaxis has favored growth of Gram-positive and fungal organisms like Staphylococcus species and Candida [42, 43]. However, none was isolated in our series. The mortality increases from 5 % to 25 % in sterile necrosis to 15 % to 28 % in presence of infection [44, 45]. Cochrane meta-analysis showed a reduction in mortality with the use of β-lactams, although there was no evidence of a reduction in the pancreatic necrosis infection rate [46]. Though the debate on prophylactic antibiotics in sterile necrotic pancreatitis is still open, a systematic review and meta-analysis concluded that antibiotic prophylaxis is not protective in SAP [42]. Majority of our patients were already on broad-spectrum antibiotics prior to ICU admission. Prophylactic antibiotics (imipenem, piperacilin-tazobactum, cefaperazone-sulbactum, ofloxacin, and teicoplanin) were used in most of the patients, and later modified as per the culture-sensitivity reports.
Fluid resuscitation and vasopressors
Early aggressive fluid management in AP patients results in the resolution of organ failure and reduces associated mortality risk [47]. In experimental studies [48, 49], improved delivery of oxygen has been shown to prevent or minimize pancreatic necrosis and improve survival. Patients exhibiting hemoconcentration at admission and a further rising hematocrit after 24 h developed higher pancreatic necrosis [50]. The nonsurvivors in our study required significantly higher volumes of fluid resuscitation in the first 3 days. Despite aggressive fluid resuscitation refractory organ failure, as indicated by higher requirement of vasopressor support, ventilatory support, and the need for RRT, explains the high mortality in this group.
Nutrition
According to the European Society of Parenteral and Enteral Nutrition (ESPEN) [51], nutritional support is indicated for SAP if intolerant to oral feeds for at least 7 days. This assessment can be made within the first 3–4 days of admission, during which TPN can fulfil the catabolic demands. Scientific evidence exists that EN is superior to TPN [52–55], with beneficial effects on mucosal integrity preventing bacterial overgrowth [56]. Other benefits include reduced risk of infection, surgical interventions, and length of hospital stay [52, 53, 56]. In a systematic review, EN commenced within 48 h of admission significantly reduced multiorgan failure, pancreatic infectious complications, and mortality [53]. However, TPN should be used till EN becomes tolerable [56]. In a meta-analysis no significant mortality benefit was observed between NG and NJ and parenteral feeding [57]. In our study, the median days of TPN use was significantly associated with mortality. Majority of our patients required both enteral and parenteral nutrition; almost equal percentage requiring NG and NJ route for EN.
Percutaneous and surgical interventions
Surgical intervention was initiated beyond the fourth week of illness, as it allows the immune system to demarcate the pancreatic necrosis [58], except in one in whom immediate surgery was required due to ACS. Open necrosectomy with continuous lavage of the lesser sac and retroperitoneum [59] was the commonest approach used in our patients. Nearly two-thirds of patients in the intervention group required surgical necrosectomy, the gold standard treatment for proven infected pancreatic necrosis [60]. Surgery is not advisable in the first 2 weeks even in the presence of multiorgan failure, and postponing it beyond fourth week is favored [61]. PCD as an alternative to surgery [62] was utilized in >70 % patients in the intervention group. Although PCD aided in postponing the surgery beyond fourth week in majority of our patients, >50 % of these patients later required surgical intervention. Similar results have been reported by the Dutch Pancreatitis Study group in their systematic review of PCD [63]. In majority of our patients, multiple PCD catheters, each with a minimum diameter of 12–14 Fr [64] and multiple side ports were used. In most, catheters had to be either upsized, repositioned, or reinserted on more than 2–3 occasions. Contrast-enhanced CT has been considered the “gold standard” for the diagnosis of pancreatic necrosis [65]. A significant number of our patients in the intervention group had necrosis ≥50 %, of which 85 % were infected. They also required prolonged duration of vasopressors, PN, and longer stay in the ICU. Higher mortality in the intervention group in our study is due to higher APACHE II and SOFA scores, and a higher percentage of patients with necrosis >50 %, majority of whom were infected. There was no death because of PCD-induced trauma in our study. The daily flushing in combination with the frequent need for catheter replacement makes PCD an intensive and time-consuming therapy. Deaths occurring after surgical intervention were more often because of profound SIRS with poor organ physiological reserves and secondary infections, rather than bleeding-related complications.
Limitations of the study
The small retrospective audit from a single center is the main limitation of our study. The course and outcome of single vs. multiorgan failure have not been elaborated because of incomplete data recording in the hospital records. Timing of PCD, postponement in surgery because of PCD, catheter-related complications, and surgical intervention details were other information that were missing in a number of the records.
Conclusions
This audit provides a picture of SAP patients admitted to ICU in terms of etiology, severity, outcome, and the factors associated with its mortality and morbidity. The adverse prognostic factors identified were higher APACHE II/SOFA score, the presence of IAH, the presence/extent of infected necrosis, initial aggressive fluid resuscitation, prolonged vasopressor and ventilator support, along with a need for RRT. A large proportion of these patients require PCD and/or surgical interventions. Prolonged duration of ICU stay, vasopressor support, PN, the extent of necrosis, blood transfusions are all significantly associated in the intervention group. SAP is a catastrophic resource-intensive illness, requiring multidisciplinary, extended, and comprehensive support in an intensive care unit.
References
Frossard JL, Steer MI, Pastor CM. Acute pancreatitis. Lancet. 2008;371:143–52.
Bradley EL 3rd. A clinically based classification system for acute pancreatitis. Summary of the international symposium on acute pancreatitis, Atlanta, GA, September 11 through 13, 1992. Arch Surg. 1993;128:586–90.
Knaus WA, Draper EA, Waqner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Halonen KI, Pettila V, Leppaniemi AK, et al. Multiple organ dysfunction associated with severe acute pancreatitis. Crit Care Med. 2002;30:1274–9.
Rangel-Frausto MS, Pitter D, Costigan M, Hwang T, Davis CS, Wenzel RP. The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study. JAMA. 1995;273:117–23.
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. American college of chest physicians/society of critical care medicine. Chest. 1992;101:1644–55.
Harrison DA, D’Amico G, Singer M. The Pancreatitis Outcome Prediction (POP) score: a new prognostic index for patients with severe acute pancreatitis. Crit Care Med. 2007;35:1703–8.
Pupelis G, Zeiza K, Plaudis H, Suhova A. Conservative approach in the management of severe acute pancreatitis: eight-year experience in a single institution. HPB. 2008;10:347–55.
Bumbasirevic V, Radenkovic D, Jankovic Z, et al. Severe acute pancreatitis: overall and early versus late mortality in intensive care units. Pancreas. 2009;38:122–5.
Company L, Saez J, Martinez J, et al. Factors predicting mortality in severe acute pancreatitis. Pancreatology. 2003;3:144–8.
Ashley SW, Perez A, Pierce EA, et al. Necrotizing pancreatitis: contemporary analysis of 99 consecutive cases. Ann Surg. 2001;234:572–9. discussion 579–80.
Johnson CD, Abu-Hilal M. Persistent organ failure during the first week as a marker of fatal outcome in acute pancreatitis. Gut. 2004;53:1340–4.
McKay CJ, Buter A. Natural history of organ failure in acute pancreatitis. Pancreatology. 2003;3:111–4.
Doley RP, Yadav TD, Wig JD, et al. Enteral nutrition in severe acute pancreatitis. JOP. 2009;10:157–62.
Baig SJ, Rahed A, Sen S. A prospective study of the aetiology, severity and outcome of acute pancreatitis in eastern India. Trop Gastroenterol. 2008;29:20–2.
Rahman SH, Ibrahim K, Larvin M, et al. Association of antioxidant enzyme gene polymorphisms and glutathione status with severe acute pancreatitis. Gastroenterology. 2004;126:1312–22.
Chatzicostas C, Roussomoustakaki M, Vlachonikolis IG, et al. Comparison of Ranson, APACHE II and APACHE III scoring systems in acute pancreatitis. Pancreas. 2002;25:331–5.
Perez A, Whang EE, Brooks DC, et al. Is severity of necrotizing pancreatitis increased in extended necrosis and infected necrosis? Pancreas. 2002;25:229–33.
Buter A, Imrie CW, Carter CR, et al. Dynamic nature of early organ dysfunction determines outcome in acute pancreatitis. Br J Surg. 2002;89:298–302.
Arroyo-Sánchez AS, García Ventura J, Aguirre Mejía RY. Acute pancreatitis in intensive care unit: review and evolution of 36 cases Víctor Lazarte E. Hospital. Trujillo, Perú. Rev Gastroenterol Peru. 2008;28:133–9.
Herrera Gutierrez ME, Seller Perez G, de La Rubia De Gracia C, Chaparro Sanchez MJ, Nacle Lopez B. Acute renal failure profile and prognostic value in severe acute pancreatitis. Med Clin (Barc). 2000;115:721–5.
Zhang XP, Wang L, Zhou YF. The pathogenic mechanism of severe acute pancreatitis complicated with renal injury: a review of current knowledge. Dig Dis Sci. 2008;53:297–306.
Tran DD, Oe PL, de Fijter CWH, Van der Meulen J, Cuesta MA. Acute renal failure in patients with acute pancreatitis: prevalence, risk factors and outcome. Nephrol Dial Transplant. 1993;8:1079–84.
Kes P, Vucicević Z, Ratković-Gusić I, Fotivec A. Acute renal failure complicating severe acute pancreatitis. Nephron. 1996;73:488–9.
Juneja D, Gopal PB, Ravula M. Scoring systems in acute pancreatitis: which one to use in intensive care units? J Crit Care. 2010;25:358.e9–358.e15.
Lankisch PG, Warnecke B, Bruns D, et al. The APACHE II score is unreliable to diagnose necrotizing pancreatitis on admission to hospital. Pancreas. 2002;24:217–22.
Malangoni MA, Martin AS. Outcome of severe acute pancreatitis. Am J Surg. 2005;189:273–7.
Mettu SR, Wig JD, Khullar M, et al. Efficacy of serumnitric oxide level estimation in assessing the severity of necrotizing pancreatitis. Pancreatology. 2003;3:506–13. discussion 513–4.
De Waele JJ, Hoste E, Blot SI, et al. Intra-abdominal hypertension in patients with severe acute pancreatitis. Crit Care. 2005;9:R452–7.
Chen H, Li F, Sun JB, Jia JG. Abdominal compartment syndrome in patients with severe acute pancreatitis in early stage. World J Gastroenterol. 2008;14:3541–8.
Poves Prim I, Fabregat Pous J, Garcia Borobia FJ, et al. Early onset of organ failure is the best predictor of mortality in acute pancreatitis. Rev Esp Enferm Dig. 2004;96:705–9.
Zhang WF, Ni YL, Cai L, Li T, Fang XL, Zhang YT. Intra-abdominal pressure monitoring in predicting outcome of patients with severe acute pancreatitis. Hepatobiliary Pancreat Dis Int. 2007;6:420–3.
Carlotti Ana PCP, Carvalho Werther B. Abdominal compartment syndrome: a review. Pediatr Crit Care Med. 2009;10:115–20.
Cheatham ML, Safcsak K. Is the evolving management of intra-abdominal hypertension and abdominal compartment syndrome improving survival? Crit Care Med. 2010;38:402–7.
Al-Bahrani AZ, Abid GH, Holt A, et al. Clinical relevance of intra-abdominal hypertension in patients with severe acute pancreatitis. Pancreas. 2008;36:39–43.
Buchler MW, Gloor B, Muller CA, et al. Acute necrotizing pancreatitis: treatment strategy according to the status of infection. Ann Surg. 2000;232:619–26.
Rau BM, Bothe A, Kron M, et al. Role of early multisystem organ failure as major risk factor for pancreatic infections and death in severe acute pancreatitis. Clin Gastroenterol Hepatol. 2006;4:1053–61.
Werner J, Ühl W, Büchler MW. Acute pancreatitis. In: Cameron JL, (ed). Current Surgical Therapy, 8th edn. Elsevier Mosby, Philadelphia. 2004; pp. 459–469.
Pitchumoni CS, Patel NM, Shah P. Factor’s influencing mortality in acute pancreatitis: can we alter them? J Clin Gastroenterol. 2005;39:798–814.
Isenmann R, Runzi M, Kron M, et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterology. 2004;126:997–1004.
Gotzinger P, Wamser P, Exner R, et al. Surgical treatment of severe acute pancreatitis: timing of operation is crucial for survival. Surg Infect (Larchmt). 2003;4:205–11.
Jafri NS, Mahid SS, Idstein SR, Hornung CA, Galandiuk S. Antibiotic prophylaxis is not protective in severe acute pancreatitis: a systematic review and meta-analysis. Am J Surg. 2009;197:806–13.
Isenmann R, Schwarz M, Rau B, Trautmann M, Schober W, Beger HG. Characteristics of infection with Candida species in patients with necrotizing pancreatitis. World J Surg. 2002;26:372–6.
Götzinger P, Wamser P, Barlan M, Sautner T, Jakesz R, Függer R. Candida infection of local necrosis in severe acute pancreatitis is associated with increased mortality. Shock. 2000;14:320–3. discussion 323–324.
Rau B, Pralle U, Uhl W, Schoenberg MH, Beger HG. Management of sterile necrosis in instances of severe acute pancreatitis. J Am Coll Surg. 1995;181:279–88.
Villatoro E, Bassi C, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev 4. 2006;CD002941
Working Party of the British Society of Gastroenterology; Association of Surgeons of Great Britain and Ireland; Pancreatic Society of Great Britain and Ireland; Association of Upper GI Surgeons of Great Britain and Ireland. UK guidelines for the management of acute pancreatitis. Gut. 2005;54 Suppl 3:iii1–9.
Isenmann R, Beger HG. Bacterial infection of pancreatic necrosis: role of bacterial translocation, impact of antibiotic treatment. Pancreatology. 2001;1:79–89.
Strate T, Mann O, Kleinhans H, et al. Microcirculatory function and tissue damage is improved after therapeutic injection of bovine hemoglobin in severe acute rodent pancreatitis. Pancreas. 2005;30:254–9.
Brown A, Baillargeon JD, Hughes MD, et al. Can fluid resuscitation prevent pancreatic necrosis in severe acute pancreatitis? Pancreatology. 2002;2:104–7.
Meier R, Ockenga J, Pertkiewicz M, et al. ESPEN guidelines on enteral nutrition: pancreas. Clin Nutr. 2006;25:275–84.
Ioannidis O, Lavrentieva A, Botsios D. Nutrition support in acute pancreatitis. J Pancreas. 2008;9:375–90.
Petrov MS, Pylypchuk RD, Uchugina AF. A systematic review on the timing of artificial nutrition in acute pancreatitis, Br J Nutr. 2009;101:787–93.
Marik PE. What is the best way to feed patients with pancreatitis? Curr Opin Crit Care. 2009;15:131–8.
Ammori BJ. Role of the gut in the course of severe acute pancreatitis. Pancreas. 2003;26:122–9.
Gianotti L, Meier R, Lobo DN, et al. ESPEN guidelines on parenteral nutrition: pancreas. Clin Nutr. 2009;28:428–35.
Jiang K, Chen X-Z, Xia Q, Tang W-F, Wang L. Early nasogastric enteral nutrition for severe acute pancreatitis: a systematic review. World J Gastroenterol. 2007;13:5253–60.
Hartwig W, Werner J, Müller CA, Uhl W, Büchler MW. Surgical management of severe pancreatitis including sterile necrosis. J Hepatobiliary Pancreat Surg. 2002;9:429–35.
Tonsi AF, Bacchion M, Crippa S, Malleo G, Bassi C. Acute pancreatitis at the beginning of the 21st century: the state of the art. World J Gastroenterol. 2009;15:2945–59.
Gloor B, Uhl W, Büchler MW. Changing concepts in the surgical management of acute pancreatitis. Baillieres Best Pract Res Clin Gastroenterol. 1999;13:303–15.
Besselink MG, Verwer TJ, Schoenmaeckers EJ, et al. Timing of surgical intervention in necrotizing pancreatitis. Arch Surg. 2007;142:1194–201.
Segal D, Mortele KJ, Banks PA, Silverman SG. Acute necrotizing pancreatitis: role of CT-guided percutaneous catheter drainage. Abdom Imaging. 2007;32:351–61.
van Baal MC, van Santvoort HC, Bollen TL, et al. Systematic review of percutaneous catheter drainage as primary treatment for necrotizing pancreatitis. Br J Surg. 2011;98:18–27.
Ferrucci JT 3rd., Mueller PR. Interventional approach to pancreatic fluid collections. Radiol Clin North Am. 2003;41:1217–26. vii.
Simchuk EJ, Traverso LW, Nukui Y, Kozarek RA. Computed tomography severity index is a predictor of outcomes for severe pancreatitis. Am J Surg. 2000;179:352–5.
Acknowledgment
The authors acknowledge the support extended by Departments of Gastro-medicine, Gastro-surgery, Radiology, and Nephrology of our institution in the management of SAP.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Singh, R.K., Poddar, B., Baronia, A.K. et al. Audit of patients with severe acute pancreatitis admitted to an intensive care unit. Indian J Gastroenterol 31, 243–252 (2012). https://doi.org/10.1007/s12664-012-0205-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-012-0205-1