Abstract
Purpose
The primary objectives of this historical case-control study were to evaluate the incidence of and reasons and risk factors for adult unanticipated admissions in three tertiary care Canadian hospitals following ambulatory surgery.
Methods
A random sample of 200 patients requiring admission (cases) and 200 patients not requiring admission (controls) was taken from 20,657 ambulatory procedures was identified and compared. The following variables were included: demographics, reason for admission, type of anesthesia, surgical procedure, length of procedure, American Society of Anesthesiologists’ (ASA) classification, surgical completion time, pre-anesthesia clinic, medical history, medications (classes), and perioperative complications. Multiple logistic regression analysis was used to assess factors associated with unanticipated admissions.
Results
The incidence of unanticipated admission following ambulatory surgery was 2.67%. The most common reasons for admission were surgical (40%), anesthetic (20%), and medical (19%). The following factors were found to be associated with an increased risk of unanticipated admission: length of surgery of one to three hours (odds ratio [OR] 16.70; 95% confidence interval [CI] 4.10 to 67.99) and length of surgery more than three hours (OR 4.26; 95% CI 2.40 to 7.55); ASA class III (OR 4.60; 95% CI 1.81 to 11.68); ASA class IV (OR 6.51; 95% CI 1.66 to 25.59); advanced age (> 80 yr) (OR 5.41; 95% CI 1.54 to 19.01); and body mass index (BMI) of 30-35 (OR 2.81; 95% CI 1.31 to 6.04). Current smoking status was found to be associated with a decreased likelihood of unanticipated admission (OR 0.44; 95% CI 0.23 to 0.83), as was monitored anesthesia care when compared with general anesthesia (OR 0.17; 95% CI 0.04 to 0.68) and plastic (OR 0.18; 95% CI 0.07 to 0.50), orthopedic (OR 0.16; 95% CI 0.08 to 0.33), and dental/ear-nose-throat surgery (OR 0.32; 95% CI 0.13 to 0.83) when compared with general surgery. Other comorbid conditions did not impact unanticipated admission.
Conclusion
Unanticipated admission after ambulatory surgery occurs mainly due to surgical, anesthetic, and medical complications. Length of surgery more than one hour, high ASA class, advanced age, and increased BMI were all predictors. No specific comorbid illness was associated with an increased likelihood of unanticipated admission. These findings support continued use of the ASA classification as a marker of patient perioperative risk rather than attributing risk to a specific disease process.
Résumé
Objectif
Les objectifs primaires de cette étude cas-témoin historique étaient d’évaluer l’incidence ainsi que les raisons et les facteurs de risque des admissions non anticipées de patients adultes dans trois hôpitaux canadiens de soins tertiaires après une chirurgie ambulatoire.
Méthode
Un échantillon aléatoire de 200 patients nécessitant une admission (cas) et de 200 patients ne nécessitant pas d’admission (témoins) a été identifié et comparé, sur un total de 20 657 interventions ambulatoires. Les variables suivantes ont été incluses: données démographiques, raison de l’admission, type d’anesthésie, intervention chirurgicale, durée de l’intervention, classification selon l’American Society of Anesthesiologists (ASA), temps de chirurgie, clinique préopératoire d’anesthésie, antécédents médicaux, médicaments (classes), et complications périopératoires. On a utilisé une analyse de régression logistique multiple pour évaluer les facteurs associés aux admissions non anticipées.
Résultats
L’incidence d’admissions non anticipées après une chirurgie ambulatoire était de 2,67 %. Les raisons les plus fréquentes d’admission étaient des complications de nature chirurgicale (40 %), anesthésique (20 %), et médicale (19 %). On a observé que les facteurs suivants étaient associés à un risque accru d’admission non anticipée: durée de chirurgie d’une à trois heures (rapport de cotes [RC] 16,70; intervalle de confiance [IC] 95 % 4,10 à 67,99) et durée de chirurgie de plus de trois heures (RC 4,26; IC 95 % 2,40 à 7,55); statut ASA de classe III (RC 4,60; IC 95 % 1,81 à 11,68); anesthésie intraveineuse (RC 6,51; IC 95 % 1,66 à 25,59); âge avancé (> 80 ans) (RC 5,41; IC 95 % 1,54 à 19,01); et indice de masse corporelle (IMC) de 30-35 (RC 2,81; IC 95 % 1,31 à 6,04). On a observé qu’un tabagisme actif était associé à une probabilité réduite d’admission non anticipée (RC 0,44; IC 95 % 0,23 à 0,83), tout comme une sédation consciente par rapport à une anesthésie générale (RC 0,17; IC 95 % 0,04 à 0,68), et une chirurgie plastique (RC 0,18; IC 95 % 0,07 à 0,50), orthopédique (RC 0,16; IC 95 % 0,08 à 0,33), ou dentaire / oto-rhino-laryngée (ORL) (RC 0,32; IC 95 % 0,13 à 0,83) par rapport à une chirurgie générale. Aucun impact sur les admissions non anticipées n’a été observé avec d’autres comorbidités.
Conclusion
Les admissions non anticipées après une chirurgie ambulatoire surviennent principalement en raison de complications chirurgicales, anesthésiques et médicales. Une durée de chirurgie de plus d’une heure, une classe ASA élevée, un âge avancé et un IMC élevé étaient tous des prédicteurs. Aucune comorbidité spécifique n’a été associée à une probabilité accrue d’admission non anticipée. Ces résultats appuient l’utilisation continue de la classification de l’ASA comme marqueur du risque périopératoire d’un patient plutôt que l’attribution du risque à un processus pathologique spécifique.
Similar content being viewed by others
Ambulatory surgery accounts for a significant component of all surgical procedures, and the number continues to climb at a rapid pace with over 35 million ambulatory procedures performed in the USA annually.1 Advances in noninvasive surgical techniques, regional anesthesia, and anesthetic agents with decreased side effects have allowed an increasing number of patients with complex medical issues to undergo ambulatory procedures.2 Several studies have looked at patient safety markers to assess outpatient surgical outcomes.3-5 Unanticipated admission has been suggested as such a marker as well as a way to identify unsuitable ambulatory surgical candidates.6,7 Unanticipated admissions result in inflated costs to an already stressed healthcare system.3,8
In the USA and the UK, the incidence of these unanticipated admissions ranges from 0.9-9.4%.7,9,10 Previously, urological surgery, duration of procedure, and sex were associated with unanticipated admissions.10 A prospective Canadian-based study identified male sex, American Society of Anesthesiologists’ (ASA) physical classification II-III, duration of procedure, and procedures starting after 3 pm as similarly associated with unanticipated admissions.7 Additionally, postoperative bleeding, postoperative nausea/vomiting, and uncontrolled pain were also associated with unanticipated admissions. With the exception of body mass index (BMI)11 and obstructive sleep apnea,12 previous studies on unanticipated admissions focused on the ASA classification or a risk alternative index instead of evaluating specific comorbid illnesses.7,9,10,13 This area has not been studied in over a decade despite the significant advances in technique.7,10
The objective of our study was to evaluate the patient and procedural-related risk factors for unanticipated hospital admission in adult patients following scheduled ambulatory surgery.
Methods
This study was approved by the local Research Ethics Board. A multi-site retrospective case-control study of ambulatory surgical patients at Hamilton Heath Sciences (HHS) was conducted during the 24 month period from June 1, 2008-June 1, 2010.
Facilities
Hamilton Health Sciences is a group of three tertiary care teaching hospitals affiliated with the residency training programs at McMaster University. A complete range of ambulatory surgical procedures are performed at HHS.. Ambulatory procedures performed outside of the operating theatre (Heart Investigation Unit, Electrophysiology Lab, Endoscopy Suites) usually are not monitored by an anesthesiologist and are not included in the study. Postoperatively, patients are monitored in the postanesthesia care unit and then the ambulatory surgical unit. Patients are discharged home from the ambulatory surgical unit when they meet appropriate discharge criteria based on a modified postanesthesia discharge scoring system.14,15
Patients
Using the HHS operating room database, which records type of surgery, admission status, and demographic characteristics, 20,657 ambulatory surgical procedures were identified. Patients who required admission after ambulatory surgery (case patients) were compared with those who underwent ambulatory surgery but did not require admission (control patients). Cases included in the analysis were adults (18 yr of age or older) scheduled for outpatient ambulatory surgery. Patients who were scheduled for outpatient surgery but were subsequently admitted prior to the procedure were excluded. Also, patients identified at their pre-anesthetic visit to require admission preoperatively or postoperatively were similarly excluded. To maintain patient confidentiality, cases were assigned an identifier number unique to this study, and at no time were hospital-based identifiers used on data extraction forms or in the databases generated from chart review. Cases were randomly selected using computer-generated software, and four different reviewers manually reviewed charts to extract information not available in the electronic database. To assess inter-reviewer reliability, a random sample of 10% of the total data set was selected and reviewed by two reviewers. To assess reproducibility of the data abstraction process, agreement between reviewers was calculated and resulted in 95% accuracy.
Sample size
The total sample size for the study was 400 patients, with 200 case patients and 200 control patients. To create a model using logistic regression that discriminates between cases and controls, simulation studies have shown that 10-15 events per predictor variable are required.16,17 For this study, since some variables are collinear, it was decided that a maximum of 20 independent variables would be included in the final model, and a sample size of 400 with 200 cases was considered sufficient to produce a stable model. The case and control groups were not matched as we were most interested in investigating demographic, medical, and surgical fields in our analysis.
Data collection
Data extraction included variables assessed in previous studies: demographics, type of anesthesia, surgical procedure, length of procedure, ASA classification, time of completion of surgery, pre-anesthesia clinic visit, and chronic opiate use. Surgical procedures were classified according to the International Classification of Disease Procedures Code (ICD-9-CM): chronic pain block, dental surgery, general surgery, gynecology, neurosurgery, ophthalmology, orthopedics, plastic surgery, and urology.18
In addition, we recorded other variables that we deemed to be predictive of admission. These included BMI, Mallampati score, comorbid medical conditions, medication class, and the presence of intraoperative complications/events. Intraoperative events were limited to difficult intubation/multiple attempts, bronchospasm requiring inhaled bronchodilators, laryngospasm, and blood loss requiring transfusion, aspiration, and myocardial ischemia. Pre-existing medical conditions were limited to those identified on the HHS anesthetic record, i.e., hypertension, dysrhythmia/atrial fibrillation, valvular disease/aortic stenosis, congestive heart failure, decreased left ventricular function, peripheral vascular disease, ischemic heart disease, smoking status, recent pneumonia, chronic obstructive pulmonary disorder, cancer, asthma, obstructive sleep apnea, diabetes mellitus, thyroid disorder, seizure disorder, stroke/transient ischemic attack, neuropathy, increased intracranial pressure, neoplasm, renal failure, gastroesophageal reflux disease, liver cirrhosis, dysphagia, osteoarthritis, rheumatoid arthritis, anemia, thromboembolic disease, alcohol abuse, illicit drug use, psychiatric illness, and chronic pain. Chronic pain was defined as opiate consumption on a daily basis for pain control. Finally, the cause of unanticipated admission was recorded and categorized as surgical, anesthetic, medical, or social/administrative.
Data analysis
The demographic, surgical, and anesthetic factors of patients were analyzed to compare differences between patients with and without unanticipated admission. Descriptive statistics were reported by group as mean (standard deviation [SD]) for continuous variables and count (percentage) for categorical variables. Our primary analysis involved multivariable logistic regression to identify the associations with unanticipated admission. The primary outcome (dependent variable) was unanticipated admission, which is a binary variable. We defined unanticipated admission as any patient admitted on the same day as their ambulatory procedure (even if the patient was discharged from the same day surgical unit).The candidate variables included those previously identified (surgical procedure, type of anesthesia, procedure duration, sex, ASA classification, late surgery).4-7 Other clinically sensible conditions included Mallampati score, hospital site, pain (combination of opiate analgesics and chronic pain), BMI score, intraoperative events, psychiatric illness (combination of antidepressants, antipsychotics, anxiolytics, and psychiatric illness), dysrhythmia (combination of atrial fibrillation and dysrhythmia), congestive heart failure (combination of congestive heart failure and decreased left ventricular function), smoking, diabetes, hypertension, ischemic heart disease, sleep apnea, thyroid disease, asthma, stroke/transient ischemic attack, and gastroesophageal reflux disease. In addition, the impact of three interactions on unanticipated admission was assessed, i.e., the interaction between age and ASA score, type of surgery and site of surgery, and ASA score and intraoperative events. The goodness-of-fit of the model was assessed by the Hosmer-Lemeshow test.19 Multiple imputation was used to handle missing data and to provide sensitivity analysis to assess the impact of the missing data on the results. All statistical tests were performed using two-sided tests at the 0.05 level of significance. For logistic regression analysis, the results were expressed as odds ratios, corresponding two-sided 95% confidence intervals, and associated P values. P values are reported to three decimal places, with values less than 0.001 reported as < 0.001. All analysis was performed using SAS® 9.2 (Cary, NC, USA).
Results
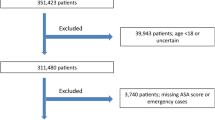
The study results were reported in accordance with the STROBE statement. The flow of patients in the study is summarized using a flow diagram (Figure). The incidence of unanticipated admissions at HHS over a 24-month period spanning June 2008-June 2010 was 2.67%. The most common reasons identified for admission were surgical (40%), anesthetic (20%), and medical (19%), followed by social/administrative (11%) and miscellaneous (8%) (Table 1).
Among admitted patients, the incidence of unanticipated admissions was higher in the older population (age > 40 yr). The following factors were associated with an increased likelihood of admission (P < 0.05): ASA classes II-IV, increased BMI, Mallampati 2, and intraoperative events. The following conditions were found to have a higher incidence in the admitted group (Table 2) but were not found to be associated with unanticipated admission in the multivariable analysis: diabetes, hypertension, ischemic heart disease, psychiatric illness (antidepressants, antipsychotics, and anxiolytics), sleep apnea, and thyroid disease. No specific medication class was associated with an increased likelihood of unanticipated admission.
When compared with general surgery, plastics, gynecology, orthopedics, dental surgery, and ear nose and throat (ENT) surgery had a decreased likelihood of admission, as did monitored anesthesia care (MAC) when compared with general or regional anesthesia. Finally, current smokers had a reduced likelihood of admission when compared with non-smokers (Table 2).
Using multivariable logistic regression analysis, length of surgery more than one hour, ASA class III and IV, advanced age (> 80 yr), and BMI of 30-35 were associated with an increased risk of unanticipated admission. Current smoking status was found to be associated with a decreased likelihood of unanticipated admission, as was MAC when compared with general anesthesia, plastics, orthopedics, and dental/ENT surgery. The results were similar when missing data was handled by multiple imputation (Table 3).
Discussion
This study found that unanticipated admission following ambulatory surgery is common and consistent with previous studies.4,7 We also found a similar consistency where most unanticipated admissions were surgical in nature.7,9 After risk adjustment length of surgery (one to three hours and greater than three hours), high ASA class (III or IV), advanced age, and increased BMI were risk factors associated with an increased likelihood of unanticipated admission.
The strengths of our study included the use of a random sample of cases and controls from three acute care hospitals. Data were extracted on specific medical comorbidities rather than ASA classification alone, and we were able to obtain complete information on the majority of the cases and controls. Our study defined unanticipated admission as those patients who were not discharged home on the day of their ambulatory procedure. One limitation of this study is that we could not quantify patients who were readmitted after a planned discharge. This may have resulted in an underestimation of the actual incidence of admission. In addition, the operating room database requires nurses to enter data, and it is possible that human error could have resulted in incorrect coding. This could have caused either an overestimate or an underestimate of the actual number of adult ambulatory procedures. The retrospective nature of this study does risk some recollection bias; however, due to the standardized anesthetic assessment completed at our institution, we consider this to have been minimized. Additionally, the records were quite complete, with less than 10% of patients having any missing data. Finally, as a potential limitation, urological surgery has previously been identified as an independent predictor of unanticipated admissions10; however, due to the paucity of urological cases performed at the studied sites, this possibility could not be examined in our study.
Many of the factors associated with unanticipated admissions (ASA III or IV, advanced age > 80 yr, increased BMI) could be identified in a pre-anesthetic clinic visit. Specifically, ASA III or IV status was associated with a fourfold increased risk of admission, and age > 80 yr was associated with a fivefold increased risk. Medical reasons for admission (20%) were higher than reported in other recent studies9 and may indicate a need to improve the procedures for selection and screening of suitable patients for day cases. Awareness of these variables could help to guide patient selection for ambulatory surgery during a pre-anesthetic clinic visit. Fleisher et al. have proposed a more formalized scoring system to identify patients at higher risk of unanticipated admission; however, no scoring system is currently utilized at our institution.13
A procedure lasting more than three hours has been identified in numerous studies as being associated with an increased likelihood of unanticipated admission. At our institution, it is rare for ambulatory surgical cases to be booked for more than three hours; as such, these findings likely implicate intraoperative complications. Unlike previous prospective studies, time of completion of surgery was not found to be a predictor of admission in our study.7 This may be accounted for by an institutional policy to book more complicated surgeries in the morning and shorter cases later in the day.
Increased BMI (30-35) was shown to be a predictor of unanticipated admissions, which is in contrast with previous studies.7,11,20 Paradoxically, a BMI > 40 was not associated with increased risk of admission which may be the result may of a reduced sample size of patients with a BMI > 35 in the study. We think the limited number of these obese patients may be due preoperative identification as being at increased risk and thus not selected for ambulatory surgery, whereas the 30-35 BMI group was not identified as being at increased risk.
Smoking was associated with a 56% reduction in risk for unanticipated admission. Although smokers are at increased risk for reactive airways, bronchospasm, and postoperative pulmonary complications,21 studies have shown that smokers have a 4% shorter length of stay following ambulatory surgery.22 This may imply that smokers are intrinsically more motivated to be discharged as a result of addictive behaviours associated with smoking. Additionally, the lower incidence of postoperative nausea/vomiting in smokers23 may account, in part, for the reduced risk of admission.
Fleisher et al. have proposed a preoperatively predictive index for patients at increased risk of unanticipated admission following day surgery.13 Our current research identifies a validation sample and model. Future research will focus on testing the model with a verification sample that could lead to the development of an index used for ambulatory preoperative assessment. Further research will also focus on the pediatric surgery at our institution and factors predictive of unanticipated admission in this population.
In conclusion, this retrospective case-control study has confirmed that unanticipated admission following ambulatory surgery is a common occurrence. Surgical complications were the most common reason for admission following ambulatory surgery. Factors found to be predictive of unanticipated admission included increased BMI, ASA status III or IV, advanced age, and increased length of surgery. Current smokers and patients receiving MAC were associated with a reduced risk of unanticipated admission. Additionally, plastic, orthopedic, dental, and ENT surgery were associated with a reduced risk when compared with general surgery. These findings further strengthen the ASA score as a marker of perioperative risk and also contribute to a clearer understanding of the factors affecting unanticipated admissions, which will help physicians improve the safety and efficiency of ambulatory surgery.
References
Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. National health statistics reports 2009: 1-25.
McGrath B, Chung F. Postoperative recovery and discharge. Anesthesiol Clin North America 2003; 21: 367-86.
Imasogie N, Chung F. Effect of return hospital visits on economics of ambulatory surgery. Curr Opin Anaesthesiol 2001; 14: 573-8.
Twersky RS. To be an outpatient or not to be—selecting the right patients for ambulatory surgery. Ambulatory Surgery 1993; 1: 5-14.
Twersky RS. How to assess quality in ambulatory surgery. J Clin Anesth 1992; 4: 25S-32S.
Shnaider I, Chung F. Outcomes in day surgery. Curr Opin Anaesthesiol 2006; 19: 622-9.
Fortier J, Chung F, Su J. Unanticipated admission after ambulatory surgery—a prospective study. Can J Anaesth 1998; 45: 612-9.
Pavlin DJ, Rapp SE, Polissar NL, Malmgren JA, Koerschgen M, Keyes H. Factors affecting discharge time in adult outpatients. Anesth Analg 1998; 87: 816-26.
Garcea G, Majid I, Pattenden CJ, Sutton CD, Neal CP, Berry DP. Predictive factors for unanticipated admission following day case surgery. J Eval Clin Pract 2008; 14: 175-7.
Twersky RS, Abiona M, Thorne AC, et al. Admissions following ambulatory surgery: outcome in seven urban hospitals. Ambulatory Surgery 1995; 3: 141-6.
Hofer RE, Kai T, Decker PA, Warner DO. Obesity as a risk factor for unanticipated admissions after ambulatory surgery. Mayo Clin Proc 2008; 83: 908-16.
Stierer TL, Wright C, George A, Thompson RE, Wu CL, Collop N. Risk assessment of obstructive sleep apnea in a population of patients undergoing ambulatory surgery. J Clin Sleep Med 2010; 6: 467-72.
Fleisher LA, Pasternak LR, Lyles A. A novel index of elevated risk of inpatient hospital admission immediately following outpatient surgery. Arch Surg 2007; 142: 263-8.
Chung F, Chan VW, Ong D. A post-anesthetic discharge scoring system for home readiness after ambulatory surgery. J Clin Anesth 1995; 7: 500-6.
Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth 1995; 7: 89-91.
Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med 2004; 66: 411-21.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49: 1373-9.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43: 1130-9.
Hosmer DW Jr, Lemeshow S. Applied Logistic Regression. 2nd ed. New York: John Wiley & Sons, Inc; 1989.
Smetana GW, Lawrence VA, Cornell JE, American College of Physicians. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006; 144: 581-95.
Turan A, Mascha EJ, Roberman D, et al. Smoking and perioperative outcomes. Anesthesiology 2011; 114: 837-46.
Chung F, Mezei G. Factors contributing to a prolonged stay after ambulatory surgery. Anesth Analg 1999; 89: 1352-9.
Cohen MM, Duncan PG, DeBoer DP, Tweed WA. The postoperative interview: assessing risk factors for nausea and vomiting. Anesth Analg 1994; 78: 7-16.
Financial support
Department of Anesthesia, McMaster University, Hamilton, Ontario, Canada.
Competing interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is accompanied by an editorial. Please see Can J Anesth 2013; 60: this issue.
Author contributions
Amanda Whippey, Greg Kostandoff, James Paul, Jinhui Ma, and Lehana Thabane helped design the study and write the manuscript. Amanda Whippey, Greg Kostandoff, and James Paul helped conduct the study. Heung Kan Ma helped in data collection, and Jinhui Ma and Lehana Thabane helped analyze the data. James Paul is the author responsible for archiving the study files. Amanda Whippey, Greg Kostandoff, Jinhui Ma, James Paul, Lehana Thabane, and Heung Kan Ma have seen the original study data. Amanda Whippey, Greg Kostandoff, Jinhui Ma, James Paul, and Lehana Thabane reviewed the analysis of the data.
Rights and permissions
About this article
Cite this article
Whippey, A., Kostandoff, G., Paul, J. et al. Predictors of unanticipated admission following ambulatory surgery: a retrospective case-control study. Can J Anesth/J Can Anesth 60, 675–683 (2013). https://doi.org/10.1007/s12630-013-9935-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-013-9935-5