Abstract
Purpose
We look at the changing nature of medical education in the developed world with particular reference to those areas of the new curriculum frameworks which have introduced topics from the psychosocial realm.
Principle findings
Research in the branch of psychology dealing with human factors has developed a useful body of working knowledge which applies to other industries where humans interact with the complex systems in which they function. Some findings are already being applied to facets of anesthesia performance, including situation awareness, effective teamwork, countermeasures against active errors and latent pathogens, and limitations of human performance. However, existing lessons and practices from industrial or military research may not translate directly into effective strategies for anesthesiologists. Collaborative studies between psychologists and clinicians should continue in order to provide the anesthetic curriculum with an effective body of knowledge for each role of the anesthesiologist. Although individual anesthesiologists have made important contributions in this field, such material has not been formally incorporated into the curricula serving anesthesiologists in the developed world.
Conclusions
There is a gap between the human factors psychologists now know and the human factors anesthesiologists need to know. As that gap closes, anesthesiologists may come to think more like human factor psychologists as well as biomedical scientists.
Résumé
Objectif
Nous examinons la nature changeante de la formation médicale dans les pays développés en nous concentrant particulièrement sur les structures des nouveaux programmes d’études qui ont intégré des thèmes tirés du monde de la psychologie.
Constatations principales
La recherche dans la branche de la psychologie s’intéressant aux facteurs humains a permis de créer un corpus utile de connaissances pratiques qui s’appliquent à d’autres domaines dans lesquels l’homme interagit avec les systèmes complexes dans lequel il évolue. Certaines découvertes sont d’ores et déjà appliquées à quelques-unes des facettes de la performance en anesthésie, notamment la prise de conscience de la situation, l’efficacité du travail en équipe, les contre-mesures pour pallier les erreurs actives et les pathogènes latents, et les limites de la performance humaine. Toutefois, les leçons et pratiques existantes tirées de la recherche dans les domaines de l’industrie et de l’armée pourraient ne pas se traduire directement en stratégies efficaces pour les anesthésiologistes. Des études collaboratives réalisées par des psychologues et des cliniciens continuent d’être réalisées. Leur objectif est de fournir au programme de formation en anesthésie un corpus efficace de connaissances concernant chacun des rôles de l’anesthésiologiste. Bien que certains anesthésiologistes aient apporté d’importantes contributions dans ce domaine, celles-ci n’ont pas été intégrées de façon formelle aux programmes suivis par les anesthésiologistes dans les pays développés.
Conclusion
Il existe un fossé entre les facteurs humains que les psychologues connaissent actuellement et les facteurs humains que les anesthésiologistes ont besoin de connaître. Au fur et à mesure que ce fossé se comblera, les anesthésiologistes pourraient être amenés à penser davantage comme des psychologues des facteurs humains et comme des scientifiques biomédicaux.
Similar content being viewed by others
In this article, we explore some of the ways that aspects of psychology are influencing the anesthesiology curriculum. Psychology is a large area of study, and there are many ways in which anesthesiologists collaborate with the different branches, e.g., clinical psychologists working with patients who attend chronic pain specialists. Herein, we confine discussion to those aspects of psychology covered by the term “human factors”. “Human factors refer to environmental, organizational, and job factors and human individual characteristics which influence behaviour at work in a way which can affect health and safety”.1 The psychologists who work in this very large multidisciplinary field typically have a background in cognitive or industrial / organizational psychology and are interested in human performance in the workplace. Much of their research has been conducted traditionally in aviation or military domains, but they have been invited increasingly to collaborate with clinicians, especially anesthesiologists.2-5
Our premise is that interactions between anesthesiologists and human factor psychologists are influencing curriculum content (what should be taught), teaching methods (how it is taught, e.g., simulation, rehearsal, structured practice), and how anesthesiologists are assessed (how we test). As other articles in this issue deal with teaching methods and assessment strategies, we concentrate on curriculum content; we use the CanMEDS 20056 domains to illustrate some of these points, and we then conclude with some thoughts on future directions.
A paradigm shift in medical education
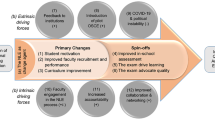
In the last decade, the biggest changes in postgraduate medical education in the developed world have resulted from the introduction of national frameworks such as those used in Canada, the United Kingdom, and the USA (i.e., CanMEDS,6 Competency Framework of the Accreditation Council for Graduate Medical Education [ACGME]),7 and Good Medical Practice.8 These frameworks have formalized an extension of the postgraduate medical curriculum from a largely biomedical model to one that increasingly encompasses a psychosocial model. In this issue of the Journal, Bould et al.9 have also alluded to some of the drivers for this change, including the increasing complexity of medical care and the systems in which it takes place, the diverse range of health care practitioners involved in the patient’s journey, and increasing expectations from the general public about what medical care can achieve. It is hardly surprising that “human factors”, which concerns itself with the efficiency and safety of human performance, has been seen as a possible source of solutions to some of the 21st century’s medical problems.10,11
The strong regulatory culture in postgraduate medical education in Canada, the USA, and the United Kingdom has ensured that the frameworks are applied to all specialities, anesthesiology included. However, this is where some of the challenges become greater. The key domains of the frameworks contain fine words reflecting noble concepts; but how do we provide sufficient and accurate detail and relevant evidence to make them both valid and easily communicated amongst the main players in the educational process? These frameworks have operated in a top-down manner in which those entrusted with regulatory powers have consulted with the subject matter experts to translate the individual domains into something meaningful for the clever end practitioner. Each domain must therefore reflect what the clever end practitioners actually do when performing their jobs. A bottom-up approach may ensure that the activities are consistent with the framework while retaining credibility and validity.
It is in the bottom-up approach that we believe human factors psychology has the greatest role to play. Many of the concepts now populating the domains of these frameworks came into medical consciousness through anesthesiology pioneers exploring the territories of these psychosocial heartlands. Mechanisms of human error, safety cultures, effective teamwork, situation awareness, to name a few, have increasingly permeated the content of anesthesiology and critical care journals, textbooks, and conferences during the last years of the previous century. However, what works well in one industry, most notably aviation, does not necessarily transmit directly to medicine12,13 without significant translation and customization. Collaborative work is required between psychologists and clinicians, and this has generated some useful products, such as the Anaesthetists’ Non-Technical Skills (ANTS) system,14 handoff tools,15 and tools for assessing teamwork in the operating room (OR).16
Curriculum content is therefore beginning to change as human factors research in anesthesiology fleshes out the necessary behavioural evidence to inform educational components within the framework models. For some time, postgraduate medical education has recognized the importance of reflection on one’s actions as a way of identifying areas that need change. The changing nature of the content of the anesthesiology curriculum brought about by human factors work is contributing to the reflective process by providing useful frameworks and terminology. For example, the use of behavioural marker systems17 is exercising a strong influence on the development of workplace-based assessment tools.
The seven CanMEDS 2005 roles apply to all physicians. Anesthesiologists, in the context of perioperative care, exercise their role as physicians by diagnosing and assessing the impact of co-existing medical conditions and any concomitant drug therapy on normal physiology. That role is further put to the test when evaluating the potential impact of surgical stressors on the patient and engaging in dialogue with both patient and surgeon about the best path to optimal perioperative care. Anesthesiology is unique in the frequency with which practitioners suppress protective reflexes, interfere with normal homeostatic mechanisms, and disrupt physiological processes. Only anesthesiologists regularly put patients closer to death, albeit (usually) on a temporary basis. The speed with which events can go wrong and the consequences of such actions can bring about severe disability or death. It is not surprising that anesthesiologists have looked to other industries where there are similar occurrences of time pressures, severe adverse consequences of mistakes or errors, decisions required despite inadequate information, and rapidly changing dynamic circumstances.
Following is a glimpse at each of the seven roles of a physician in the CanMEDS 2005 framework with a review of some of the key areas in which psychology / human factors influence our understanding of these areas as they relate to educating anesthesiologists. It is impossible to cover all areas in an article of this size so we confine ourselves to some illustrative examples.
Medical expert
Relevant key competency
-
1.
Perform a complete and appropriate assessment of the patient
The biomedical model to assess patients, which was taught to generations of medical students, consisted of history, examination, laboratory tests, differential diagnosis, further tests, and treatment. This model continues to have a valuable place in modern practice in all branches of medicine, especially anesthesiology, where clinicians must diagnose and assess those diseases affecting their patients. However, it is not the best model for dealing with acutely ill patients in dynamic conditions where time is limited and immediate action is often necessary. Gaba et al. recognized the importance of situation awareness for anesthesiologists18 and further work continues.19 Situation awareness can be thought of as creating and maintaining an accurate mental model of what is happening to the patient, and it is a key component in the perioperative management of patients, especially during the intraoperative phase when it is of absolute importance. In patients undergoing surgery under general anesthesia, we can only infer what is happening to the patient in terms of response to noxious stimuli and the perfusion of vital organs. The development of a whole set of monitors over the last three decades can be thought of as attempts to provide some answers to these questions. However, no monitors have yet provided us with all of the necessary information, and the anesthesiologist must assimilate many different strands of information from many different sources to create and maintain that mental model.
The focus on book knowledge; physiology, pharmacology, etc. continues to be vital, but we are now beginning to appreciate the importance of the cognitive processes of anesthesiologists, especially during different clinical settings. At one extreme, we have an anesthesiologist managing a major trauma patient and coordinating with surgeons from several different specialties; at the other extreme, we have an anesthesiologist at a pre-assessment clinic dealing with one patient with multiple co-morbidities who was prescribed a large number of daily drugs. Croskerry20,21 has compared how different parts of the brain are used when working in an intuitive fashion vs how they are used when working in a more analytical fashion. Adverse patient outcomes can arise if inappropriate cognitive approaches are used for the set of clinical circumstances. Also, work is ongoing in other cognitive processes, such as fixation errors22 and working23 or prospective memory.24,25 Fixation occurs when a person concentrates on a single aspect of the case to the detriment of other more relevant aspects. Working memory or short-term memory refers to the information in our conscious awareness. Unlike long-term memory, this store has a very limited capacity, holding about four pieces of information at one time. This information is also highly susceptible to interference, which explains why interruptions are so detrimental when we are engaged in tasks that rely heavily on working memory, such as mental arithmetic.
Prospective memory is that which allows us to create a mental list of tasks to be done in the near future and to remember to do them. Work in these areas of the brain is important because of their contribution to potential adverse outcomes, especially if we fail to recognize how hardwiring of the human brain can take us down inappropriate paths. The built-in hardwiring of the human brain to recognize patterns from imprecise information can result in the brain creating inappropriate patterns on the basis of flimsy facts and data. Croskerry has published a list of “hardwired” tendencies in the context of emergency medicine which can result in diagnostic failures. He uses the term “cognitive dispositions to respond”.21 A better understanding of the cognitive processes used to assess what is happening to our patients allows us to develop countermeasures against adverse outcomes. However, if we do not understand how and when to use such countermeasures, how can we instruct our trainees in such processes?
Communicator
Relevant key competencies
-
2.
Accurately elicit and synthesize relevant information and perspectives of patients and families, colleagues, and other professionals;
-
3.
Accurately convey relevant information and explanations to patients and families, colleagues, and other professionals;
-
4.
Develop a common understanding of issues, problems, and plans with patients and families, colleagues, and other professionals to develop a shared plan of care.
Situation awareness comes into prominence once more, but in a social context. The individual health care practitioner (anesthesiologist) not only must develop an accurate mental model but also must communicate and share that mental model with the patient and other relevant health care workers. Shared mental models break down when assumptions are made, when key facts are not communicated, or when key information is not sought and obtained. As health care has become more complex and more individuals with different roles and requirements become involved in the patient’s journey, the need for an accurate shared and up-to-date mental model becomes even more crucial. This is particularly relevant to anesthesiology where the anesthesiologist is often performing a coordinating role between different teams, especially during the management of more complex cases. When the group mental model breaks down, inappropriate decisions are more likely to be made and inappropriate actions may be taken that are to the detriment of the patient.26 Much effort has gone into “communication skills” during the last two decades.27,28 These have been focused largely on doctor-patient relationships, but we are now beginning to develop a better understanding regarding how to communicate effectively with colleagues.29,30 Techniques such as SBAR (Situation, Background, Assessment, Recommendation)31 and closed-loop communication32 are promoted; however, we not only need a better understanding of what works well and what doesn’t, but we also need to understand why certain techniques are effective and when they are effective. How formally are the existing strategies and techniques taught and assessed? How stringent are the criteria that are used to determine whether a good handover (handoff) has taken place?15,33 When we can provide working answers to such questions, then we can construct a body of knowledge that can be formally taught and assessed.
Collaborator
Relevant key competencies
-
1.
Participates effectively and appropriately in an interprofessional health care team
-
2.
Works effectively with other health professionals to prevent, negotiate, and resolve interprofessional conflict.
This section clearly follows the previous one. Effective communication is key to good team work, but good team work is more than good communication.26,31,33-35 For example, the roles performed by both leaders and followers must be taken into account, including delegation, monitoring of team members’ performance, and maintaining accurate mental models.36,37 Recent research suggests that the most effective leadership in anesthesia teams is shared leadership.38
How well do models (e.g., TEAM STEPS)39,40 work for anesthesiologists where existing bodies of knowledge, such as effective teamwork, from other domains have been applied to health care? A study by Morgan et al.41 highlighted the difficulties in evaluating team performance in a simulated obstetric environment in which anesthesiologists participated. In their study, transfer of the existing system of measurement did not appear to capture key aspects of performance, which suggests there are aspects of team performance in this context that require further study to facilitate development of more effective measurement tools.
This implies that more work is needed before the collaborator competencies become the routine standard. As the underlying bodies of knowledge on teamwork are developed, there is a need for collaborative work not only between the different medical specialties but also between different health care professions in order to produce meaningful material that can be taught, developed, and refined in the clinical workplace.
Manager
Key competencies
-
1.
Participate in activities that contribute to the effectiveness of their health care organizations and systems
-
2.
Manage their practice and career effectively
Many aspects of anesthesiology practice transfer well to a formal organizational role. Such aspects include an ability and willingness to collaborate and communicate, to recognize the “larger picture”, and to use “human factors” language and terminology to help make organizations more effective and efficient. Anesthesiologists throughout the world make use of such strengths from the hospital level to the national and international levels. However, not every anesthesiologist has the desire to take on a formal management role, although every physician must influence his/her own working environment to make it effective and efficient. This expertise is not taught formally and does not appear in many written curricula. It involves understanding how the organization works as well as the ability to monitor the organization and identify those components that work well and those that are not working in order to facilitate change and ensure that the organization functions efficiently and effectively. There are many dimensions to consider for inclusion in the formal curriculum, and one way to apply lessons regarding human factors is to detect potential sources of adverse outcomes and establish countermeasures against such outcomes. We next explore the issue of human error as an example. Reason42 has described two types of errors, active errors, caused directly by humans, and latent factors. The latter are present but contribute to adverse outcomes only when activated. Reason compares the latent factors to resident pathogens that normally do not cause harm but may do so when the opportunity arises (e.g., gut flora giving rise to septicemia is associated with a perforated bowel). A variety of strategies have been developed to help identify latent conditions or to reduce their potential harm.43 An example of a technique to reduce error is the performance of a surgical brief before an operating list and the performance of the surgical pause before each patient undergoes surgery. These actions have been shown to reduce errors, including wrong-side operations and failure to administer appropriate antibiotics.44 The process is not the only important issue here; another important factor is the encouragement of greater communication between OR staff. When exchange of information becomes a regular feature of OR practice and an example of management in the day-to-day workplace, it provides the ultimate opportunity to develop teamwork. The process will be obvious to trainees, but the concepts behind the processes may not be as obvious. Further exploration of such concepts is an example of how teaching in this area can take place in the clinical arena. An example of an organizational approach to identify and repair potentially dangerous latent factors is the use of reporting systems. A system that reviews adverse outcomes or near misses can identify latent factors before a major disaster takes place, but the system will enhance safety only if those with influence engage in it.45 Important as engagement is, change is more likely to occur if those analyzing the near misses or adverse outcomes use the language of human factors to facilitate comprehension of the interaction between the practitioners and their environment.
Health advocate
Key competencies
-
1.
Respond to the individual patient’s health needs and issues as part of patient care
-
2.
Respond to the health needs of the communities that they serve
Anesthesiologists help individual patients make decisions by explaining some of the relative risks and benefits of proposed surgical interventions. Such clinical expertise is also brought to bear when looking at potential benefits and risks to groups of patients, for example, determining the level of anesthesiology service required for an obstetric unit to function safely and effectively. Such contributions can extend well beyond the hospital level to the organization of health care for a region, country, or continent.
Anesthesiologists bring more than just their clinical expertise. As has been discussed, the complexity and tight mergence of today’s health care systems in the developed world are themselves a potential source of adverse outcome.46 At the individual and collective levels, anesthesiologists have played an important role in not only advancing patient safety but also in raising the profile of factors that can promote patient safety.5,47
If we consider patient safety from the perspective of how current health care systems can fail to achieve their desired goals and actually result in patient harm, then understanding how the different elements of these systems interact at different levels can help determine where human system interactions can go wrong. Our argument throughout this article is that the nature of the anesthesiologist’s profession, i.e., working with different members of different health care teams—sometimes in periods of high risk and uncertainty with great time pressures and severe threat to outcomes—has encouraged anesthesiologists to look for sources of help. Lessons anesthesiologists have learned from the application of human factors in other industries have placed us at the forefront of the patient safety movement;46 therefore, in the context of Health Advocate, we not only can develop that expertise and understanding but also we can share it with others in the quest to make our systems safer for our current patients and those who may need to use our systems in the future.
Scholar
Key competencies
-
1.
Maintain and enhance professional activities through ongoing learning
-
3.
Facilitate the learning of patients, families, students, residents, other health professionals, the public, and others as appropriate
-
4.
Contribute to the creation, dissemination, application, and translation of new medical knowledge and practices.
For the purpose of this review, this topic can be summarized as follows: What do psychologists already know that anesthesiologists should know, and what would anesthesiologists like to know that psychologists can help them find out? Unlike the biomedical component, which is readily available and dealt with in textbooks, journals, and conferences, we contend that the skills and behaviours pertaining to the psychosocial element have been acquired in a much less formal way – by copying behaviours in the clinical environment or through a process of trial and error. These characteristics make it difficult to instruct and assess the majority of practicing anesthesiologists all over the world.
The role of scholar is actively maintained through many contributions to research— only a mere fraction of which we have mentioned—and education. Although we have focused on the education of anesthesiologists, we recognize the duty that anesthesiology as a specialty has to contribute to the education of others. Many anesthesiologists already contribute formally to the dissemination of existing human factors knowledge in health care, e.g., by involvement with specific medical undergraduate courses and simulation-based education. Clearly, there is more scope for anesthesiologists, especially those in university departments, to contribute to the education of medical undergraduates and those engaged in formal education in other health care professions.
The implementation of national frameworks, such as CanMEDS, should encourage us to bring this knowledge into the formal curriculum so that it becomes as much a part of anesthesiology knowledge as a part of the knowledge of cardiovascular physiology and pharmacokinetics. It is existing knowledge that provides the theories to underpin our practice as we aim to improve standards of care.
As teachers, we can assist our trainees by helping them reflect on their current levels of performance and practice. However, work has shown that doctors in general could be better at debriefing.48 Given the importance of making trainees aware of human factor issues in the clinical workplace, our skills in debriefing and teaching in this setting are essential, especially if we intend to help our trainees learn what psychologists already know and what anesthesiologists should learn. As Bould et al. 9 have pointed out, engagement with qualitative research is necessary not only for those conducting such work but also for those critically reading journal articles or textbooks. One of the challenges addressed in this issue of the Journal is not only the content of the curriculum but also the ability of anesthesiologists to teach and assess the trainees of today.
Professional
Key competencies
-
1.
Demonstrate a commitment to their patients, profession, and society through ethical practice
-
3.
Demonstrate a commitment to physician health and sustainable practice
Professionalism is often promoted in terms of values and the behaviours that are manifestations of those values. However, as key competency #3 reveals, working to high standards requires anesthesiologists to be aware of how they are performing and, in particular, aware of factors that will impinge on that performance. Factors such as stress, fatigue, hunger, thirst, and ageing can have negative impacts on the cognitive performance of anesthesiologists.49 The ability to recognize deterioration in one’s own performance or that of one’s colleagues is a relatively new change in approach for medicine. The macho culture of long hours, little sleep, and long periods without meals is changing as the complexities of health care (patients with more comorbidities undergoing more complex procedures) place greater demands on today’s anesthesiologists. Specific content has not become integrated to the extent that other industries at the astute end of human-systems interactions have adopted such knowledge into their curricula. Pilots undergo formal instruction and assessment in limitations of human performance.50 This is yet another area that could be incorporated into the knowledge-based components of the anesthesiology curriculum.
Conclusion
This article has focused on ways in which the body of knowledge developed by psychologists working in the field of human factors can apply to the practice of anesthesia and help provide curriculum content for each of the seven roles outlined in CanMEDS 2005.
We are aware that anesthesiologists perform other roles (e.g., expert witnesses and government advisers); however, we chose to concentrate on the core curriculum for all anesthesiologists.
Application of existing knowledge is merely an entry point to further work that can help us explore the principles described above in the context of our clinical work. A vast amount of work has yet to be undertaken in areas such as the cognitive processes of anesthesiologists, effective team work in dynamic environments with the potential for multiple leaders, engaging effectively with complex systems of care, and coping with the physical, mental, and social demands of our jobs. Developing the legacy of work entrusted to us by pioneers in these fields can allow us to reshape the anesthesiology curriculum into a tool fit for the anesthesiologists of the forthcoming century.
Key points
-
The medical curriculum is expanding to incorporate elements from the psychosocial models of human performance.
-
Anesthesiologists have taken a lead in patient safety, but further work is required to provide sufficient and accurate curriculum content.
-
Important aspects of cognition include better understanding of situation awareness, decision-making strategies, use of working memory, and prospective memory.
-
Important social areas include shared leadership models, a better understanding of interprofessional working during time pressures and high-risk dynamic clinical situations.
-
Understanding of limitations of human performance, including fatigue and stress, on both the cognitive and social processes is also necessary to reduce error and adverse outcomes.
-
There is a gulf between what psychologists know and what anesthesiologists need to know. Curriculum reform allows narrowing of that gap.
References
Health & Safety Executive. Reducing Error and Influencing Behaviour, 2nd ed. HSG48, London: HSE Books; 1999.
Helmreich RL, Davies JM. Human factors in the operating room: interpersonal determinants of safety, efficiency and morale. Best Pract Clin Anaesthesiol 1996; 10: 277-95.
Klemola UM, Norros L. Analysis of the clinical behaviour of anaesthetists: recognition of uncertainty as a basis for practice. Med Educ 1997; 31: 449-56.
Manser T, Harrison T, Gaba D, Howard S. Coordination patterns related to high clinical performance in a simulated anesthesia crisis. Anesth Analg 2009; 108: 1606-15.
Runciman WB, Webb RK, Lee R, Holland R. The Australian Incident Monitoring Study. System failure: an analysis of 2000 incident reports. Anaesth and Intensive Care 1993; 21: 684-95.
Royal College of Physicians and Surgeons of Canada. CanMEDS Competency Framework (2005). Available from URL; http://rcpsc.medical.org/canmeds (accessed July 2011).
Accreditation Council for Graduate Medical Education. Outcome Project. Available from URL: http://www.acgme.org/Outcome (accessed July 2011).
General Medical Council. Good Medical Practice: Duties of a doctor. Available from UR: http://www.gmc-uk.org/guidance/good_medical_practice/duties_of_a_doctor.asp (accessed August 2011).
Bould MD, Naik VN, Hamstra SJ. Review article: New directions in medical education related to anesthesiology and perioperative medicine. Can J Anesth 2012; 59: this issue. DOI:10.1007/s12630-011-9633-0.
Carayon P. Handbook of Human Factors and Ergonomics for Patient Safety. Mahwah: NJ: Erlbaum; 2007.
Flin R, Winter J, Sarac C, Raduma M. Human Factors in Patient Safety: Review of Topics and Tools. Report for Methods and Measures Working Group of WHO Patient Safety. Geneva: World Health Organization. 2009; WHO/IER/PSP/2009.05. Available from URL: http://www.who.int/patientsafety/research/methods_measures/human_factors/human_factors_review.pdf (accessed August 2011).
Helmreich R, Merrit A. Culture at Work in Aviation and Medicine. Aldershot: Ashgate Publishing; 2001 .
Musson D. Putting behavioural markers to work: developing and evaluating safety training in healthcare settings. In: Flin R, Mitchell L, editors. Safer Surgery. Analysing Behaviour in the Operating Theatre. Farnham: Ashgate Publishing; 2009. p. 423-35.
Flin R, Patey R, Glavin R, Maran N. Anaesthetists’ non-technical skills. Br J Anaesth 2010; 105: 38-44.
Manser T, Foster S, Gisin S, Jaeckel D, Ummehofer W. Assessing the quality of patient handoffs at care transitions. Qual Saf Health Care 2010; 19: 1-5.
Undre S, Sevdalis N, Healey AN, Darzi A, Vincent CA. Observational teamwork assessment for surgery (OTAS): refinement and application in urological surgery. World J Surg 2007; 31: 1373-81.
Flin R, O’Connor P, Crichton M. Safety at the Sharp End: A Guide to Non-Technical Skills. Aldershot: Ashgate Publishing; 2008 .
Gaba DM, Howard SK, Small SD. Situation awareness in anesthesiology. Hum Factors 1995; 37: 20-31.
Fioratou E, Flin R, Glavin R, Patey R. Beyond monitoring: distributed situation awareness in anaesthesia. Br J Anaesth 2010; 105: 83-90.
Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med 2003; 78: 775-80.
Croskerry P. A universal model of diagnostic reasoning. Acad Med 2009; 84: 1022-8.
Fioratou E, Flin R, Glavin R. No simple fix for fixation errors: cognitive processes and their clinical applications. Anaesthesia 2010; 65: 61-9.
Bartel P, Offermeir W, Smith F, Becker P. Attention and working memory in resident anaesthetists after night duty: group and individual effects. Occup Environ Med 2004; 61: 167-70.
Dieckmann P, Madsen M, Reddersen S, Rall M, Wehner T. Remembering to do things later and resuming interrupted tasks: prospective memory and patient safety. In: Flin R, Mitchell L, editors. Safer Surgery. Analysing Behaviour in the Operating Theatre. Farnham: Ashgate Publishing; 2009. p. 339-52.
Grundgeiger T, Sanderson P, MacDougall HG, Venkatesh B. Interruption management in the intensive care unit: predicting resumption times and assessing distributed support. J Exp Psychol Appl 2010; 16: 317-34.
Reader T, Flin R, Mearns K, Cuthbertson B. Developing a team performance framework for the intensive care unit. Crit Care Med 2009; 37: 1787-93.
Kurtz S, Silverman J, Draper J. Teaching and Learning Communication Skills in Medicine. 2nd ed. Abingdon, Oxfordshire: Radcliffe Publishing Ltd; 2005 .
Smith AF, Shelley MP. Communication skills for anesthesiologists. Can J Anesth 1999; 46: 1082-8.
Smith AF, Pope C, Goodwin D, Mort M. Communication between anesthesiologists, patients and the anesthesia team: a descriptive study of induction and emergence. Can J Anesth 2005; 52: 915-20.
Smith A, Pope C, Goodwin D, Mort M. Teams, talk and transitions in anaesthetic practice. In: Flin R, Mitchell L, editors. Safer Surgery. Analysing Behaviour in the Operating Theatre. Farnham: Ashgate Publishing; 2010. p. 241-57.
Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf 2006; 32: 167-75.
Wilson KA, Burke CS, Priest HA, Salas E. Promoting healthcare safety through training high reliability teams. Qual Saf Health Care 2005; 14: 303-9.
Smith AF, Pope C, Goodwin D, Mort M. Interprofessional handover and patient safety in anaesthesia: observational study of handovers in the recovery room. Br J Anaesth 2008; 101: 332-7.
Manser T, Howard SK, Gaba DM. Adaptive coordination in cardiac anaesthesia: a study of situational changes in coordination patterns using a new observation system. Ergonomics 2008; 51: 1153-78.
Xiao Y, Hunter WA, Mackenzie CF, Jefferies NJ, Horst RL. Task complexity and emergency medical care and its implications for team coordination. LOTAS Group. Level One Trauma Anesthesia Simulation. Hum Factors 1996; 38: 636-45.
Makary MA, Sexton JB, Freischlag JA, et al. Operating room teamwork among physicians and nurses: teamwork in the eye of the beholder. J. Am Coll Surg 2006; 202: 746-52.
Marsch SC, Muller C, Marquardt K, Conrad G, Tschan F, Hunziker PR. Human factors affect the quality of cardiopulmonary resuscitation in simulated cardiac arrests. Resuscitation 2004; 60: 51-6.
Kunzle B, Zala-Mezo E, Wacker J, Kolbe M, Spahn DR, Grote G. Leadership in anaesthesia teams: the most effective leadership is shared. Qual Saf Health Care 2010; 19: e46.
Baker DP, Day R, Salas E. Teamwork as an essential component of high reliability organisations. Health Serv Res 2006; 41: 1576-98.
Capella J, Smith S, Philp A, et al. Teamwork training improves the clinical care of trauma patients. J Surg Educ 2010; 67: 439-43.
Morgan PJ, Pittini R, Regehr G, Marrs C, Haley MF. Evaluating teamwork in a simulated obstetric environment. Anesthesiology 2007; 106: 907-15.
Reason J. Managing the Risks of Organizational Accidents. Aldershot: Ashgate Publishing; 1997 .
Jackson J, Sarac C, Flin R. Hospital safety climate surveys: measurement issues. Curr Opin Crit Care 2010; 106: 907-15.
Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009; 360: 491-9.
Nuckols TK, Bell DS, Liu H, Paddock SM, Hilborne LH. Rates and types of events reported to established incident reporting systems in two US hospitals. Qual Saf Health Care 2007; 16: 164-8.
Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington, DC: Institute of Medicine. National Academy of Sciences; 1999 .
Gaba DM, Fish KJ, Howard SK. Crisis Management in Anesthesiology. New York: Churchill Livingstone; 1994 .
Rudolph JW, Simon R, Dufresne RL, Raemer DR. There’s no such thing as “non-judgmental” debriefing: a theory and method for good judgment. Simul Healthc 2006; 1: 49-55.
Glavin R. Human Performance Limitations (communication, stress, prospective memory and fatigue). Best Pract Res Clin Anaesthesiol 2011; 25: 193-206.
Campbell RD, Bagshaw M. Human Performance and Limitations in Aviation. 3rd ed. Oxford: Blackwell Science Ltd; 2002.
Financial support
None received.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Glavin, R., Flin, R. Review article: The influence of psychology and human factors on education in anesthesiology. Can J Anesth/J Can Anesth 59, 151–158 (2012). https://doi.org/10.1007/s12630-011-9634-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-011-9634-z