Abstract
Purpose
Mitochondrial calcium sensitive potassium (mKCa) channels are involved in cardioprotection induced by ischemic preconditioning. In the present study we investigated whether morphine-induced preconditioning also involves activation of mKCa channels.
Methods
Isolated rat hearts (six groups; each n = 8) underwent global ischemia for 30 min followed by a 60-min reperfusion. Control animals were not further treated. Morphine preconditioning (MPC) was initiated by two five-minute cycles of morphine 1 μM infusion with one five-minute washout and one final ten-minute washout period before ischemia. The mKCa blocker, paxilline 1 μM, was administered, with and without morphine administration (MPC + Pax and Pax). As a positive control, we added an ischemic preconditioning group (IPC) alone and combined with paxilline (IPC + Pax). At the end of reperfusion, infarct sizes were determined by triphenyltetrazoliumchloride staining.
Results
Infarct size was (mean ± SD) 45 ± 9% of the area at risk in the Control group. The infarct size was less in the morphine or ischemic preconditioning groups (MPC: 23 ± 8%, IPC: 20 ± 5%; each P < 0.05 vs Control). Infarct size reduction was abolished by paxilline (MPC + Pax: 37 ± 7%, P < 0.05 vs MPC and IPC + Pax: 36 ± 6%, P < 0.05 vs IPC), whereas paxilline alone had no effect (Pax: 46 ± 7%, not significantly different from Control).
Conclusion
Cardioprotection by morphine-induced preconditioning is mediated by activation of mKCa channels.
Résumé
Objectif
Les canaux potassiques mitochondriaux calcium-dépendants (mKCa) participent à la cardioprotection induite par le préconditionnement ischémique. Dans la présente étude, nous avons tenté de découvrir si le préconditionnement provoqué par la morphine implique également l’activation des canaux mKCa.
Méthodes
Des cœurs isolés de rats (six groupes; chacun de n = 8) ont été soumis à une ischémie globale pendant 30 min, suivie d’une perfusion de 60 min. Les animaux témoins n’ont reçu aucun autre traitement. Le préconditionnement provoqué par la morphine (MPC) a été initié par deux cycles de cinq minutes d’une perfusion de morphine à 1 μM, avec une période de rinçage de cinq minutes et une période de rinçage finale de dix minutes avant l’ischémie. L’inhibiteur des canaux mKCa, la paxilline à 1 μM, a été administré, avec ou sans administration de morphine (MPC + Pax et Pax). À titre de valeur témoin positive, nous avons ajouté un groupe soumis à un préconditionnement ischémique (IPC) seul et combiné à la paxilline (IPC + Pax). À la fin de la reperfusion, la taille de chaque infarctus a été déterminée par la coloration du chlorure de tryphényltétrazolium.
Résultats
La taille de l’infarctus couvrait 45 ± 9 % (moyenne ± écart type) de la zone à risque dans le groupe témoin. La taille de l’infarctus était moins importante dans les groupes ayant reçu de la morphine ou ayant subi un préconditionnement ischémique (MPC: 23 ± 8 %, IPC: 20 ± 5 %; chacun de P < 0,05 contre le groupe témoin). L’effet de réduction de la taille de l’infarctus a été éliminé par la paxilline (MPC + Pax: 37 ± 7 %, P < 0.05 contre MPC et IPC + Pax: mi,que (MPC ± 6 %, P < 0,05 contre IPC), tandis qu’administrée seule, la paxilline n’a eu aucun effet (Pax: 46 ± 7 %, aucune différence notable comparativement au groupe témoin).
Conclusion
La cardioprotection par préconditionnement provoqué par la morphine est assistée par l’activation des canaux mKCa.
Similar content being viewed by others
Cardioprotection by preconditioning can be induced by various stimuli, such as brief cycles of ischemia or pharmacological agents, including volatile anesthetics and morphine1,2. Both ischemic and morphine preconditioning protect the heart by sharing common cellular pathways. Opening of mitochondrial ATP-sensitive potassium (mKATP) channels is involved in regulation of mitochondrial functions, representing a key step in mediating the cardioprotective effects of ischemic- and morphine-induced preconditioning, possibly due to inhibition of mitochondrial permeability transition pore (mPTP).3-5 Besides opening of mKATP channels, activation of the mitochondrial calcium sensitive potassium (mKCa) channel is also involved in preconditioning.6,7 Cao et al. demonstrated that activation of mKCa channels plays a crucial role in ischemic preconditioning and that cardioprotection, by activation of mKCa channels, is independent of mKATP channels and vice versa.8 In another study, the same authors demonstrated that preconditioning by activation of κ-opioid receptors is triggered by mKCa channels.9 However, the opioid, morphine, is predominantly a μ-receptor agonist and has only a low affinity for κ-opioid receptors.10,11 Furthermore, there is no κ-opioid agonist for clinical practice available. It is not known whether activation of mKCa channels is involved in morphine-induced preconditioning. The purpose of the present study was to test the hypothesis that morphine-induced preconditioning is mediated by activation of mKCa channels.
Methods
The investigation conforms to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996) and was performed in accordance with the requirements of the Animal Ethics Committee of the University of Duesseldorf, Duesseldorf, Germany.
Chemicals and reagents
All chemicals were purchased from Sigma-Aldrich (Taufkirchen, Germany).
Surgical preparation
Male Wistar rats were used for these studies. The rats were maintained on a 12:12 light/dark schedule (lights on at 0600 hr) with food and water provided ad libitum. The animals were anesthetized with pentobarbital 90 mg · kg−1 ip. After thoracotomy, the hearts were excised, mounted on a Langendorff system, and perfused at constant pressure (80 mmHg) with Krebs–Henseleit solution containing (in mM) 116 NaCl, 4.7 KCl, 1.1 MgSO4, 1.17 KH2PO4, 24.9 NaHCO3, 2.52 CaCl2, 8.3 glucose, and 2.2 pyruvate at 37°C. A fluid-filled balloon was inserted into the left ventricle, and end-diastolic pressure was set at 1-4 mmHg. All hearts underwent a stabilization period of 20 min. Heart rate (HR), myocardial function (isovolumetric left ventricular pressure), coronary flow, left ventricular end-diastolic pressure, and rate of left ventricular pressure development (dP/dtmax) were measured continuously. The data were digitized using an analogue to digital converter (PowerLab/8SP, ADInstruments Pty Ltd, Castle Hill, Australia) at a sampling rate of 500 Hz, and they were recorded continuously on a personal computer using Chart for Windows v5.0 (ADInstruments). Maximal contracture and time to maximal contracture were noted during ischemia. Arrhythmic intervals were not used for data analysis.
Experimental protocol for infarct size determination
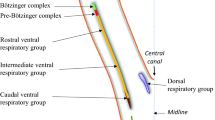
The hearts were assigned randomly to one of six experimental groups (Figure 1). The hearts of all groups underwent 30 min of ischemia followed by 60 min of reperfusion. In the control group (Con), the hearts were kept under baseline conditions prior to ischemia. To investigate whether morphine induces preconditioning (MPC), morphine 1 μM was given in two five-minute cycles, separated by one five-minute washout period, and ending with one final ten-minute washout period prior to ischemia. The morphine concentration was chosen because Liang et al. demonstrated that the preconditioning effect of morphine was maximal at 1 μM.12 Morphine was dissolved in 0.9% NaCl and separately infused into a mixing chamber placed in the perfusion system. As a positive control, the ischemic preconditioning group (IPC) underwent two similar five-minute cycles of ischemia ten minutes prior to ischemia. To test whether mKCa channels are involved in the phenomenon of preconditioning, the mKCa channel inhibitor, paxilline 1 μM,8,9 was given over 25 min together with morphine- and ischemic-induced preconditioning (MPC + Pax and IPC + Pax). To rule out an effect of paxilline itself, we investigated the effect of paxilline alone (Pax).
After 60 min of reperfusion, the heart was cut into transverse slices, which were then stained with 0.75% triphenyltetrazoliumchloride solution. The infarcted area was determined by planimetry using SigmaScan Pro 5® computer software (SPSS Science Software, Chicago, IL, USA).
Statistical analysis
The sample size was calculated using GraphPad StatMate™ Version 1.01 (GraphPad Software, San Diego, CA, USA). Sample size analysis revealed that a group size of n = 8 was necessary to detect a difference in infarct size of 25% with a power of 80% and an α < 0.05. The estimations of the mean difference of 25% and the standard deviation (SD) of 15% were based on our own data.13 Data are expressed as mean ± SD. Heart rate (in min−1) and mean aortic pressure (in mmHg) were measured during baseline, coronary artery occlusion, and reperfusion period. Comparisons of hemodynamics between groups or between time points in a group were performed (SPSS Science Software, version 12.0.1) using two-way analysis of variance followed by Dunnett’s post hoc test. A researcher blinded to the experimental groups determined the infarct sizes. The infarcts were analyzed by Student’s t test followed by Bonferroni’s correction for multiple comparisons. Changes within and among groups were considered statistically significant if P < 0.05.
Results
No differences in body or heart weight were observed between the groups (Table 1). In the preconditioning groups, the level of maximal ischemic contracture was significantly lower, and the time of maximal ischemic contracture was significantly higher compared with the Control group (P < 0.05 vs Con) (Table 1).
Infarct size measurement
In the Control group, infarct size was (mean ± SD) 45 ± 9% of the area at risk (Figure 2). In the ischemic- and morphine-induced preconditioning groups, infarct size was similar and significantly less than in the Control group (IPC: 20 ± 5%, MPC: 23 ± 8%; each P < 0.05 vs Con) (Figure 2). The preconditioning effect of ischemia and morphine was attenuated significantly by the mKCa-channel inhibitor, paxilline. Infarct size was 36 ± 6% and 37 ± 7% in the IPC + Pax and MPC + Pax groups, respectively; each P < 0.05 vs IPC and MPC, respectively (Figure 2). Paxilline alone had no effect on infarct size (Pax: 46 ± 7%; not significantly different from Con). There was no significant difference in infarct size between the preconditioning groups with paxilline compared with the Control group.
Infarct size measurement. Histogram showing the infarct size (IS) as percent of area at risk (AAR) in Controls (Con, n = 8), morphine preconditioning (MPC, n = 8), ischemic preconditioning (IPC, n = 8), morphine preconditioning with paxilline (MPC + Pax, n = 8), ischemic preconditioning with paxilline (IPC + Pax, n = 8), and paxilline alone (Pax, n = 8). Data are mean ± SD; * P < 0.05 vs Con; # P < 0.05 vs IPC; § P < 0.05 vs MPC
Hemodynamic variables
Hemodynamic variables are summarized in Table 2. No significant differences in left ventricular end-diastolic pressure and dP/dtmax were observed between the experimental groups during baseline conditions and at the beginning of ischemia (Table 2). At the end of the experiment, dP/dtmax was higher in the preconditioning groups (Table 2). There was no difference in HR compared with Controls at baseline and during reperfusion, with the exception of the paxilline group at time point final ten-minute washout shortly before index ischemia (Table 2).
Discussion
The main finding of our study is that the opioid, morphine, initiates preconditioning in a similar manner as ischemia, i.e., by activation of mKCa channels.
Ischemic preconditioning (IPC) describes a cardioprotective phenomenon where short periods of myocardial ischemia protect the heart against a subsequent longer period of ischemia and reduce the deleterious consequences of ischemia/reperfusion injury.14 Besides ischemic stimuli, volatile anesthetics15,16 and morphine can mimic the cardioprotective effect of preconditioning.17 In contrast to volatile anesthetics, morphine can be administered to patients who are subjected to organ ischemia (vascular surgery, organ transplantation, cardiac surgery) or who recently underwent regional ischemia (stroke, angina pectoris, myocardial infarction, organ transplantation) without the side effect of being “anesthetized”. The mechanisms by which opioids protect the myocardium share common pathways with ischemic preconditioning. Opening of mitochondrial ATP-sensitive potassium (mKATP) channels that are involved in regulating mitochondrial functions is a key step that mediates cardioprotection induced by both morphine and ischemic preconditioning, possibly through inhibition of mitochondrial permeability transition pore (mPTP) opening.3,5
Mitochondrial calcium sensitive potassium (mKCa) channels seem to be another class of K+ channels, apart from mKATP channels, that mediate cardioprotection by preconditioning.6,7 In 2002, Xu et al.7 reported that KCa-activated potassium channels are located on the inner mitochondrial membrane and mediate cardioprotection against ischemia and reperfusion injury in the isolated perfused guinea pig heart. Since this initial observation, mKCa-activated potassium channels have been found to be implicated in ischemic preconditioning against ischemia and reperfusion injury in isolated rat and mouse hearts, anesthetized dogs, and isolated cardiac myocytes.6,8,9,18,19
The mKCa channel contains a pore forming α-subunit and a regulatory β-subunit.20-22 The β-subunit consists of four accessory β-subunits (β1-4). Both mKATP and mKCa channel activation triggers preconditioning that is independent one from the other and involves the mPTP. 8 Cao et al. showed that ischemic preconditioning is triggered by activation of mKCa channels and is abolished by the mKCa channel inhibitor, paxilline.8 Paxilline is a mycotoxin produced by the fungus, Penicillium paxilli. It has the ability to block all subunits23 of mKCa channels and is a selective inhibitor.24 Besides paxilline, there are not many mKCa channel blockers available. Iberiotoxin, for example, is a mKCa channel blocker that is also suitable for in vivo use,13 whereas paxilline is predominantly used for in vitro experiments. However, we did not check whether iberiotoxin also abolishes morphine preconditioning. Besides ischemic preconditioning, our results demonstrate that pharmacological preconditioning with morphine also induces cardioprotection by activation of mKCa channels. Cao et al.8 administered the mKCa channel blocker, paxilline, at the onset of reperfusion after a prolonged period of ischemia. We applied paxilline during the preconditioning period, suggesting that mKCa channel inhibition blocks the infarct size reducing effect of preconditioning during the trigger phase. In a recent study, we could demonstrate that activation of mKCa channels not only reduced infarct size by preconditioning but also caused a significant reduction in the mitochondrial respiratory control index.13 Co-administration of the mKCa channel blocker, iberiotoxin, completely abolished the reduction in the respiratory control index, and we concluded that cardioprotection is mediated by activation of mKCa channels leading to mild mitochondrial uncoupling. Mild mitochondrial uncoupling during the trigger phase of preconditioning may represent a common characteristic of mitochondria in a “conditioned” state.7,25-27 The involvement of mKCa channels in morphine-induced preconditioning was addressed in our study.
We demonstrated here that ischemic- and morphine-induced preconditioning reduced the infarct size to a similar extent. The mKCa channel blocker, paxilline, abolished both effects, confirming the findings of others that ischemic preconditioning involves activation of mKCa channels. Furthermore, it supports our hypothesis that mKCa channels are involved in the trigger phase of morphine-induced preconditioning. Heinen et al. showed that opening of mKCa channels can cause a slight increase in mitochondrial reactive oxygen species generation.28 The mKCa channel agonist, NS1619, requires superoxide radical generation during the preconditioning stimulus to induce a cardioprotective effect.29 Furthermore, these authors demonstrated that cardioprotection by NS1619 reduces mitochondrial calcium overload and mitochondrial reactive oxygen species production during the subsequent period of ischemia and early reperfusion.29 Such a reduction in mitochondrial calcium overload and reactive oxygen species generation has been suggested to prevent mPTP opening.30,31 Evidence suggests that the mKCa channel is located upstream of the mPTP, because cardioprotection induced by activation of mKCa channels was abolished by opening of the mPTP. Vice versa, inhibition of the mKCa channel with paxilline did not block protection induced by inhibition of the mPTP with cyclosporine A (CsA).8 Whether cardiac preconditioning by morphine is also mediated by regulation of the mPTP due to mKCa channel activation is yet unknown.
The results of the present study have to be interpreted within the scope of some limitations. First, we did not investigate possible upstream mechanisms of mKCa channels. Opioid receptors are G-protein coupled receptors whose activation inhibits adenylyl cyclase. The post-receptor signalling following opioid receptor activation has not been well defined. We cannot rule out that morphine confers preconditioning via intracellular pathways leading to activation of mKCa channels. However, the means by which morphine regulates mKCa channel activation to induce preconditioning is unknown. It has been shown that mKCa channel activation is involved in desflurane preconditioning and that protein kinase A (PKA) is located upstream of the mKCa channel.32 The activity of PKA as a possible upstream activator of KCa channels depends on the cellular level of cyclic adenosine monophosphate (cAMP)—PKA is known as cAMP-dependent protein kinase. Gross et al. demonstrated that morphine-induced cardioprotection involves glycogen synthase kinase-3beta (GSK3beta) and Akt (also called PKB).33 However, we did not investigate in the present study whether these enzymes are related to mKCa channels.
Another limitation of our study is that we did not determine the effect of ischemic and morphine preconditioning on the mitochondria. Xi et al. could show that morphine prevents mPTP opening by inactivation of GSK3beta.34 Our results showing that morphine confers preconditioning through activation of mKCa channels and the fact that enzymes like PKA regulate mKCa channel activation suggest future directions for investigating the underlying mechanism of morphine-induced cardioprotection. Clinically, morphine might be administered to patients who are subjected to organ ischemia (vascular surgery, organ transplantation, cardiac surgery) or who recently underwent regional ischemia (stroke, angina pectoris, myocardial infarction, organ transplantation) without the side-effect of being “anesthetized”. Furthermore, there is no κ-opioid agonist for clinical practice available. Therefore, unravelling the exact mechanisms of morphine-induced cardioprotection might have clinical consequences.
In summary, our results demonstrate that, besides ischemic preconditioning, morphine also initiates cardiac preconditioning via activation of mKCa channels.
References
Ferdinandy P, Schulz R, Baxter GF. Interaction of cardiovascular risk factors with myocardial ischemia/reperfusion injury, preconditioning, and postconditioning. Pharmacol Rev 2007; 59: 418-58.
Gross GJ. Role of opioids in acute and delayed preconditioning. J Mol Cell Cardiol 2003; 35: 709-18.
Cohen MV, Yang XM, Liu GS, Heusch G, Downey JM. Acetylcholine, bradykinin, opioids, and phenylephrine, but not adenosine, trigger preconditioning by generating free radicals and opening mitochondrial K(ATP) channels. Circ Res 2001; 89: 273-8.
Hausenloy DJ, Maddock HL, Baxter GF, Yellon DM. Inhibiting mitochondrial permeability transition pore opening: a new paradigm for myocardial preconditioning? Cardiovasc Res 2002; 55: 534-43.
Murphy E, Steenbergen C. Preconditioning: the mitochondrial connection. Annu Rev Physiol 2007; 69: 51-67.
Shintani Y, Node K, Asanuma H, et al. Opening of Ca2 + -activated K + channels is involved in ischemic preconditioning in canine hearts. J Mol Cell Cardiol 2004; 37: 1213-8.
Xu W, Liu Y, Wang S, et al. Cytoprotective role of Ca2 + - activated K + channels in the cardiac inner mitochondrial membrane. Science 2002; 298: 1029-33.
Cao CM, Xia Q, Gao Q, Chen M, Wong TM. Calcium-activated potassium channel triggers cardioprotection of ischemic preconditioning. J Pharmacol Exp Ther 2005; 312: 644-50.
Cao CM, Chen M, Wong TM. The K(Ca) channel as a trigger for the cardioprotection induced by kappa-opioid receptor stimulation–its relationship with protein kinase C. Br J Pharmacol 2005; 145: 984-91.
Martin WR. Pharmacology of opioids. Pharmacol Rev 1983; 35: 283-323.
Trescot AM, Helm S, Hansen H, et al. Opioids in the management of chronic non-cancer pain: an update of American Society of the Interventional Pain Physicians’ (ASIPP) Guidelines. Pain Physician 2008; 11: S5-62.
Liang BT, Gross GJ. Direct preconditioning of cardiac myocytes via opioid receptors and KATP channels. Circ Res 1999; 84: 1396-400.
Heinen A, Huhn R, Smeele KM, et al. Helium-induced preconditioning in young and old rat heart: impact of mitochondrial Ca(2 +) -sensitive potassium channel activation. Anesthesiology 2008; 109: 830-6.
Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation 1986; 74: 1124-36.
Cason BA, Gamperl AK, Slocum RE, Hickey RF. Anesthetic-induced preconditioning: previous administration of isoflurane decreases myocardial infarct size in rabbits. Anesthesiology 1997; 87: 1182-90.
Mullenheim J, Ebel D, Frassdorf J, et al. Isoflurane preconditions myocardium against infarction via release of free radicals. Anesthesiology 2002; 96: 934-40.
Schultz JE, Hsu AK, Gross GJ. Morphine mimics the cardioprotective effect of ischemic preconditioning via a glibenclamide-sensitive mechanism in the rat heart. Circ Res 1996; 78: 1100-4.
Sato T, Saito T, Saegusa N, Nakaya H. Mitochondrial Ca2 + -activated K + channels in cardiac myocytes: a mechanism of the cardioprotective effect and modulation by protein kinase A. Circulation 2005; 111: 198-203.
Wang X, Yin C, Xi L, Kukreja RC. Opening of Ca2 + -activated K + channels triggers early and delayed preconditioning against I/R injury independent of NOS in mice. Am J Physiol Heart Circ Physiol 2004; 287: H2070-7.
Kaczorowski GJ, Knaus HG, Leonard RJ, McManus OB, Garcia ML. High-conductance calcium-activated potassium channels; structure, pharmacology, and function. J Bioenerg Biomembr 1996; 28: 255-67.
Munujos P, Knaus HG, Kaczorowski GJ, Garcia ML. Cross-linking of charybdotoxin to high-conductance calcium-activated potassium channels: identification of the covalently modified toxin residue. Biochemistry 1995; 34: 10771-6.
Wallner M, Meera P, Ottolia M, et al. Characterization of and modulation by a beta-subunit of a human maxi KCa channel cloned from myometrium. Receptors Channels 1995; 3: 185-99.
Hu H, Shao LR, Chavoshy S, et al. Presynaptic Ca2 + -activated K + channels in glutamatergic hippocampal terminals and their role in spike repolarization and regulation of transmitter release. J Neurosci 2001; 21: 9585-97.
Sanchez M, McManus OB. Paxilline inhibition of the alpha-subunit of the high-conductance calcium-activated potassium channel. Neuropharmacology 1996; 35: 963-8.
Liem DA, Manintveld OC, Schoonderwoerd K, et al. Ischemic preconditioning modulates mitochondrial respiration, irrespective of the employed signal transduction pathway. Transl Res 2008; 151: 17-26.
Ljubkovic M, Mio Y, Marinovic J, et al. Isoflurane preconditioning uncouples mitochondria and protects against hypoxia-reoxygenation. Am J Physiol Cell Physiol 2007; 292: C1583-90.
Minners J, Lacerda L, McCarthy J, et al. Ischemic and pharmacological preconditioning in Girardi cells and C2C12 myotubes induce mitochondrial uncoupling. Circ Res 2001; 89: 787-92.
Heinen A, Camara AK, Aldakkak M, Rhodes SS, Ries ML, Stowe DF. Mitochondrial Ca2 + -induced K + influx increases respiration and enhances ROS production while maintaining membrane potential. Am J Physiol Cell Physiol 2007; 292: C148-56.
Stowe DF, Aldakkak M, Camara AK, et al. Cardiac mitochondrial preconditioning by Big Ca2 + -sensitive K + channel opening requires superoxide radical generation. Am J Physiol Heart Circ Physiol 2006; 290: H434-40.
Halestrap AP, Clarke SJ, Khaliulin I. The role of mitochondria in protection of the heart by preconditioning. Biochim Biophys Acta 2007; 1767: 1007-31.
Lim SY, Davidson SM, Hausenloy DJ, Yellon DM. Preconditioning and postconditioning: the essential role of the mitochondrial permeability transition pore. Cardiovasc Res 2007; 75: 530-5.
Redel A, Lange M, Jazbutyte V, et al. Activation of mitochondrial large-conductance calcium-activated K + channels via protein kinase A mediates desflurane-induced preconditioning. Anesth Analg 2008; 106: 384-91.
Gross ER, Hsu AK, Gross GJ. The JAK/STAT pathway is essential for opioid-induced cardioprotection: JAK2 as a mediator of STAT3, Akt, and GSK-3 beta. Am J Physiol Heart Circ Physiol 2006; 291: H827-34.
Xi J, Tian W, Zhang L, Jin Y, Xu Z. Morphine prevents the mitochondrial permeability transition pore opening through NO/cGMP/PKG/Zn2 +/GSK-3beta signal pathway in cardiomyocytes. Am J Physiol Heart Circ Physiol 2010; 298: H601-7.
Financial support
This study was supported by institutional and departmental sources. This work is part of Corinna Niersmann’s MD thesis.
Conflicts of interest
None declared.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Fräßdorf, J., Huhn, R., Niersmann, C. et al. Morphine induces preconditioning via activation of mitochondrial KCa channels. Can J Anesth/J Can Anesth 57, 767–773 (2010). https://doi.org/10.1007/s12630-010-9325-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-010-9325-1