Abstract
Purpose
The purpose of this article is to review the effective options for the reversal of vitamin K antagonists (warfarin and it coumarin analogues) and to help identify the option best suited for the patient requiring urgent surgery.
Principal findings
Vitamin K antagonists, the mainstay in long-term anticoagulation therapy, can be reversed with the administration of vitamin K, frozen plasma (FP), recombinant factor VIIa (rFVIIa), or the recently approved four-factor prothrombin complex concentrate (PCC), Octaplex®. While there is little evidence to suggest a superiority of PCC over FP, the availability of PCC in Canada is an important therapeutic addition requiring a thorough understanding of its pharmacology and risk benefit profile for the reversal of vitamin K antagonists. The use of PCC in the management of microvascular bleeding should be limited to very specific indications and should not be indicated in the routine management of massive blood loss.
Conclusions
In order to limit the blood loss associated with surgery and the management of uncontrolled bleeding, PCC is an important addition to our therapeutic armamentarium in the reversal of vitamin K antagonists.
Résumé
Objectif
L’objectif de cet article est de passer en revue les méthodes efficaces pour neutraliser l’effet des antagonistes de la vitamine K (analogues de la warfarine et de la coumarine) et d’aider à déterminer la meilleure option pour un patient nécessitant une chirurgie urgente.
Constatations principales
L’effet des antagonistes de la vitamine K, l’élément principal de la thérapie d’anticoagulation à long terme, peut être neutralisé par l’administration de vitamine K (po, iv), de plasma congelé (PC), de facteur recombinant VIIa (rFVIIa), ou de concentré de complexe prothrombique (CCP) à quatre facteurs, l’Octaplex®, qui a été autorisé récemment. Bien que nous n’ayons que peu de données suggérant la supériorité du CCP sur le PC, la disponibilité du CCP au Canada constitue un ajout thérapeutique majeur qui nécessite une compréhension minutieuse de sa pharmacologie et de son profil risque-bénéfice dans la neutralisation de l’effet des antagonistes de la vitamine K. L’utilisation du CCP pour la prise en charge des saignements microvasculaires devrait se limiter à des indications très spécifiques et ne devrait pas être indiquée pour la prise en charge de routine des pertes sanguines massives.
Conclusion
Le CCP est un ajout important à notre arsenal thérapeutique pour la neutralisation de l’effet des antagonistes de la vitamine K. Il permet de limiter les pertes sanguines associées à la chirurgie et de prendre en charge des saignements incontrôlés.
Similar content being viewed by others
In spite of the development of novel oral factor Xa and thrombin inhibitors,1,2 the vitamin K antagonists (VKA) continue to be the mainstay of long-term anticoagulation for patients with prosthetic heart valves, atrial fibrillation, a history or risk of deep vein thrombosis, or other thromboembolic events.3 The efficacy of the VKA is supported by extensive evidence, yet their narrow therapeutic index and the risk of major bleeding with urgent surgery requires an understanding of their pharmacology and awareness of the options for reversal of their anticoagulant effects.3 The best option for reversal depends on the clinical circumstances, particularly the time interval to surgery and the rate of bleeding.
In May 2007, a single prothrombin complex concentrate (PCC), Octaplex®, was approved by Health Canada for the urgent reversal of VKA anticoagulation. This PCC is distributed by the Canadian Blood Services and HemaQuebec, but the National Advisory Committee on Blood and Blood Products has recommended that the use of PCC should be guided by hospital guidelines, “Due to inventory concerns, lack of strong randomized control trial evidence of efficacy and the potential for thrombotic complications ……”Footnote 1 To support this intention, we reviewed the pharmacology of the VKA and the options for reversal of their anticoagulant effects, including the use of oral vitamin K, intravenous vitamin K, frozen plasma (FP),Footnote 2 recombinant factor VIIa (rFVIIa), and PCC. In addition, we considered the off-label use of PCC and the potential risks and complications associated with their use.
Warfarin
The coumarin analogues inhibit the production of the procoagulant proteins, factors II, VII, IX, and X (FII, FVII, FIX, and FX). They were first identified in the late 1930’s as the cause of a hemorrhagic disorder in cattle after the ingestion of fermented sweat clover.4,5 Warfarin is the most commonly prescribed coumarin derivative in North America, but other coumarin analogues share the same mechanism of action while differing in potency and duration of action.
The vitamin K dependent coagulation factors are synthesized as inactive precursor forms requiring carboxylation of the amino-terminal glutamate residues by gamma (δ) carboxylase (Figure 1). This carboxylation allows for the binding of Ca2+, hence, activation of these serine proteases. The protein carboxylation is directly coupled with the oxidation of vitamin K to the corresponding epoxide. The vitamin K epoxide can be reused as a cofactor for δ-carboxylase if it is returned to its reduced form by vitamin K oxide reductase (VKOR). The supply of cofactor vitamin K is limited in the diet; therefore, the generation of carboxylated clotting factors is limited if the reduction of the vitamin K epoxide is prevented by VKA.6
Mechanism of action and warfarin. Vitamin K dependent carboxylation of the precursor coagulation proteins (factors II, VII, IX, X, protein C, and S) allows for the binding of calcium (Ca 2+) and, therefore, the activation of these proteins. This protein carboxylation results in the formation of vitamin K epoxide (oxidized) that cannot participate in protein carboxylation unless it is returned to its reduced form by vitamin K oxide reductase (VKOR). Warfarin binds to VKOR and prevents this reduction of the vitamin K epoxide, thereby limiting the amount of vitamin K available to act as the co-factor for protein carboxylation. The administration of exogenous vitamin K can bypass the effects of warfarin and serve as a co-factor for protein carboxylation
Although the VKA antagonists were recognized to be structurally similar to vitamin K, their intracellular target, VKOR, and its gene, vitamin K epoxide complex subunit 1 (VKORC1), were only recently described.7,8 The gene for VKOR encodes for several isoforms of the protein with varying sensitivities to the VKA inhibition. As a result of VKA inhibition of VKOR, the liver synthesizes partially carboxylated and de-carboxylated proteins with reduced activity, but clot formation is not completely inhibited. The introduction of vitamin K in the diet or its administration will replenish the depleted levels of the reduced vitamin, bypassing the VKA inhibition of VKOR and restoring the formation of carboxylated active clotting factors (Figure 1). These vitamin K dependent factors are present as precursor proteins and only require carboxylation to complete their synthesis; hence, reversal of VKA with vitamin K is prompt and does not require de novo protein synthesis.
Warfarin, a racemic mixture, is well absorbed orally and highly protein bound, limiting its apparent volume of distribution.4 Peak serum concentration is attained in 90 min with a serum half-life of 36 to 42 hr. S-Warfarin is the more active isomer cleared by cytochrome P450 2C9 (CYP2C9), and its inactive hydroxylated metabolites are eliminated in the urine.5 The less active R-isomer is cleared by a different series of cytochromes P450 (CYP1A2, CYP3A4).
Although the serum half-life of warfarin is approximately 40 hr, its functional duration of effect is two to five days. The duration of action of warfarin is highly variable, as CYP2C9 is also responsible for the metabolism of a wide variety of exogenous substrates that can alter the metabolism of warfarin (Table 1).Footnote 3 , 9 Furthermore, 30 CYP2C9 alleles are recognized, three of which result in a slower elimination of warfarin and a greater sensitivity to its effects.5
Risks and side effects
Warfarin has an exceptionally narrow therapeutic index with significant morbidity and mortality with over or under treatment, i.e., bleeding or thromboembolic complications. Its metabolism can be increased or decreased by numerous medications, foods, and alcohol, but the evidence to support the clinical consequences of these interactions is limited.9 Warfarin co-administration with azole antibiotics, macrolides, quinolones, non-steroidal anti-inflammatory drugs, serotonin uptake inhibitors, lipid lowering agents, amiodarone, and fluoruracil should be done only with close monitoring.9,10
From 0.4 to 2.0% of patients require transfusion, hospitalization, or surgery due to bleeding caused by warfarin toxicity. This outcome is given as one of the most common reasons sited for the underutilization of warfarin anticoagulation.3,11 While warfarin-induced bleeding may be the indication for surgery, e.g., intra-cerebral hemorrhage (ICH) or gastrointestinal bleeding, the more common preoperative concern is excessive surgical blood loss or perioperative complications in patients with an elevated prothrombin time (PT) or normalized PT known as the international normalized ratio (INR). The therapeutic options for reversal depend on the risk of bleeding from the procedure, the degree of INR elevation, and the clinical urgency of the surgical procedure.
Monitoring
The INR reflects the level of three of the four vitamin K dependent procoagulant proteins, FII, FVII, and FX. Due to the difference in the half-life of the vitamin K dependent proteins (FVII t1/2 = 2-9 hr; FX t1/2 = 17-44; and FII t1/2 60-72 hr), the changes in the PT/INR with the initiation or discontinuation of warfarin will reflect changes in the concentration of FVII, then FX, and finally FII.3 The mean effective half-life of warfarin is approximately 40 hr; therefore, the INR should return to normal range within five to ten days after being discontinued without the administration of vitamin K.12
Preoperative VKA reversal
Many surgical procedures, such as ophthalmic procedures (cataract extractions and trabeculectomies),13 dental procedures,13,14 low risk endoscopic procedures,13,15 arthrocentesis,13 and minor dermatological procedures15 entail a low risk of surgical bleeding, and warfarin reversal, while controversial, may not be indicated (Table 2). In addition, while VKA reversal has been customary for diagnostic procedures, such as lung and liver biopsy, this practice has been challenged, and withholding VKA to obtain an INR of < 2.0 may be sufficient.16
When reversal of warfarin anticoagulation is indicated, the clinician must decide on a target INR. Most surgical procedures can be performed safely with an INR of ≤ 1.5, and this corresponds to coagulation factor levels of approximately 50% of normal.17
Options for the reversal of VKA
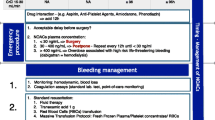
The appropriate option for the reversal of VKA anticoagulation depends on the time permitted before surgery, the ability to assess and control blood loss, the risk of injury (e.g., neurological injury), and the need for anti-coagulation after the surgical procedure (Table 3). For surgery that is required within six to 24 hr, intravenous vitamin K should be considered, with a repeat INR prior to surgery in sufficient time to act on the result if required. For emergency surgery within less than six hours or in patients with on-going blood loss, the options include intravenous vitamin K (5-10 mg iv) in conjunction with FP, rFVIIa or PCC.3
Vitamin K
Vitamin K in the urgent reversal of warfarin therapy acts by increasing endogenous synthesis of functional coagulation factors (Figure 1). Importantly, vitamin K administration does not reverse the VKOR inhibition, but rather, it bypasses this enzymatic reaction providing a source of reduced vitamin K to allow for the δ-carboxylation of the precursor coagulation proteins. Occasionally, vitamin K administration may need to be repeated until the inhibition of VKOR has been reversed by the elimination of the VKA.
Vitamin K is available in numerous formulations and can be administered by several routes, including oral, subcutaneous, intramuscular, and intravenous. For the urgent VKA reversal, the intravenous route is the most rapid approach, leading to a substantial reduction of the INR within four to six hours.18,19 There is a small risk of an allergic reaction in the form of an anaphylactoid reaction (3 in 10,000), but this should not preclude this route of administration, particularly in the bleeding or surgical population.20,21 Many of the allergic reactions associated with vitamin K in the past may well have been better attributed to the use of polyethoxylated castor oil preservative (cremophor) and the rate of administration (intravenous push). Vitamin K should be administered as a slow infusion over 30 min, where possible. The subcutaneous and intramuscular route, in addition to its unpredictable onset, leaves an area of induration and is not recommended for reversal of oral VKAs.22 However, the subcutaneous route is used in neonatalogy and severe liver disease and serves as a vitamin K depot.6
Frozen plasma
Frozen plasma is a good source of coagulation factor replacement for the reversal of VKA, and although Canadian standards require it to be used within 24 hr of thawing or it must be discarded, the activity of the coagulation factors is stable for more than six days when stored at 6°C.23 However, FP has several important limitations. First, prior to the administration of FP, there is a delay needed to test for pre-transfusion ABO blood group compatibility, to thaw the product (20-30 min), and to infuse the product safely in order to minimize the risk of fluid overload. In addition, the requisite dose (a single dose equal to 15 mL·kg−1) calls for large volumes (750-1750 mL), particularly if the targeted INR is < 1.5.24 In most cases, a single dose of FP is thought to contain approximately 1,000 international units (IU) of the vitamin K dependent factors, enough to increase factor levels by an estimated 20%.
In addition to treatment delays and the risk of fluid overload, FP is also associated with an underlying risk of transfusion-transmitted infections and transfusion-related acute lung injury (TRALI) and anaphylaxis. The risk of TRALI with FP transfusion has been historically reported at 1 in 5,000 components transfused. However, reports to United Kingdom’s hemovigilance program, Severe Hazards of Transfusion (SHOT), suggest a 50% reduction in risk of TRALI with the use of FP that is predominantly (99%) derived from male donors.Footnote 4 Due to supply issues with AB plasma, the universal plasma donor, the plasma from female donors must be retained; thus, risk of TRALI remains higher with this ABO blood group.
Dilution of red blood cell (RBC) concentration can lead to a significant decrease in hemoglobin concentration prompting RBC transfusion by the clinical team. Furthermore, hemodilution may alter the rheological properties of the blood and, paradoxically, increase bleeding.25
Frozen plasma remains an acceptable method for the reversal of warfarin anticoagulation.3 It must be remembered that the duration of action of FP is limited by the brief survival of coagulation factors, and vitamin K should be administered concomitantly to stimulate the synthesis of endogenous coagulation factors (e.g., the half-life of FVII is five hours) and sustain warfarin reversal once the transient effect of FP is lost.
Recombinant FVIIa
Recombinant FVIIa is indicated in the control of hemorrhage in congenital hemophilia complicated by antibodies to the recombinant replacement FVIII and FIX.26 However, rFVIIa has been evaluated as a rescue agent in the case of massive bleeding in a wide variety of clinical situations, including warfarin reversal.3,26-29 Factor VIIa was recommended for warfarin reversal in the most recent American guidelines.3
Recombinant FVIIa (5 μg·kg−1) reverses the INR to within a normal range for 12 hr, while much higher doses (120 μg/kg) are required to prolong the correction of the INR for up to 24 hr.30 It must be kept in mind that the short half-life of rFVIIa (60-180 min) varies with the patient status and presence of on-going blood loss. Vitamin K supplementation should be co-administered.31
In a review of the available case series and case reports, Rosovsky and Crowther concluded that, while rFVIIa appears to rapidly reverse the abnormal INR, the clinical impact is difficult to ascertain due to small, poorly controlled trials in which conventional therapy, i.e., plasma and vitamin K therapy, was employed concomitantly.32 An in vitro comparison of the INR reversal with rFVIIa and PCC demonstrated greater clot stability with PCC. This was presumed to be due to the synthesis of thrombin-activatable fibrinolysis inhibitor (TAFI).33 In a rat model using tail tip bleeding, blood loss was greater with the rFVIIa than with the PCC despite similar correction of the aPTT and PT.34
On balance, given the lack of clinical experience, the greater risk of thromboembolic complications, and the substantial cost of rFVIIa (approximately $1,000 per mg), rFVIIa cannot be recommended for the preoperative VKA reversal.35
Prothrombin complex concentrate
Prothrombin complex concentrates are prepared as either three-factor PCC (FII, FIX, and FX) or four-factor PCC (FII, FVII, FIX, and FX). The three-factor PCC is recommended as an adjunct to plasma, and there is evidence to suggest that the three-factor PCC is not effective alone.36 Furthermore, with the exception of special access programs, it is unlikely that the three-factor PCC will be made available in Canada for the reversal of oral anticoagulation. Therefore, we restricted our attention to the available four-factor PCC products and refer to them as PCC. A review of all of the available PCC products is beyond the scope of this review; however, we have provided other references for a comparison of these products.37,38
There are two commonly used four-factor PCC products formulated and indicated for the reversal of VKA, i.e., Beriplex® (CSL Behring, Marburg, Germany) and Octaplex® (Octapharma, Vienna, Austria and Canada). These products have similar composition (Table 4),Footnote 5 , Footnote 6 but Beriplex® contains a small amount of anti-thrombin (2-15 IU) not found in Octaplex®. In addition, there is close to a ten-fold greater amount of heparin contained in Octaplex® than in Beriplex® (Octaplex® 80-310 IU and Beriplex® 8-40 IU), albeit a small non-therapeutic dose. Data comparing the safety and efficacy of Beriplex® with FP are pending and constitute a current impediment to the approval of Beriplex® by the FDA37 (clinicalTrials.gov numbers NCT00708435 NCT00803101). Octaplex® and Beriplex® are both available in Europe, Australia, and the United Kingdom.
There are no clinical studies comparing these two PCC preparations for safety or efficacy. The reader is cautioned that there are several publications regarding the reversal of VKA using factor concentrates indicated for use in hemophiliacs with higher concentration of FIX or activated factors, e.g., FEIBA (Baxter, USA). These latter products should be considered separately from the current discussion and are well summarized by Levy et al. 37 Our focus was on Octaplex®, since it is the only four-factor PCC product currently licensed for use in Canada, and we made comparisons and references to Beriplex® where appropriate.
Pharmacology
Due to the concentrated nature of factors in PCC (25-fold that in plasma), the volume infused is approximately 40-80 mL (each 500 IU of lyophilized product is reconstituted in 20 mL of sterile water), which is much lower than for FP. So far, the optimum dose of PCC has not been established, and the manufacturer’s dose recommendations are higher than those of the National Advisory Committee on Blood and Blood Products. Factor activity is expressed in international units (IU) and relates to FIX activity within the PCC preparation. Each vial contains approximately 500 IU of each of the vitamin K dependent coagulation factors, plus protein C and S and a small amount of heparin (Table 4).
No thawing or blood ABO grouping is required prior to administration. Prothrombin complex concentrate is a lyophilized product which is supplied as a powder with sterile water provided for reconstitution for intravenous injection. The reconstituted solution should be colourless to slightly blue, and strict aseptic techniques should be employed. The reconstitution of the product requires a review of the product preparation instructions contained within the product insert. Some transfusion medicine services in Canada issue the product in a lyophilized form, while others reconstitute the complete dose and issue in a mini-bag for immediate infusion. To minimize the risk of thromboembolic complications, each 1,000 IU of Octaplex® should be administered over 15 min by slow infusion.
Octaplex® can be stored at room temperature (+2 to +25°C) and should be protected from light exposure. It has a two-year shelf life, but should be used immediately (within 12 hr) or discarded once reconstitution has occurred.
Dosage and efficacy
Classical dosing studies with PCC have not been performed due to the human origin of the product. Dosing depends on the clinical situation, particularly the extent of bleeding and patient status. In their prospective multi-centre descriptive trial, Riess et al. demonstrated that the perioperative physician could effectively correct INR to predetermined levels by individually dosing PCC.39 In their review of the available evidence (14 published studies), Leissinger et al. pointed out that the majority of the evidence comes from prospective non-randomized trials or retrospective observational studies.40 Differing indications for treatment and the off-label use of these products further complicates any conclusion to be drawn from these trials. Despite these short-comings, PCC has been recommended for urgent reversal of warfarin.3,41,42
While the correction of the INR is a surrogate outcome, there is some, albeit limited, data to suggest that PCC may reverse the anticoagulation more rapidly and, therefore, the bleeding associated with VKA toxicity. In a retrospective single centre study, the use of PCC alone or in combination with vitamin K was associated with a reduced incidence and extent of ICH hematoma growth compared with FP alone or in combination with vitamin K.43 While this study included a small population (n = 55), an association between early (i.e., within two hours) normalization of INR and the prevention of hematoma growth in both the FP- and PCC-treated groups supports the use of INR as an outcome to compare the efficacy of these treatment options.
The current dosing recommendations from the National Advisory Committee on Blood and Blood Products are for PCC 1,000 IU (Octaplex® 40 mL, two vials) with consideration for a second dose for supratherapeutic INR or extremes of patient weight (maximum dose 3,000 IU).Footnote 7 Consideration of the starting INR and the patient’s weight is known to improve the efficacy of INR reversal.44 An upper dose of 30 IU·kg−1 and a lower dose of 8.8 IU·kg−1 are supported by limited clinical data.45,46 The Canadian recommendation is for 10-12 IU·kg−1 for INR less than 3.0.A This dosing guideline is approximately one-third of the dose recommended in the product monographs, but was selected to balance the risk-benefit profile of the treatment. A PCC utilization review from Northern Alberta found that the recommended dose successfully corrected the INR to < 1.5 in 75% of cases.47 Many hospitals in Canada utilize a higher dose if the INR exceeds 3.0-4.0 or if the patient weighs more than 90 kg (Hospital Guidelines, University Health Network and Sunnybrook Health Science Centre, Toronto, Ontario).
To date, there are no randomized controlled trials comparing FP and PCC. However, there have been several small trials in patients with intra-cerebral hemorrhages that demonstrate a more complete reversal of the INR with PCC.48,49 In addition, PCC may be a more reliable source of FIX that is not assessed with the PT/INR test and yet may be particularly important in hemostasis.50 Until now, evidence of improved outcomes or better control of bleeding risk is unavailable, but data may be available on the completion of the FDA required studies comparing FP with Beriplex® for patients with major bleeding due to warfarin toxicity.
The effects of PCC on coagulation lasts six to eight hours in the absence of major blood loss, and as discussed above, the effects of vitamin K administered concomitantly should start within 4-6 hours; therefore, repeat dosing is usually not required. For the urgent reversal of oral anticoagulation, most guidelines, including the American College of Physicians and the British, recommend the concomitant use of intravenous vitamin K 5-10 mg.3,41,42 While the use of smaller doses of vitamin K have been recommended in the management of patients on VKA, the objective in the bleeding patient or the patient scheduled for urgent surgery is to ensure reversal of the anti-coagulant effects; therefore, the higher doses of vitamin K are recommended.
Contra-indications
Octaplex® is contraindicated in patients who are hypersensitive to any of its constituents, particularly those patients with a history of heparin-induced thrombocytopenia (HIT), as the product contains a small amount of heparin (Table 4). In addition, PCC should be avoided in cases of dissemination intravascular coagulation (DIC) or anti-thrombin (AT) deficiency, as the PCC may add to the thromboembolic risk associated with these situations (Table 5). The use of PCC in patients with a history of recent thromboembolic events (< two weeks) or a recent myocardial infarction is relatively contraindicated and should only be used after careful consideration of the potential risks and benefits.
Prothrombin complex concentrate is not recommended as a treatment for coagulopathies associated with massive blood transfusion or sepsis.51 Clinical safety has not been established in pregnancy, in the early postpartum period, and in pediatrics.
Toxicity/risk
Octaplex® is a human plasma-derived product from up to 1,500 screened plasma donors. While products derived from human plasma have a risk of infectious transmission that cannot be eliminated, this PCC is solvent-detergent treated and nanofiltered. These measures are considered effective for the encapsulated viruses, i.e., human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV), but their effectiveness is limited against the non-encapsulated viruses, such as hepatitis A (HAV) or parvovirus B19. In addition, the product undergoes a prion protein reduction process that has been assessed to have a removal log of 5.18 log10. While the clinical importance of this is difficult to ascertain, the transmission of variant Creutzfeldt-Jakob Disease in hemophiliac patients treated with factor concentrates has been reported.52 Importantly, Octaplex® is a blood product with an infectious risk profile similar to other manufactured blood products, such as albumin.
In addition to the infectious risks, PCC carries a risk of DIC and thromboembolic complications and may worsen DIC by serving as a substrate for the on-going consumptive coagulopathy. The inclusion of the anticoagulant factors, proteins C and S, is believed to balance its pro-coagulant properties and limit the thromboembolic risk. There are case reports of thromboembolic events following the administration of PCC;53,54 however, it is difficult to assign the PCC as the cause of a thrombotic complication when it is being used to reverse VKA anticoagulation in patients at increased risk of thromboembolic events.
Potential rare complications include the generation of an autoimmune response to one of the vitamin K dependent coagulation factors and anaphylaxis.
Cost of PCC and FP
It is difficult to establish the relative cost of PCC compared with FP, as the cost of FP varies with product availability and source. Even if we assume the cost of the products themselves to be similar, e.g., $1,000 per 1,000 IU of PCC or 750-1750 mL of FP, there are many other costs more difficult to delineate. Unused FP has value because it can be used as a plasma source for manufacturing albumin and intravenous immunoglobulin to assist Canada in becoming more self-sufficient rather than relying on a US plasma source. Furthermore, there are cost implications associated with FP for the urgent reversal of VKA, when PCC may be more effective and associated with fewer side effects or complications such as TRALI. Without doubt, the use of PCC or FP should be discouraged when vitamin K would be sufficient, i.e., the non-urgent use of these products.
Off-label use of PCC
In Canada, the indication for PCC is the treatment of ongoing bleeding and perioperative prophylaxis for bleeding in acquired deficiency of the prothrombin coagulation factors, such as the deficiency caused by treatment with VKA.Footnote 8 The off-label use of PCC must be cautioned against, but at the same time, we should recognize this as an important concern for this product and for those involved in the perioperative management of the bleeding patient. Monitoring the efficacy and adverse affects of PCC, as with the off-label use of any therapeutic modality, may be the first and, in some cases, the only evidence available for its use, and it is the responsibility of both practitioners and facilities where the off-label use of PCC is deemed necessary.
Massive hemorrhage is the first off-label indication considered for the use of PCC. While, DIC and AT deficiency must be excluded prior to its use, PCC may be indicated when volume overload or severe right ventricular dysfunction renders the use of FP impossible. It must be remembered that PCC is not a replacement for FP, as it is does not contain many of the constituents of FP known to play a role in homeostasis, such as fibrinogen or FXIII.
In a porcine model, the combination of fibrinogen and PCC reversed a dilutional coagulopathy assessed with thromboelastography and substantially reduced blood loss following a traumatic liver injury.55 In a similar animal model, PCC, but not FP, fully reversed the effects of a dilutional coagulopathy on PT and reduced blood loss resulting from both bone and soft tissue injury.56 Prothrombin complex concentrate has been used in cardiac and non-cardiac surgical patients to treat microvascular bleeding that does not respond to factor replacement therapy with FP and platelets.51,57 However, we need to be very clear that PCC contains only the vitamin K dependent clotting factors, and, unlike FP, it does not contain all of the essential components of the clotting cascade.
The use of PCC as a relatively inexpensive substitute for rFVIIa cannot be justified. In the off-label use of rFVIIa, the most conservative dose recommendation (15-30 μg·kg−1) increased FVIIa to nmolar concentration range and increased the measured activity of FVII by 50- to 100-fold.31 In contrast, even with the highest dose of PPC recommended (3,000 IU), the target is the replacement of coagulation factors, and the maximum levels of FVII would increase by two- to three-fold, far from the pharmacological doses provided with the off-label use of rFVIIa.31,39
Summary
Despite a narrow therapeutic index and the need for frequent blood testing, warfarin and the coumarin analogues are likely to remain the mainstay of oral anticoagulation therapy. Whenever possible, the reversal of warfarin anticoagulation should be done electively under close medical supervision. However, in order to limit the blood loss associated with urgent surgery and the management of uncontrolled bleeding, PCC is an important addition to our therapeutic armamentarium. Similar to many therapeutic dilemmas, it is essential to have a thorough understanding of the treatment options for the reversal of VKA and the indications for PCC.
Notes
The term frozen plasma is used to denote plasma frozen within 24 hours of collection in contrast to fresh frozen plasma, which is frozen within six hours of collection.
http://www.shotuk.org/SHOT%20Report%202008.pdf (accessed September 1, 2009).
Product Monograph, Octaplex®, Octapharma Canada Inc. Control # 116440 (approved December 3, 2007).
Product Monograph, Beriplex®P/N, CSL Behring UK Limited (updated April 3, 2009).
http://www.shotuk.org/SHOT%20Report%202008.pdf (accessed September 1, 2009).
References
De Caterina R, Kristensen SD, Renda G. New anticoagulants for atrial fibrillation. J Cardiovasc Med (Hagerstown) 2009; 10: 446-53.
Spyropoulos AC. Brave new world: the current and future use of novel anticoagulants. Thromb Res 2008; 123(Suppl 1): S29-35.
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. American College of Chest Physicians. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(6 Suppl): 160S-98S.
Majerus PW, Tollefsen DM. Blood coagulation and anticoagulant, thrombolytic and antiplatelet drugs. In: Brunton LL, Lazo J, Parker K, editors. Goodman and Gilman’s Pharmacological Basis of Therapeutics, 11th ed. New York: McGraw-Hill, Medical Publishing Division; 2006.
Hill CE, Duncan A. Overview of pharmacogenetics in anticoagulation therapy. Clin Lab Med 2008; 28: 513-24.
Shearer MJ. Vitamin K. Lancet 1995; 345: 229-34.
Whitlon DS, Sadowski JA, Suttie JW. Mechanism of coumarin action: significance of vitamin K epoxide reductase inhibition. Biochemistry 1978; 17: 1371-7.
Li T, Chang CY, Jin DY, Lin PJ, Khvorova A, Stafford DW. Identification of the gene for vitamin K epoxide reductase. Nature 2004; 427: 541-4.
Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med 2005; 165: 1095-106.
Wells PS, Holbrook AM, Crowther NR, Hirsh J. Interactions of warfarin with drugs and food. Ann Intern Med 1994; 121: 676-83.
Garcia DA, Regan S, Crowther M, Hylek EM. The risk of hemorrhage among patients with warfarin-associated coagulopathy. J Am Coll Cardiol 2006; 47: 804-8.
McMillian WD, Rogers FB. Management of prehospital antiplatelet and anticoagulant therapy in traumatic head injury: a review. J Trauma 2009; 66: 942-50.
Dunn AS, Turpie AG. Perioperative management of patients receiving oral anticoagulants: a systematic review. Arch Intern Med 2003; 163: 901-8.
Wahl MJ. Dental surgery in anticoagulated patients. Arch Intern Med 1998; 158: 1610-6.
Veitch AM, Baglin TP, Gershlick AH, Harnden SM, Tighe R. Cairns S; British Society of Gastroenterology; British Committee for Standards in Haematology; British Cardiovascular Intervention Society. Guidelines for the management of anticoagulant and antiplatelet therapy in patients undergoing endoscopic procedures. Gut 2008; 57: 1322-9.
Abdel-Wahab OI, Healy B, Dzik WH. Effect of fresh-frozen plasma transfusion on prothrombin time and bleeding in patients with mild coagulation abnormalities. Transfusion 2006; 46: 1279-85.
Ciavarella D, Reed RL, Counts RB, et al. Clotting factor levels and the risk of diffuse microvascular bleeding in the massively transfused patient. Br J Haematol 1987; 67: 365-8.
Watson HG, Baglin T, Laidlaw SL, Makris M, Preston FE. A comparison of the efficacy and rate of response to oral and intravenous vitamin K in reversal of over-anticoagulation with warfarin. Br J Haematol 2001; 115: 145-9.
Lubetsky A, Yonath H, Olchovsky D, Loebstein R, Halkin H, Ezra D. Comparison of oral vs intravenous phytonadione (vitamin K1) in patients with excessive anticoagulation: a prospective randomized controlled study. Arch Intern Med 2003; 163: 2469-73.
Riegert-Johnson DL, Volcheck GW. The incidence of anaphylaxis following intravenous phytonadione (vitamin K1): a 5-year retrospective review. Ann Allergy Asthma Immunol 2002; 89: 400-6.
Fiore LD, Scola MA, Cantillon CE, Brophy MT. Anaphylactoid reactions to vitamin K. J Thromb Thrombolysis 2001; 11: 175-83.
Dezee KJ, Shimeall WT, Douglas KM, Shumway NM, O’malley PG. Treatment of excessive anticoagulation with phytonadione (vitamin K): a meta-analysis. Arch Intern Med 2006; 166: 391-7.
von Heymann C, Keller MK, Spies C, et al. Activity of clotting factors in fresh-frozen plasma during storage at 4 degrees C over 6 days. Transfusion 2009; 49: 913-20.
Holland LL, Brooks JP. Toward rational fresh frozen plasma transfusion: the effect of plasma transfusion on coagulation test results. Am J Clin Pathol 2006; 126: 133-9.
Valeri CR, Cassidy G, Pivacek LE, et al. Anemia-induced increase in the bleeding time: implication for treatment of nonsurgical blood loss. Transfusion 2001; 41: 977-83.
Karkouti K, Beattie WS, Arellano R, et al. Comprehensive Canadian review of the off-label use of recombinant activated factor VII in cardiac surgery. Circulation 2008; 118: 331-8.
Karkouti K, Beattie WS, Crowther MA, et al. The role of recombinant factor VIIa in on-pump cardiac surgery: proceedings of the Canadian Consensus Conference. Can J Anesth 2007; 54: 573-82.
Boffard KD, Riou B, Warren B, et al. Recombinant factor VIIa as adjunctive therapy for bleeding control in severely injured trauma patients: two parallel randomized, placebo-controlled, double-blind clinical trials. J Trauma 2005; 59: 8-15.
Lodge JP, Jonas S, Oussoultzoglou E, et al. Recombinant coagulation factor VIIa in major liver resection: a randomized, placebo-controlled, double-blind clinical trial. Anesthesiology 2005; 102: 269-75.
Erhardtsen E, Nony P, Dechavanne M, Ffrench P, Boissel JP, Hedner U. The effect of recombinant factor VIIa (NovoSeven) in healthy volunteers receiving acenocoumarol to an international normalized ratio above 2.0. Blood Coagul Fibrinolysis 1998; 9: 741-8.
Klitgaard T, Nielsen TG. Overview of the human pharmacokinetics of recombinant activated factor VII. Br J Clin Pharmacol 2008; 65: 3-11.
Rosovsky RP, Crowther MA. What is the evidence for the off-label use of recombinant factor VIIa (rFVIIa) in the acute reversal of warfarin? ASH evidence-based review 2008. Hematology Am Soc Hematol Educ Program 2008: 36-8
Taketomi T, Szlam F, Levy JH, Tanaka KA. Warfarin reversal with prothrombin complex concentrate confers better antifibrinolytic activity compared with recombinant activated factor VII. Blood Coagul Fibrinolysis 2008; 19: 106-8.
Dickneite G. Prothrombin complex concentrate versus recombinant factor VIIa for reversal of coumarin anticoagulation. Thromb Res 2007; 119: 643-51.
O’Connell NM, Perry DJ, Hodgson AJ, O’Shaughnessy DF, Laffan MA, Smith OP. Recombinant FVIIa in the management of uncontrolled hemorrhage. Transfusion 2003; 43: 1711-6.
Holland L, Warkentin TE, Refaai M, Crowther MA, Johnston MA, Sarode R. Suboptimal effect of a three-factor prothrombin complex concentrate (profilnine-SD) in correcting supratherapeutic international normalized ratio due to warfarin overdose. Transfusion 2009; 49: 1171-7.
Levy JH, Tanaka KA, Dietrich W. Perioperative hemostatic management of patients treated with vitamin K antagonists. Anesthesiology 2008; 109: 918-26.
Samama CM. Prothrombin complex concentrates: a brief review. Eur J Anaesthesiol 2008; 25: 784-9.
Riess HB, Meier-Hellmann A, Motsch J, Elias M, Kursten FW, Dempfle CE. Prothrombin complex concentrate (Octaplex) in patients requiring immediate reversal of oral anticoagulation. Thromb Res 2007; 121: 9-16.
Leissinger CA, Blatt PM, Hoots WK, Ewenstein B. Role of prothrombin complex concentrates in reversing warfarin anticoagulation: a review of the literature. Am J Hematol 2008; 83: 137-43.
Baglin TP, Keeling DM, Watson HG. British Committee for Standards in Haematology. Guidelines on the oral anticoagulation (warfarin): third edition - 2005 update. Br J Haematol 2006; 132: 277-85.
Baker RI, Coughlin PB, Gallus AS, Harper PL, Salem HH, Wood EM. Warfarin Reversal Consensus Group. Warfarin reversal: consensus guidelines, on behalf of the Australasian Society of Thrombosis and Haemostasis. Med J Aust 2004; 181: 492-7.
Huttner HB, Schellinger PD, Hartmann M, et al. Hematoma growth and outcome in treated neurocritical care patients with intracerebral hemorrhage related to oral anticoagulant therapy: comparison of acute treatment strategies using vitamin K, fresh frozen plasma, and prothrombin complex concentrates. Stroke 2006; 37: 1465-70.
van Aart L, Eijkhout HW, Kamphuis JS, et al. Individualized dosing regimen for prothrombin complex concentrate more effective than standard treatment in the reversal of oral anticoagulant therapy: an open, prospective randomized controlled trial. Thromb Res 2006; 118: 313-20.
Evans SJ, Biss TT, Wells RH, Hanley JP. Emergency warfarin reversal with prothrombin complex concentrates: UK wide study. Br J Haematol 2008; 141: 268-9.
Yasaka M, Sakata T, Naritomi H, Minematsu K. Optimal dose of prothrombin complex concentrate for acute reversal of oral anticoagulation. Thromb Res 2005; 115: 455-9.
Onell R, Sahota P, larke G, Nahirniak S. Octaplex® utilization post NAC recommendations in northern Alberta - The first five months. Transfusion 2009; 49: 161A (SP289).
Makris M, Greaves M, Phillips WS, Kitchen S, Rosendaal FR, Preston EF. Emergency oral anticoagulant reversal: the relative efficacy of infusions of fresh frozen plasma and clotting factor concentrate on correction of the coagulopathy. Thromb Haemost 1997; 77: 477-80.
Cartmill M, Dolan G, Byrne JL, Byrne PO. Prothrombin complex concentrate for oral anticoagulant reversal in neurosurgical emergencies. Br J Neurosurg 2000; 14: 458-61.
Makris M. Optimisation of the prothrombin complex concentrate dose for warfarin reversal. Thromb Res 2005; 115: 451-3.
Bruce D, Nokes TJ. Prothrombin complex concentrate (Beriplex P/N) in severe bleeding: experience in a large tertiary hospital. Crit Care 2008; 12: R105.
Eaton L. Haemophilia patient had variant CJD agent in spleen. BMJ 2009; 338. DOI:10.1136/bmj.b705.
Warren O, Simon B. Massive, fatal, intracardiac thrombosis associated with prothrombin complex concentrate. Ann Emerg Med 2009; 53: 758-61.
White R, Rushbrook J, McGoldrick J. The dangers of prothrombin complex concentrate administration after heart surgery. Blood Coagul Fibrinolysis 2008; 19: 609-10.
Fries D, Haas T, Klingler A, Streif W, et al. Efficacy of fibrinogen and prothrombin complex concentrate used to reverse dilutional coagulopathy—a porcine model. Br J Anaesth 2006; 97: 460-7.
Dickneite G, Pragst I. Prothrombin complex concentrate vs fresh frozen plasma for reversal of dilutional coagulopathy in a porcine trauma model. Br J Anaesth 2009; 102: 345-54.
Stuklis RG, O’Shaughnessy DF, Ohri SK. Novel approach to bleeding in patients undergoing cardiac surgery with liver dysfunction. Eur J Cardiothorac Surg 2001; 19: 219-20.
Acknowledgements
We sincerely thank Willa Bradshaw, MScBMC, of Perioperative Interactive Education, Toronto General Hospital, Department of Anesthesia and Pain Management for the artwork and Drs. Christine Cserti, Yulia Lin, Keyvan Karkouti, Susan Nahirniak, and Jacob Pendergrast for their helpful discussions and support in the preparation of the manuscript.
Disclosure
Dr. S.A. McCluskey has received research grants and honoraria from Novo Nordisk.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article will be accompanied by an editorial. Please see Can J Anesth 2010; 57(5).
Dedicated to Dr. Kenneth Alan McCluskey, July 18, 1923-Oct 12, 2009.
Rights and permissions
About this article
Cite this article
Grobler, C., Callum, J. & McCluskey, S.A. Reversal of vitamin K antagonists prior to urgent surgery. Can J Anesth/J Can Anesth 57, 458–467 (2010). https://doi.org/10.1007/s12630-009-9250-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-009-9250-3