Abstract
Purpose
To determine the rate of successful conversion of epidural labour analgesia (ELA) to epidural surgical anesthesia (ESA) for intrapartum Cesarean delivery (CD) with identification of potential risk factors for inadequate ESA. Secondary outcomes include a comparison of the management by subspecialist obstetric anesthesiologists (OB) vs. generalist anesthesiologists (GEN), when inadequate ESA was encountered, with an intention of identifying potential interventional strategies to reduce the need for general anesthesia (GA).
Methods
Health records of all parturients who received ELA and who underwent intrapartum CD during the 3-year period from April 01, 2001 to March 31, 2004 were manually reviewed. Data were analyzed using t test, Chi-square, Fisher’s exact test, and analysis of variance where appropriate. A P < 0.05 was considered significant.
Results
Eight hundred ninety-nine cases were identified. Four were excluded, as two received continuous spinal labour analgesia and two underwent emergency CD with insufficient time for conversion to ESA. Initially, 86.6% (775/895) of the 895 cases were successfully converted to ESA leaving 120 cases of inadequate ESA, 36 of these were managed by OB and 84 by GEN. Ineffective ELA was identified as a risk factor for unsuccessful conversion. Pulling the epidural catheter back 1 cm was identified as an effective intervention that resulted in the successful conversion in >80% of the 120 cases of inadequate ESA. Spinal anesthesia proved effective in 75% of cases. Both interventions reduced the need for GA to 1.2% for OB and 5.6% for GEN.
Conclusions
This investigation provides anesthesiologists with strategies to manage inadequate ESA for intrapartum CD that may reduce the need for GA.
Résumé
Objectif
Déterminer le taux de conversion réussie d’analgésie péridurale pour travail obstétrical (APT) à une anesthésie péridurale chirurgicale (APC) pour un accouchement par césarienne et identifier les facteurs de risque potentiels d’une APT inadaptée. Les résultats secondaires comprennent la comparaison de la prise en charge par des anesthésiologistes surspécialisés en obstétrique (OB) et des anesthésiologistes généralistes (GEN), lors d’APT inadaptée, avec pour objectif d’identifier des stratégies possibles d’intervention pour réduire le recours à une anesthésie générale (AG).
Méthode
Les dossiers médicaux de toutes les parturientes à qui une APT a été administrée et qui ont subi une césarienne au cours d’une période de trois ans allant du 1er avril 2001 au 31 mars 2004 ont été révisés manuellement. Les données ont été analysées à l’aide du test t de Student, du test du khi carré, du test exact de Fisher, et de l’analyse de variance lorsque ce test était approprié. Une valeur P < 0,05 a été considérée significative.
Résultats
Huit cent quatre-vingt-dix-neuf cas ont été identifiés. Quatre ont été exclus, étant donné que deux ont reçu une analgésie du travail par rachianesthésie continue et les deux autres ont subi des césariennes d’urgence, ne laissant pas suffisamment de temps pour une conversion à une APC. Initialement, 86,6 % (775/895) des 895 cas ont montré une conversion réussie à une APC, ce qui laisse 120 cas d’APC inadaptée, dont 36 ont été pris en charge par des OB et 84 par des GEN. Une APT inefficace a été identifiée comme un facteur de risque de conversion manquée. Le fait de retirer le cathéter péridural d’un cm a été identifié comme une intervention efficace résultant en la conversion réussie dans >80 % des 120 cas d’APC inadaptée. La rachianesthésie s’est avérée efficace dans 75 % des cas. Les deux interventions ont réduit le besoin d’AG à 1,2 % avec un OB et 5,6 % avec un GEN.
Conclusion
Cette enquête propose aux anesthésiologistes des stratégies pour la prise en charge d’une APC inadaptée pour une césarienne qui pourraient réduire le besoin d’une AG.
Similar content being viewed by others
The physiologic changes of pregnancy1 place pregnant women at high risk for morbidity and mortality when general anesthesia (GA) rather than regional anesthesia (RA) is administered for Cesarean delivery (CD).2–5 One of the important advantages of epidural labour analgesia (ELA) is the potential for this analgesic modality to be rapidly converted to epidural surgical anesthesia (ESA). This capacity can facilitate CD thereby avoiding the inherent risks of GA. Several small studies6–12 and three larger studies13–15 have suggested a high conversion success rate (89–95%) of ELA to ESA for intrapartum CD. Unfortunately, the identification of significant risk factors for failed conversion of ELA to effective ESA, and the development of management strategies to improve conversion rates have not previously been elucidated. As well, the successful conversion rates and management strategies of experienced subspecialty fellowship-trained obstetric anesthesiologists (OB) compared to generalist anesthesiologists (GEN) for intrapartum CD with an in situ epidural catheter have not previously been reported. The purpose of this investigation was to determine the rate of successful conversion of ELA to ESA for intrapartum CD with identification of potential risk factors for inadequate ESA. Secondary outcomes include a comparison of the management by subspecialist OB vs. GEN, when inadequate ESA was encountered, with an intention of identifying potential strategies to reduce the need for GA.
Methods
Following Human Studies Institutional Review Board approval, the health records of all women at the Royal University Hospital who received ELA and who subsequently underwent CD during a three-year period (from April 01, 2001 to March 31, 2004) were identified and reviewed. Demographic data, gestation at time of labour, number of previous pregnancies and previous deliveries, intrapartum anesthetic epidural management, indication for the CD, and time from epidural placement to CD were recorded. If an attempt to convert ELA to ESA was undertaken but failed to facilitate adequate surgical anesthesia or if conversion from ELA to ESA was not attempted, the subsequent anesthetic management was recorded. Inadequate ESA was defined as (i) an unsuccessful conversion of ELA to ESA utilizing surgical anesthetic concentrations of local anesthetics or (ii) no attempted conversion to ESA for CD. Whether the consultant anesthesiologist at the time of the CD was either OB or GEN was also recorded. Data were analyzed using t test, Chi-square, Fisher’s exact test, and analysis of variance where appropriate. A P < 0.05 was considered significant.
Results
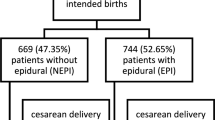
A total of 899 health records of women who had ELA followed by a CD during the 3-year period from April 01, 2001 to March 31, 2004 were identified and manually reviewed. During this time, the anesthetic management was provided by two OB and 37 GEN. Of these 899 cases, two women (0.2%) (1 OB; 1 GEN) who were receiving continuous spinal labour analgesia, administered through an epidural catheter intentionally placed intrathecally, were excluded following an accidental, inadvertent dural puncture during attempted ELA placement. Also, two (0.2%) additional cases (2 GEN) that required emergency CD (one prolapsed umbilical cord; one emergent intervention for second twin), with documentation suggesting that there was insufficient time to convert ELA to ESA, were consequently excluded from further analysis. Therefore, 895 health records were included: 293 (April 01, 2001 to March 31, 2002), 303 (April 01, 2002 to March 31, 2003), and 299 (April 01, 2003 to March 31, 2004). The demographic data were similar for all three years (Table 1).
All women had ELA initiated and maintained with 0.08% ropivacaine + 2 μg ml−1 fentanyl16 utilizing patient-controlled epidural analgesia (PCEA), with or without continuous infusion epidural analgesia (CIEA), which is consistent with routine clinical practice at our institution. None of the women received single-shot intrathecal or combined spinal epidural (CSE) labour analgesia, again consistent with routine clinical practice at our institution.
Of the 895 women included, 86.6% (775/895) of the ELA were successfully converted to effective ESA for CD. The successful conversion to effective ESA was accomplished in 98.6% (764/775) of cases by administering pre-packaged carbonated 2% lidocaine (Astra-Zeneca Canada Inc., Mississauga, ON, Canada), and in 83.6% (640/764) of cases by administering 100 μg of epidural fentanyl (Abbott Laboratories Limited, Toronto, ON, Canada). All (100%) conversions undertaken by OB included the administration of 100 μg of epidural fentanyl. In addition to the carbonated 2% lidocaine, 23 women (21 GEN vs. 2 OB) received other local anesthetics to facilitate effective ESA: 3% 2-chloroprocaine (Astra-Zeneca Canada Inc., Mississauga, ON, Canada) with 7/8 also receiving 100 μg epidural fentanyl (6 GEN; 2 OB) (n = 8); 0.5% ropivacaine (Astra-Zeneca Canada Inc., Mississauga, Ontario) with 8/9 also receiving 100 μg epidural fentanyl (9 GEN) (n = 9); and 0.5% bupivacaine (Astra-Zeneca Canada Inc., Mississauga, ON, Canada) with 5/6 also receiving 100 μg epidural fentanyl (6 GEN) (n = 6). Of the 11 women (GEN) not receiving carbonated 2% lidocaine, the local anesthetics utilized to achieve effective ESA are outlined in Table 2.
Inadequate ESA was initially identified in 120 (13.4%) of the 895 CD. There were no clinically important differences in the demographic profiles between effective ESA compared to inadequate ESA (Table 3). The time from the placement of ELA to CD was not significantly different between effective and inadequate ESA (t test; P = 0.75). Of these 120 women, 50% (60/120) underwent an unsuccessful attempt to convert ELA to ESA. No attempted conversion was recorded for the remaining 50%. In all 60 (100%) attempted conversions that resulted in inadequate ESA, carbonated 2% lidocaine was administered, and in 85% (51/60) 100 μg epidural fentanyl was also administered. All of these attempted but unsuccessful conversions undertaken by OB included the administration of 100 μg of epidural fentanyl. In addition to the carbonated 2% lidocaine, five women (GEN) received other local anesthetics: 3% 2-chloroprocaine with 2/3 also receiving 100 μg epidural fentanyl (n = 3); 0.5% ropivacaine and no epidural fentanyl (n = 1); and 0.5% bupivacaine plus 0.5% ropivacaine and no epidural fentanyl (n = 1). Of the remaining 60 women who did not experience an attempted conversion, 98.3% (59/60) received spinal anesthesia [subarachnoid block (SAB)].
There were no clinically important differences in the demographics of conversion by either OB or GEN (Table 4). Overall, anesthesia for CD was managed by OB in 27.5% (246/895) of the cases and by GEN in 72.5% (649/895) of the cases. There was also no significant difference in the successful conversion of ELA to ESA with 85.4% (210/246) OB and 87.1% (565/649) GEN (Chi-square; P = 0.51).
The mean number of unscheduled anesthesiologist-administered “top ups” per parturient was not significantly different between the two groups with 0.58 (142/246) OB and 0.56 (366/649) GEN per parturient (t test; P = 0.33). The mean number of unscheduled anesthesiologist-administered “top ups” per parturient was significantly higher with inadequate ESA (0.98 ± 1.2) compared to effective ESA (0.50 ± 0.96) (t test; P < 0.0001). Of the successful conversions, 70.3% (545/775) required no unscheduled anesthesiologist-administered “top ups” compared to significantly fewer, 50% (60/120), in the inadequate ESA group (Chi-square; P = 0.009).
Management of the inadequate ESA by both OB and GEN is described in Table 5. The obstetric anesthesiologists pulled the catheter back (1 cm) and administered additional epidural anesthesia significantly more frequently than GEN (58.3% vs. 5.9%, respectively) (Chi-square; P < 0.0001). This intervention resulted in similar, highly successful conversion rates in both groups 85.7% (18/21) OB and 80% (4/5) GEN, respectively. Subarachnoid block resulted in similar rates of successful anesthesia in 77.8% (14/18) OB and 84.9% (45/53) GEN, with no high or total (cardiac arrests) spinals reported. Of the 12 failed SAB, 75% of the women in both groups, OB (3/4) and GEN (6/8), had no epidural local anesthetics administered prior to SAB. Of the failed SAB, 91.7% (11/12) underwent subsequent GA, with the remaining one (OB) having effective ESA following the replacement of the epidural catheter.
The GA rate for intrapartum CD with ELA in situ over the entire 3-year period was 4.4% (39/895). Significantly more GEN chose not to attempt SAB prior to inducing GA, in 75% (27/36) compared to 0% (0/3) by OB (Fisher’s exact test; P = 0.0059). A description of intubating conditions was documented in 37 of the 39 (94.9%) cases, with a difficult intubation (two or three attempts) documented in 10.8% (4/37) cases (Table 6). No failed intubations were reported. The incidence of GA for OB was 1.2% (3/246), significantly less compared to 5.6% (36/649) for GEN (Fisher’s exact test; P = 0.0057).
Discussion
The conversion of ELA to ESA for intrapartum CD was first reported by Milne and Lawson17 in 1973. They reported that 93.3% (112/120) of parturients underwent successful ESA using 2% lidocaine with 1:200,000 epinephrine for CD. This information was noteworthy as the Obstetric Anesthesia authorities of the time reported that the majority of parturients preferred GA for CD.18–20 At that time, this novel management strategy was particularly important considering that maternal mortality directly related to anesthesia was reported to be 36/100,000 CD. The vast majority were related to the complications of GA.2 In a follow-up review in 1979, Milne et al.15 described the anesthetic management of 722 consecutive cases of an intrapartum CD and reported an overall 69% (533/772) success rate of conversion of ELA to ESA. At that time, unfortunately, 23.2% (168/772) of the women with ELA underwent GA with no attempt to utilize the in situ epidural catheter. Importantly, 96.2% (533/554) of the 554 attempted conversions reportedly resulted in effective ESA.
Over the three decades following the initial report by Milne et al.,17 several studies6–15 described retrospective reviews of the anesthesia for intrapartum CD in parturients receiving ELA. Unfortunately, when the attempted conversion resulted in inadequate ESA, none of these studies focused on the anesthetic management in an attempt to identify interventions to potentially reduce the need for GA. This may have been due to either the small sample size or to different identified outcomes. In an attempt to do so and, in part, as a quality review of our own institutional practice patterns, we embarked on this large chart review.
Of the 895 epidurals utilized for ELA, initially 86.6% (775/895) were successfully converted to ESA for CD. This is important considering the potentially devastating consequences of urgent induction of GA, including a difficult or failed intubation combined with a significantly reduced maternal oxygen reserve and a high risk of regurgitation and aspiration.1–5 Such complications may lead to significant maternal morbidity or mortality specifically due to hypoxemia resulting from unsuccessful airway manipulation. The overall successful conversion rate observed in this study (87%) is consistent with other reviews and provides further support for attempting a conversion from ELA to ESA rather than simply abandoning the option of ESA in favour of proceeding directly to GA.
The attempted conversion of ELA to ESA was identified as inadequate in 13.4% of the cases (120/895). We considered the possibility that the failure to convert ELA to ESA may have been the result of an increase in time between epidural catheter placement and utilization for surgery. However, there was no significant difference in the time between ELA placement and effective (496 ± 264 min) or inadequate (504 ± 244 min) ESA (t test; P = 0.75). There was, however, a significantly greater number of unscheduled anesthesiologist-administered “top ups” per parturient during labour (0.98 ± 1.2 vs. 0.56 ± 0.96) with epidural catheters eventually identified to produce inadequate ESA (t test; P < 0.0001). This implies that inadequate ELA is certainly associated with inadequate ESA. Two previous investigations,7,21 each identifying 20 cases of inadequate ESA for intrapartum CD, observed, nonetheless, a significantly higher number of unscheduled anesthesiologists-administered “top ups” with ELA that eventually produced inadequate ESA. Combined with the results of these two smaller studies,7,21 the current investigation further supports the contention that ineffective ELA is much more likely to produce inadequate ESA when conversion is attempted. Consequently, if the chances of inadequate ESA and the potential need for GA are to be reduced, the importance of appropriate ELA management22 to ensure effective ELA can not be overemphasized.
This is the first investigation to compare the anesthetic management of inadequate ESA by OB and GEN (Table 3). Of the 36 inadequate ESA managed by OB, the initial intervention involved pulling the epidural catheter back (~1 cm) followed by the administration of additional surgical anesthetic concentrations of local anesthesia in 56% of the cases. This non-invasive intervention resulted in a successful conversion of previously inadequate ESA in 85% of the cases, thereby avoiding an additional invasive regional anesthetic technique (epidural catheter replacement or SAB) or GA. This simple intervention increased the overall success rate of conversion to effective ESA to 92.3% when managed by OB. Interestingly, significantly fewer (5.9%) cases managed by GEN underwent this intervention. However, 80% (4/5) of those who did were successfully converted to effective ESA. This analysis did not delineate whether the indication to undertake the catheter manipulation was due to the determination of a low level, unilateral, or patchy anesthetic block. Ultimately, this observation is clinically important. It suggests that pulling the catheter back (~1 cm) is an effective means to provide ESA in over 80% of women when an inadequate ESA is encountered, and it also signifies that this intervention has the potential to further increase the overall successful conversion rate to >90%. The success rate of this simple intervention is much higher than the 56% success rate previously reported.23 The retrospective review undertaken by Eappen et al.23 identified 153 cases of ELA in which the catheter was pulled back 0.5 to 1.0 cm in an attempt to improve ELA. Perhaps the higher success rate reported in our review was the result of the routine practice in our institution of pulling the catheter back a minimum of 1.0 cm. Unfortunately, Eappen et al.23 did not report the number of the cases in which the catheter was pulled back only 0.5 cm; therefore, a comparison of the efficacy of the intervention of pulling the catheter back 0.5 cm vs. 1.0 cm cannot be made.
Regarding the remaining inadequate ESA, both groups performed SAB in a comparable number of women with 50.0% OB and 63.1% GEN. Effective surgical anesthesia was reported in 77.8% and 84.9% of the cases, respectively. This observation is clinically significant as it indicates that SAB is a viable option when faced with inadequate ESA. However, an anesthesiologist must be aware that this success rate, although high, is much lower than that observed with SAB with elective CD, i.e., >97%.13 Consequently, these observations do not support the “routine” practice of removing all epidural catheters when presented with inadequate ESA and proceeding immediately to a single shot SAB. Considering the observed SAB failure rate of 15–22% that has not previously been reported, the present investigation suggests that pulling the epidural catheter back should be considered prior to undertaking SAB.
Also, following the failure of one of the four unsuccessful SAB (OB), the epidural catheter was actually replaced resulting in an effective ESA. This important observation does provide anesthesiologists with an alternative management strategy to GA following a failed SAB, should the fetal heart rate tracing be reassuring.
The Royal College of Anaesthetists (RCA) is the only major governing body to issue a “proposed standard or target for best practice” of <3% for the conversion of ELA to GA for intrapartum CD.24 Over the 3-year review period, our overall GA rate of 4.4% (39/895) was higher than the RCA’s <3% recommendation, although the GA for OB was 1.2% (3/246) significantly lower compared to 5.5% (36/649) for GEN (Fisher’s exact test; P = 0.0057). These results provided excellent opportunities for information transfer between OB and GEN with a focus on identifying patient-centred quality improvement management strategies to potentially reduce the need for GA.
A review of the 39 GAs revealed documentation regarding the degree of difficulty encountered during intubation in 95% (37/39) of the cases. Intubation was documented as “easy” in 87% (32/37) of the cases, i.e., requiring only one attempt. However, of the 14% (5/37) of intubations described as “difficult”, two or more direct laryngoscopy attempts were required to successfully intubate. This further highlights the importance of identifying management strategies to avoid the need for GA in the parturient population. Fortunately, no significant morbidity or mortality from difficulty with intubation was reported, and complete failure to intubate was not reported.
Finally, the observations in this study have permitted the development of a clinical pathway (Fig. 1) that will assist anesthesiologists with effective management strategies to deal with inadequate ESA for an intrapartum CD, and will facilitate their attempt to achieve the RCA’s recommendation of <3% GA.24
In conclusion, as anesthesiologists strive to provide best practice guidelines and to further improve care for parturients undergoing intrapartum CD, the beneficial impact of facilitating the conversion of ELA to ESA to avoid GA has come to the fore. For anesthesiologists, inadequate ESA following an attempted conversion presents several management dilemmas which place parturients at risk. As an initial step, this study highlights the importance of maintaining effective ELA, not solely for the purpose of providing analgesia, but, more importantly, to increase the success rate of conversion to ESA should an intrapartum CD become necessary. This investigation provides anesthesiologists with strategies to manage inadequate ESA for intrapartum CD when it is encountered, in order to reduce or obviate the significant maternal morbidity and mortality associated with GA.
References
Campbell DC. Physiologic changes of pregnancy. In: Katz RL, editor. “Obstetric Anesthesia Update” Seminars in Anesthesia, Perioperative Medicine and Pain. 2000; 76: 149–56.
Lewis G. The Confidential Enquiry into Maternal and Child Health (CEMACH). Saving Mothers’ Lives: reviewing maternal deaths to make motherhood safer—2003–2005. The Seventh Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. London: CEMACH. http://www.cemach.org.uk/getattachment/927cf18a-735a-47a0-9200-cdea103781c7/Saving-Mothers-Lives-2003-2005_full.aspx. Accessed October 2008.
Mhyre JM, Riesner MN, Polley LS, Naughton NN. A series of anesthesia-related maternal deaths in Michigan, 1985–2003. Anesthesiology 2007; 106: 1096–104.
Hawkins JL. Anesthesia-related maternal mortality. Clin Obstet Gynecol 2003; 46: 679–87.
Hawkins JL, Koonin LM, Palmer SK, Gibbs CP. Anesthesia-related deaths during obstetric delivery in the United States, 1979–1990. Anesthesiology 1997; 86: 277–84.
Tortosa JC, Parry NS, Mercier FJ, Maziot JX, Benhamou D. Efficacy of augmentation of epidural analgesia for caesarean section. Br J Anaesth 2003; 91: 532–5.
Riley ET, Papasin J. Epidural catheter function during labor predicts anesthetic efficacy for subsequent cesarean delivery. Int J Obstet Anesth 2002; 11: 81–4.
Norris MC. Are combined spinal-epidural catheters reliable? Int J Obstet Anesth 2000; 9: 3–6.
Furst SR, Reisner LS. Risk of high spinal anesthesia following failed epidural block for cesarean delivery. J Clin Anesth 1995; 7: 71–4.
Dickson MA, Jenkins J. Extension of epidural blockade for emergency caesarean section. Assessment of a bolus dose of bupivacaine 0.5% 10 ml following an infusion of 0.1% for analgesia in labour. Anaesthesia 1994; 94: 636–8.
Price ML, Reynolds F, Morgan BM. Extending epidural blockade for emergency caesarean section: evaluation of 2% lignocaine with adrenaline. Int J Obstet Anesth 1991; 1: 13–8.
Morgan BM, Magni V, Goroszenuik T. Anaesthesia for emergency caesarean section. Br J Obstet Gynaecol 1990; 97: 420–4.
Pan PH, Bogard TD, Owen MD. Incidence and characteristics of failures in obstetric neuraxial analgesia and anesthesia: a retrospective analysis of 19,259 deliveries. Int J Obstet Anesth 2004; 13: 227–33.
Garry M, Davies S. Failure of regional blockade for caesarean section. Int J Obstet Anesth 2002; 11: 9–12.
Milne MK, Dalrymple DG, Allison R, Lawson JI. The extension of labour epidural analgesia for caesarean section. Anaesthesia 1979; 34: 992–5.
Campbell DC, Zwack RM, Crone LA, Yip RW. Ambulatory labor epidural analgesia: bupivacaine versus ropivacaine. Anesth Analg 2000; 90: 1384–9.
Milne MK, Lawson JI. Epidural analgesia for caesarean section. A review of 182 cases. Br J Anaesth 1973; 45: 1206–10.
Crawford JS. Principles and Practice of Obstetric Anaesthesia. 3rd ed. London: Blackwell; 1972. p. 188.
Doughty A. Anaesthesia for operative obstetrics and gynaecology. In: Wylie WD, Churchill-Davidson HC, editors. A Practice of Anaesthesia. 3rd ed. London: Lloyd-Luke; 1972. p. 1459.
Moir DD. Recent advances in pain relief in childbirth. II. Regional anaesthesia. Br J Anaesth 1971; 43: 849–63.
Orbach-Zinger S, Friedman L, Avramovich A, et al. Risk factors for failure to extend labor epidural analgesia to epidural anesthesia for cesarean section. Acta Anaesthesiol Scand 2006; 50: 793–7.
Campbell DC. Low-dose epidural labor analgesia. Tech Reg Anesth Pain Manag 2001; 5: 3–8.
Eappen S, Blinn A, Segal S. Incidence of epidural catheter replacement in parturients: a retrospective chart review. Int J Obstet Anesth 1998; 7: 220–5.
Russell IF. Technique of anaesthesia for caesarean section. In: Kinsella M, editor. Raising the Standard: A Compendium of Audit Recipes. Section 8.8: Obstetric Services. 2nd ed. London: The Royal College of Anaesthetists; 2006. http://www.rcoa.ac.uk/index.asp?PageID=125. Accessed October 2008.
Acknowledgements
Financial support: 1. Dean’s Medical Student Summer Project, sponsored by the College of Medicine, University of Saskatchewan (Tony Tran). 2. Dr. Campbell received funded research time from the Department of Anesthesiology, Perioperative Medicine and Pain Management, College of Medicine, University of Saskatchewan. 3. Chart review was supported by Health Records Department of Saskatoon Health Region.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Campbell, D.C., Tran, T. Conversion of epidural labour analgesia to epidural anesthesia for intrapartum Cesarean delivery. Can J Anesth/J Can Anesth 56, 19–26 (2009). https://doi.org/10.1007/s12630-008-9004-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-008-9004-7