Abstract
Objective
To find out etiology and clinical course of thrombocytosis in Indian pediatric population.
Methods
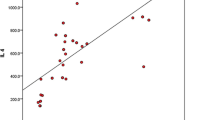
A total of 250 patients having thrombocytosis (defined as platelet count >500 × 109/L) on haematological investigations were studied over one yr period. All patients were evaluated clinically and were subjected to investigations, including complete blood counts (CBC) with peripheral smear examination. To elucidate the possible role of inflammatory cytokines in pathogenesis of RT, levels of Interleukin-6 (IL-6) and C — reactive protein (CRP) were estimated.
Results
Infants and young children (<2 yr age) were most common group, contributing 60% of total cases. Out of total 250 cases, only 3 (1.2%) cases were found to have primary thrombocytosis and remaining 98.8% cases were having RT. Among RT patients, infections (alone or in association with iron deficiency anemia) were most common cause, accounting for 65% cases, while iron deficiency anemia (IDA) was second most common cause accounting for 41.3% cases (12.6% IDA alone and 28.7 % in association with infections). Other causes included nutritional dimorphic anemia and patients on treatment for megaloblastic anemia, acute lymphoblastic leukemia (during treatment) and lymphoma. Among various groups of RT, IL-6 and CRP levels were higher in patients with infection with or without IDA than IDA alone. One child with essential thrombocytosis and one child with RT had thrombotic complications. On follow up, platelet counts normalized in most of the patients with treatment of underlying conditions.
Conclusions
Results of this study suggest that essential thrombocytosis is extremely rare in children. Infections and IDA (alone or in association with infections) are common causes of RT. IL-6 and CRP levels are increased in patients with RT, to a higher level in patients with infections than in patients with IDA. Most patients with RT have uneventful recovery of platelet counts to normal range with treatment for underlying condition.
Similar content being viewed by others
References
Dame C, Sutor AH. Primary and secondary thrombocytosis in childhood. Br J Haematol 2005; 129: 165–177.
Schafer AI. Thrombocytosis. New Engl J Med 2004; 350: 1211–1219.
Maguire JL, deVeber G, Parkin PC. Association between iron-deficiency anemia and stroke in young children. Pediatrics 2007; 120: 1053–1057.
Akins PT, Glenn S, Nemeth PM, Derdeyn CP. Carotid artery thrombus associated with severe iron-deficiency anemia and thrombocytosis. Stroke 1996; 27: 1002–1005.
Belman AL, Roque CT, Ancona R, Anand AK, Davis RP. Cerebral venous thrombosis in a child with iron deficiency anemia and thrombocytosis. Stroke 1990; 21: 488–493.
Sebire G, Tabarki B, Saunders DE, Leroy I, Leisner R, Martin SC, Husson B et al. Cerebral venous sinus thrombosis in children: risk factors, presentation, diagnosis and outcome. Brain 2005; 128: 477–489.
Hollen CW, Henthorn J, Koziol JA, Burstein SA. Elevated serum interleukin-6 levels in patients with reactive thrombocytosis. Br J Haematol 1991; 79: 286–290.
Tefferi A, Ho TC, Ahmann GJ, Katzmann JA, Greipp PR. Plasma interleukin-6 and C-reactive protein levels in reactive versus clonal thrombocytosis. Am J Med 1994; 94: 374–378.
Matsubara K, Fukaya T, Nigami H, Harigaya H, Hirata T, Nozaki H, baba K. Age-dependent changes in the incidence and etiology of childhood thrombocytosis. Acta Haematol 2004; 111: 132–137.
Chan KW, Kaikov Y, Wadsworth LD. Thrombocytosis in childhood: A survey of 94 patients. Pediatrics 1989; 84: 1064–1067.
Vora AJ, Lilleyman JS. Secondary thrombocytosis. Arch Dis Child 1993; 68: 88–90.
Yohannan MD, Higgy KE, Al-Mashhadani SA, Santhosh-Kumar CR. Thrombocytosis: Etiologic analysis of 663 patients. Clinic Pediatr 1994; 33: 340–343.
Gomber S, Kumar S, Rusia U, Gupta P, Agarwal KN, Sharma S. Prevalence and etiology of nutritional anemias in early childhood in an urban slum. Indian J Med Res 1998; 107: 269–273.
Lipschitz DA, Cook JD, Finch CA. A Clinical evaluation of serum ferritin as an index of iron stores. New Engl J Med 1974; 290: 1213.
National Family Health Survey-3, 2005–2006. International Institute of Population Sciences, Mumbai 2005.
Bilic E. Amino acid sequence homology of thrombopoietin and erythropoietin may explain thrombocytosis in children with iron deficiency anemia. J Pediatr Hematol Oncol 2003; 25: 675–676.
Chandra J, Jain V, Narayan S et al. Tremors and thrombocytosis during treatment of megaloblastic anemia. Annals Trop Pediatr 2006; 26: 101–105.
Randi ML, Rossi C, Barbonr E, Pietrogrande F, Girolami A. Incidence of thrombocytosis in lymphomas. Leuk Lymphoma 1992; 7: 139–141.
Ishiguro A, Suzuki Y, Mito M et al. Elevation of serum thrombopoietin precedes thrombocytosis in acute infections. Br J Haematol 2002; 116: 612–618.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yadav, D., Chandra, J., Sharma, S. et al. Clinicohematological study of thrombocytosis. Indian J Pediatr 77, 643–647 (2010). https://doi.org/10.1007/s12098-010-0091-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-010-0091-4