Abstract
Objective
Predicting extubation failure (EF) is one of the most challenging aspects of critical care medicine. The literature on EF in neurocritical care patients is very scarce. We sought to determine the ability of traditional weaning parameters to predict EF in neurocritical patients.
Methods
This is a retrospective observational study performed at a tertiary level, academic, Neurological Intensive Care Unit (NCCU). We included all adult patients intubated for neurological reasons in whom an attempt to perform extubation was performed. We compared traditional weaning parameters between patients who failed extubation and those successfully extubated. Fishers exact test was used for categorical variables and t-test for continuous variables. Weaning parameters were analyzed as categorical variables and when appropriate as continuous. We incorporated a coma scale (Four Score) in an attempt to determine if neurologic dysfunction could account for EF.
Results
The study sample compromised 62 patients undergoing extubation trial. None of the individual weaning parameters predicted EF: rapid shallow breathing index (P = 0.62), minute ventilation (P = 0.7479), respiratory rate (P = 1.0), negative inspiratory force (P = 0.62), tidal volume, and PaO2/FIO2 ratio (P = 1.0). There was no significant difference in Four Scale score between EF and successfully extubated patients (0.44, proportions of the mean, t-test). There was no combination of weaning parameters that allowed prediction of EF. All patients had at least three normal weaning parameters, but there was no combination of parameters that accurately predicted EF. Overall, weaning parameters had better specificity than sensitivity for predicting EF.
Conclusions
In this sample of neurocritical care patients undergoing extubation trial, traditional weaning parameters do not predict extubation failure.
Similar content being viewed by others
Introduction
It is estimated that between 5 and 20% of patients undergoing extubation will experience extubation failure (EF) [1]. Premature discontinuation of mechanical ventilation is associated with increased morbidity and mortality [1]. Extubation failure is associated with increased mortality, increased cost, prolonged stay, greater need for tracheostomy, and prolonged intensive care unit (ICU) care. Multiple clinical studies have analyzed the factors involved in EF and have attempted to refine the clinical elements and laboratory findings that can be used to assess the readiness for extubation [2, 3]. Unfortunately, most EF studies have focused mainly on medical ICU patients or general surgery ICU patients. The data on patients with neurosurgical or neurological pathology undergoing extubation trials are very limited.
Extubating neurocritical patients presents some very unique challenges [4]. Performing a detailed brainstem examination in the intubated (often uncooperative) patient is very difficult and it is only once the patient has failed extubation that it becomes evident that the patient is unable to protect his airway. Neurocritical patients often require copious amounts of intravenous fluids to enhance cerebral perfusion, a factor well known to hinder successful extubation. Neuromuscular weakness and diminished level of consciousness are known to be associated with EF, but the degree of weakness and the level of alertness required for successful extubation are not clear. In addition, it is possible that patients with brain injury may have unique respiratory mechanics that make weaning and extubation even more challenging [5]. In this study, we sought to determine if traditional weaning parameters (TWPs) successfully predicted EF in a consecutive series of patients undergoing extubation trial in a neurocritical care unit (NCCU).
Materials and Methods
This is a retrospective case series study performed in an NCCU at a tertiary care university hospital. All patients undergoing intubation and mechanical ventilation due to cranial pathology were identified using a prospectively collected database and/or the NCCU log book. Patients undergoing intubation due to spinal cord pathology were excluded. The following information was obtained from the above-mentioned database and/or the medical records: basic demographics, admission diagnosis, severity of illness (as determined by the Glasgow Coma Scale), past medical history, intubation date, duration of intubation, and the presence of failed extubation (need for reintubation within 48 h). In addition, we determined the presence of in-hospital comorbidities that could interfere with extubation. The following comorbidities were recorded: pneumonia, sepsis, hydrocephalus requiring ventriculostomy, seizures, vasospasm, venous thromboembolism, acute lung injury/acute respiratory distress syndrome, and barotrauma. The presence or absence of a spontaneous breathing trial on the extubation day and during prior days was recorded. A new coma scale (the Four Scale) was used to determine if differences in the level of consciousness could explain EFs [6]. The Four Scale was selected, as it evaluates brainstem function (integral for successful extubation) more accurately than other coma scales. The Four Scale was obtained from the nursing notes and the physicians’ progress notes when not calculated directly.
Weaning parameters (recorded daily by the respiratory therapist) were obtained from the ventilator log sheet. Weaning parameters are obtained when readiness for liberation from mechanical ventilation is established as determined by the fact that the patient is on pressure support ventilation, the intracranial pressure is controlled, the patient is alert, and endotracheal secretions are minimal. The following weaning parameters are recorded daily by the respiratory therapist at our institution when there are no contraindications to doing so: respiratory rate (RR), minute ventilation (MV), rapid shallow breathing index (RSBI), tidal volume (Vt), and negative inspiratory force (NIF). The PaO2/FIO2 ratio was calculated by obtaining the PaO2 from the latest arterial blood gas obtained prior to extubation and the FIO2 used at that time, either during a spontaneous breathing trial (SBT), or during CPAP if an SBT was not done. For the purpose of this study, we used only the weaning parameters obtained on the day the extubation attempt was performed.
We compared demographics, past medical history, admission diagnosis, and hospital complications between patients who failed extubation and those who were successfully extubated to determine if there were any baseline differences between the two groups. We compared TWPs between patients who failed extubation and those who were successfully extubated. The following values were used as cutoff for normal: RR < 30, MV ≤ 10 l/min, RSBI < 105, Vt ≥ 5 ml/kg, NIF > −20 cm H2O, and PaO2/FIO2 ratio ≥ 300. Fishers exact test was used to compare all categorical variables. A proportion of the means test (t-test) was used to compare all continuous variables. We analyzed both individual weaning parameters as well as different combinations of weaning parameters to determine which one(s) most accurately predicted EF. We analyzed all variables except Vt as both categorical and continuous values to determine if any specific values different from the traditional cutoff values where associated with a greater likelihood of failing extubation. In addition, we sought to determine if the number of normal weaning parameters (as opposed to a single normal weaning parameter) had any influence on the success of attempted extubation.
Results
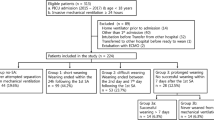
During an 8 month period of examination, 123 patients required intubation and mechanical ventilation in our unit. We excluded 61 patients because of the following reasons: intubation for medical reasons (9), intubation due to spine injuries (13), intubation only for performance of a procedure (15), tracheostomy performed without extubation trial (4), care withdrawn or brain dead (11), and missing data (9). The final sample comprised 62 patients of which 11 (17.5%) failed extubation and 51 (82.5%) were successfully extubated. The median age was 52 years (range 17–87) and 28/62 of the patients were women. The cohort was composed of 31 Caucasians, 28 African Americans, and 3 patients belonging to other ethnic groups. The clinical diagnosis included intracranial hemorrhage (20), subarachnoid hemorrhage (16), traumatic brain injury (11), brain tumor (7), subdural hematoma (5), ischemic stroke (2), and other (1).
There was no difference in the baseline demographics, in-hospital complications, or Four Scale score between patients who failed extubation and those who were successfully extubated (Table 1). We did not find a Four Scale score that discriminated patients who failed extubation from those who were successfully extubated. In patients, who failed extubation, 3/11 (27%) had Four Scores of <12, in the group that was successfully extubated, 11/51 (22%) had Four Scores below 12 (P = 0.6997. Fishers exact test). There were no patients with normal Four Scales as it was always performed prior to extubation (typically during T-piece trial). There was no significant difference in the mean Four Scale between patients who failed extubation and those who were successfully extubated (12.4 vs. 12.1, P = 0.44, t-test). When the individual weaning parameters were analyzed as normal or abnormal based on the previously specified cutoffs, we did not find any significant difference between patients who had EF and those who did not (Table 2). When the weaning parameters were analyzed as continuous variables (t-test) we also did not find any difference in the weaning parameters between EFs and successful extubations (Table 3). The number of normal weaning parameters (three or more as all patients had at least three normal weaning parameters) did not predict successful extubation (Table 4). Thus, even the 11 patients who failed extubation had at least three normal weaning parameters.
A spontaneous breathing trial was performed in 50/62 (81%) patients studied. There was no significant difference between patients undergoing a spontaneous breathing trial and not undergoing it in terms of extubation failure (P = 0.6708. Fishers exact test). Since a spontaneous breathing trial is not a conventional weaning parameter we did not include it in all our tables.
The sensitivity, specificity, positive predictive value, and negative predictive value of the different weaning parameters are listed in Table 5. Although some of the weaning parameters achieved relatively high specificity (RSBI, PaO2/FIO2, NIF) none of the weaning parameters achieved enough sensitivity and specificity to be reliably used as a sole predictor of extubation failure. Performance of a spontaneous breathing trial achieved the highest sensitivity (90%) but had low specificity (20%).
Discussion
The ability to predict extubation failure is paramount, as it has been demonstrated that both premature extubation and prolonged intubation lead to increased morbidity and mortality, hospitals costs, and length of stay [1–5]. The hope of accurately predicting EF has led to a large volume of literature, and weaning parameters that are both highly sensitive and specific remain a holy grail for ICU physicians. In our retrospective study, we found that traditional weaning parameters poorly predict EF in the neurocritical care population. This was found to be true for individual weaning parameters as well as for combination of weaning parameters.
Given our neurocritical care patient population, the failure of conventional weaning parameters is not surprising, as patients are often intubated for airway protection rather than lung pathology. As weaning parameters are primarily a measure of the pulmonary system, it can be expected that their sensitivity for assessing patients with primary neurological dysfunction would be poor. In addition, recent studies suggest that patients with acute brain injury may have abnormal respiratory mechanics secondary to the brain injury, a finding that can easily be overlooked in patients with seemingly normal lungs [5].
It may be that conventional weaning parameters fail in other ICU populations as well [2]. Frequency to tidal volume ratio (f/Vt), commonly considered as the most accurate weaning parameter, was recently investigated by Tanios et al. [2]. It was found that including this ratio in a weaning protocol prolonged weaning time. In their study, patients were divided into two groups. The first group incorporated f/Vt into a weaning protocol, specifically, an f/Vt greater than 105 breaths/min/l, precluded a spontaneous breathing trial. The second group did not have an f/Vt incorporated into their weaning protocol, and were given spontaneous breathing trials based on clinical acumen. It was found that the group that relied upon f/Vt had a longer duration of intubation. It is a disturbing notion that even in a general ICU population; f/Vt was poor in predicting EF.
Another factor that may have contributed to extubation failure in our population is the amount of fluids that our patients received. Neurocritical care patients tend to receive generous amounts of intravenous fluids mainly in an attempt to improve cerebral perfusion. This fact, coupled with the knowledge that a positive fluid balance 24 h prior to extubation is a predictor of EF certainly may have played a role [7].
Others have noted the difficulty in applying TWP’s in the neurologic population (8). Previous research by Vallverdu and colleagues found that it was more difficult to predict EF in patients who were intubated for neurological reasons when compared to those intubated for acute respiratory failure. They suggested that the ability to cough and clear respiratory secretions might be of clinical benefit, which was objectively measured as the maximal expiratory pressure, a parameter that we did not incorporate into our weaning parameters. Conventional weaning parameters in general, measure how well a patient can breathe in a relatively rested state, and do not assess the forced maneuver of clearing the airway. In the strict sense, conventional weaning parameters do not indicate if the patient is able to protect his/her airway, a determination that is mainly based on clinical judgment. Therefore, while TWP’s are imperative in the assessment of respiratory failure with pulmonary etiology, they do little for the patient intubated solely for neurological reasons. Measuring the maximal expiratory pressure does intuitively make sense, as neurological patients often have a decreased ability to clear their airway, and measuring maximal expiratory pressure may provide the clinician a way to objectively determine how well a patient can protect their airway. Nevertheless, the ability to splint the airway and maintain it open is only evident after extubation.
There are multiple factors that can influence EF in the NCCU and many of them are specific to neurocritical care patients. Cranial neuropathy, cerebellar dysfunction, midbrain compression due to hemispheric lesions, basal ganglia involvement, airway edema related to prone positioning during surgery, vocal cord palsy, unrecognized neuromuscular dysfunction, and stress cardiomyopathy are common occurrences in the NCCU. The above-mentioned factors in concert with cardiopulmonary problems such as flail chest, pleural effusions, atelectasis, and pulmonary embolism, make extubating patients in the NCCU very challenging. Early tracheostomy is a frequently used approach in patients deemed at high-risk for extubation failure. Unfortunately, as our data indicates, we do not have adequate predictive factors that help us identify such group of patients. Early tracheostomy does offer significant advantages, as if facilitates liberation from mechanical ventilation. The use of non-invasive mechanical ventilation as a bridge from mechanical ventilation to unassisted breathing remains controversial. In our study, patients did not receive noninvasive ventilation as NCCU patients often have contraindications for this therapy (impaired cough, craniofacial wounds, obtundation).
Being a retrospective study, limitations are inherent. As many reintubations are done in emergency situations, the etiology of respiratory failure was not always recorded. This is a key piece of missing data, as it may provide insight as to why TWP’s were not helpful. Also, the fluid balance for each patient was not recorded. As stated earlier, positive fluid balance 24 h prior to extubation is a predictor for EF (7). Without an accurate record of fluid balance, we cannot say if extubation failure was independent of this factor. In this study, collecting fluid balance was difficult as data transfers from other ICUs, other institutions, and the operating room was not complete.
A recent study by Navalesi et al. [8] concluded that a systematic approach to extubation in the NCCU is superior to sole physician judgement. However, the study is significantly different from ours. In our study, we included patients intubated only for neurologic reasons and excluded patients intubated for cardiopulmonary reasons and for elective procedures. The weaning parameters used in our study were also different, as Navalesi et al. relied mainly on the RSBI and arterial gasimetry to perform extubation. Our study focused on neurosurgical patients, while Navalesi studied neurological and neurosurgical patients. We agree with Navalesi’s findings that a systematic approach is better, but the question that remains unanswered is which systematic approach is the optimal one.
Conclusion
Our findings suggest that TWP’s do not predict extubation failure in a neurological population. It is a retrospective study and further prospective, randomized controlled trials need to be performed. If, as Vallverdu has proposed, EFs are due to the inability to clear the airway, focus should be placed on maximal expiratory pressure and in quantifying the amount of secretions [9]. However, our study supports the argument that the clinician must use parameters outside of TWP’s to decide whether or not a neurological patient will fail extubation.
References
Epstein SK. Predicting extubation failure. Chest. 2001;120:1061–3. doi:10.1378/chest.120.4.1061.
Tanios MA, Nevins ML, Hendra KP, et al. A randomized, controlled trial of the role of weaning predictors in clinical decision making. Crit Care Med. 2006;34:2530–5. doi:10.1097/01.CCM.0000236546.98861.25.
Epstein SK. Extubation failure: an outcome to be avoided. Crit Care. 2004;8:310–2. doi:10.1186/cc2927.
Coplin WM, Pierson DJ, Cooley KD, et al. Implications of extubation delay in brain-injured patients meeting standard weaning criteria. Am J Respir Crit Care Med. 2000;161:1530–6.
Koutsoukou A, Perraki H, Raftopoulou A, et al. Respiratory mechanics in brain-injured patients. Intensive Care Med. 2006;32:1947–54. doi:10.1007/s00134-006-0406-0.
Wijdicks EF, Bamlet WR, Maramattom BV, et al. Validation of a new coma scale: the FOUR score. Ann Neurol. 2005;58(4):585–93. doi:10.1002/ana.20611.
Frutos-Vivar F, Ferguson N, Esteban A, et al. Risk factors for extubation failure in patients following a successful spontaneous breathing trial. Chest. 2006;130:1664–71. doi:10.1378/chest.130.6.1664.
Navalesi P, Frigerio P, Moretti M, et al. Rate of reintubation in mechanically ventilated neurosurgical and neurologic patients: evaluation of a systematic approach to weaning and extubation. Crit Care Med. 2008;36:2986–92. doi:10.1097/CCM.0b013e31818b35f2.
Vallverdu I, Calaf N, Subirana M, et al. Clinical characteristics, respiratory functional parameters, and outcome of a two-hour T-piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med. 1998;158:1855–62.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ko, R., Ramos, L. & Chalela, J.A. Conventional Weaning Parameters do not Predict Extubation Failure in Neurocritical Care Patients. Neurocrit Care 10, 269–273 (2009). https://doi.org/10.1007/s12028-008-9181-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-008-9181-9