Abstract
Background
Radiation exposure to patients and spine surgeons during spine surgery is expected. The risks of radiation exposure include thyroid cancer, cataracts, and lymphoma. Although imaging techniques facilitate less invasive approaches and improve intraoperative accuracy, they may increase radiation exposure.
Questions/purposes
We performed a systematic review to determine whether (1) radiation exposure differs in open spine procedures compared with less invasive spine procedures; (2) radiation exposure differs in where the surgeon is positioned in relation to the C-arm; and (3) if radiation exposure differs using standard C-arm fluoroscopy or fluoroscopy with computer-assisted navigation.
Methods
A PubMed search was performed from January 1980 to July 2013 for English language articles relating to radiation exposure in spine surgery. Twenty-two relevant articles met inclusion criteria. Level of evidence was assigned on clinical studies. Traditional study quality evaluation of nonclinical studies was not applicable.
Results
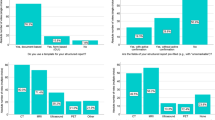
There are important risks of radiation exposure in spine surgery to both the surgeon and patient. There is increased radiation exposure in less invasive spine procedures, but the use of protective barriers decreases radiation exposure. Where the surgeon stands in relation to the image source is important. Increasing the distance between the location of the C-arm radiation source and the surgeon, and standing contralateral from the C-arm radiation source, decreases radiation exposure. The use of advanced imaging modalities such as CT or three-dimensional computer-assisted navigation can potentially decrease radiation exposure.
Conclusions
There is increased radiation exposure during less invasive spine surgery, which affects the surgeon, patient, and operating room personnel. Being cognizant of radiation exposure risks, the spine surgeon can potentially minimize radiation risks by optimizing variables such as the use of barriers, knowledge of position, distance from the radiation source, and use of advanced image guidance navigation-assisted technology to minimize radiation exposure. Continued research is important to study the long-term risk of radiation exposure and its relationship to cancer, which remains a major concern and needs further study as the popularity of less invasive spine surgery increases.


Similar content being viewed by others
References
Abdullah KG, Bishop FS, Lubelski D, Steinmetz MP, Benzel EC, Mroz TE. Radiation exposure to the spine surgeon in lumbar and thoracolumbar fusions with the use of an intraoperative computed tomographic 3-dimensional imaging system. Spine (Phila Pa 1976). 2012;37:E1074–1078.
Bandela JR, Jacob RP, Arreola M, Griglock TM, Bova F, Yang M. Use of CT-based intraoperative spinal navigation: management of radiation exposure to operator, staff, and patients. World Neurosurg. 2013;79:390–394.
Bronsard N, Boli T, Challali M, de Dompsure R, Amoretti N, Padovani B, Bruneton G, Fuchs A, de Peretti F. Comparison between percutaneous and traditional fixation of lumbar spine fracture: intraoperative radiation exposure levels and outcomes. Orthop Traumatol Surg Res. 2013;99:162–168.
Fischetti M. Exposed. Medical imaging delivers big doses of radiation. Sci Am. 2011;304:96.
Fransen P. Fluoroscopic exposure in modern spinal surgery. Acta Orthop Belg. 2011;77:386–389.
Gebhard FT, Kraus MD, Schneider E, Liener UC, Kinzl L, Arand M. Does computer-assisted spine surgery reduce intraoperative radiation doses? Spine (Phila Pa 1976). 2006;31:2024–2027; discussion 2028.
Giordano BD, Baumhauer JF, Morgan TL, Rechtine GR. Cervical spine imaging using standard C-arm fluoroscopy: patient and surgeon exposure to ionizing radiation. Spine (Phila Pa 1976). 2008;33:1970–1976.
Giordano BD, Baumhauer JF, Morgan TL, Rechtine GR 2nd. Cervical spine imaging using mini-C-arm fluoroscopy: patient and surgeon exposure to direct and scatter radiation. J Spinal Disord Tech. 2009;22:399–403.
Giordano BD, Grauer JN, Miller CP, Morgan TL, Rechtine GR 2nd. Radiation exposure issues in orthopaedics. J Bone Joint Surg Am. 2011;93:e69(61–10).
Hayashi A. Radiation exposure in the OR: is it safe? AAOS Now. 2008. Available at: http://www.aaos.org/news/aaosnow/dec08/clinical1.asp. Accessed December 1, 2013.
Jones DP, Robertson PA, Lunt B, Jackson SA. Radiation exposure during fluoroscopically assisted pedicle screw insertion in the lumbar spine. Spine (Phila Pa 1976). 2000;25:1538–1541.
Kim CW, Lee YP, Taylor W, Oygar A, Kim WK. Use of navigation-assisted fluoroscopy to decrease radiation exposure during minimally invasive spine surgery. Spine J. 2008;8:584–590.
Kraus MD, Krischak G, Keppler P, Gebhard FT, Schuetz UH. Can computer-assisted surgery reduce the effective dose for spinal fusion and sacroiliac screw insertion? Clin Orthop Relat Res. 2010;468:2419–2429.
Kruger R, Faciszewski T. Radiation dose reduction to medical staff during vertebroplasty: a review of techniques and methods to mitigate occupational dose. Spine (Phila Pa 1976). 2003;28:1608–1613.
Lange J, Karellas A, Street J, Eck JC, Lapinsky A, Connolly PJ, Dipaola CP. Estimating the effective radiation dose imparted to patients by intraoperative cone-beam computed tomography in thoracolumbar spinal surgery. Spine (Phila Pa 1976). 2013;38:E306–312.
Lee K, Lee KM, Park MS, Lee B, Kwon DG, Chung CY. Measurements of surgeons’ exposure to ionizing radiation dose during intraoperative use of C-arm fluoroscopy. Spine (Phila Pa 1976). 2012;37:1240–1244.
Lester JD, Hsu S, Ahmad CS. Occupational hazards facing orthopedic surgeons. Am J Orthop (Belle Mead NJ). 2012;41:132–139.
Mariscalco MW, Yamashita T, Steinmetz MP, Krishnaney AA, Lieberman IH, Mroz TE. Radiation exposure to the surgeon during open lumbar microdiscectomy and minimally invasive microdiscectomy: a prospective, controlled trial. Spine (Phila Pa 1976). 2011;36:255–260.
Mastrangelo G, Fedeli U, Fadda E, Giovanazzi A, Scoizzato L, Saia B. Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med (Lond). 2005;55:498–500.
McCollough CH, Schueler BA. Calculation of effective dose. Med Phys. 2000;27:828–837.
Mehlman CT, DiPasquale TG. Radiation exposure to the orthopaedic surgical team during fluoroscopy: ‘how far away is far enough?’ J Orthop Trauma. 1997;11:392–398.
Mroz TE, Abdullah KG, Steinmetz MP, Klineberg EO, Lieberman IH. Radiation exposure to the surgeon during percutaneous pedicle screw placement. J Spinal Disord Tech. 2011;24:264–267.
Mroz TE, Yamashita T, Davros WJ, Lieberman IH. Radiation exposure to the surgeon and the patient during kyphoplasty. J Spinal Disord Tech. 2008;21:96–100.
Mulconrey DS. Fluoroscopic radiation exposure in spinal surgery: in vivo evaluation for operating room personnel. J Spinal Disord Tech. 2013 Nov 7 [Epub ahead of print].
Nakashima M, Kondo H, Miura S, Soda M, Hayashi T, Matsuo T, Yamashita S, Sekine I. Incidence of multiple primary cancers in Nagasaki atomic bomb survivors: association with radiation exposure. Cancer Sci. 2008;99:87–92.
Rampersaud YR, Foley KT, Shen AC, Williams S, Solomito M. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976). 2000;25:2637–2645.
Recommendations of the International Commission on Radiological Protection. New York, NY, USA: International Commission on Radiological Protection; 1990;21.
Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37:1–332.
Recommendations on Limits for Exposure to Ionizing Radiation. Bethesda, MD, USA: National Council on Radiation Protection and Measurements; 1987:91.
Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005;13:69–76.
Slomczykowski M, Roberto M, Schneeberger P, Ozdoba C, Vock P. Radiation dose for pedicle screw insertion. Fluoroscopic method versus computer-assisted surgery. Spine (Phila Pa 1976). 1999;24:975–982; discussion 983.
Smith HE, Welsch MD, Sasso RC, Vaccaro AR. Comparison of radiation exposure in lumbar pedicle screw placement with fluoroscopy vs computer-assisted image guidance with intraoperative three-dimensional imaging. J Spinal Cord Med. 2008;31:532–537.
Synowitz M, Kiwit J. Surgeon’s radiation exposure during percutaneous vertebroplasty. J Neurosurg Spine. 2006;4:106–109.
Theocharopoulos N, Damilakis J, Perisinakis K, Papadokostakis G, Hadjipavlou A, Gourtsoyiannis N. Occupational gonadal and embryo/fetal doses from fluoroscopically assisted surgical treatments of spinal disorders. Spine (Phila Pa 1976). 2004;29:2573–2580.
US Nuclear Regulatory Commission Basic References. US Nuclear Regulatory Commission. Available at: http://www.nrc.gov/reading-rm/basic-ref.html. Accessed December 1, 2013.
von Wrangel A, Cederblad A, Rodriguez-Catarino M. Fluoroscopically guided percutaneous vertebroplasty: assessment of radiation doses and implementation of procedural routines to reduce operator exposure. Acta Radiol. 2009;50:490–496.
Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. 2010;19:1780–1784.
Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85:1–3.
Zhang J, Weir V, Fajardo L, Lin J, Hsiung H, Ritenour ER. Dosimetric characterization of a cone-beam O-arm imaging system. J Xray Sci Technol. 2009;17:305–317.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
About this article
Cite this article
Yu, E., Khan, S.N. Does Less Invasive Spine Surgery Result in Increased Radiation Exposure? A Systematic Review. Clin Orthop Relat Res 472, 1738–1748 (2014). https://doi.org/10.1007/s11999-014-3503-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3503-3