Opinion statement
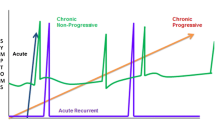
Migraine prophylaxis is a stepwise procedure with lifestyle advice followed by consideration of medications. Patients should be advised to try to maintain a regular lifestyle, with regular sleep, meals, exercise, and management of stress, perhaps through relaxation techniques or other ways that are sensible for them. If this regimen does not adequately control their migraines, preventatives are indicated. Patients can choose between evidence-based nutraceuticals such as riboflavin, feverfew, butterbur, or coenzyme Q10, or more traditional pharmaco-therapeutics. Medicine choices are somewhat limited by what is available in each country, but from the full range, the medicines of first choice are beta-adrenoceptor blockers, flunarizine, topiramate, and valproic acid. Beta-adrenoceptor blockers are particularly useful in patients also suffering from hypertension or tachycardia. Following recent studies, topiramate has become a first choice for episodic as well as chronic migraine. It is the only prophylactic drug that may lead to weight loss, but it is sometimes associated with adverse cognitive effects. Valproic acid and flunarizine also have very good prophylactic properties. However, valproic acid is often associated with adverse effects, and flunarizine is unavailable in many countries, including the United States. If sequential monotherapies are ineffective, combinations of first-line drugs should be tried before advancing to drugs of second choice, which are associated with more adverse effects or have less well-established prophylactic properties. Amitriptyline should be used carefully because of its anticholinergic effects, although it is useful in comorbid tension-type headache, depression, and sleep disorders. Methysergide is very effective, but it has been supplanted or even made unavailable in many countries because of its well-described association with retroperitoneal fibrosis. Pizotifen has a slightly better safety profile but is unavailable in the United States. Aspirin is particularly useful in patients needing platelet inhibitors for other medical conditions, but the risk of gastrointestinal bleeding must be considered. The prophylactic properties of magnesium, riboflavin, and coenzyme Q10 are low at best, but their lack of severe adverse effects makes them good treatment options. Magnesium may be particularly useful during pregnancy. Lisinopril and candesartan were shown to be effective in single trials and are preferable in patients with hypertension. Acupuncture may be another alternative; although controlled trials have failed to differentiate its effect from placebo, it is at least innocuous. Botulinum toxin A is not effective in the prophylaxis of episodic migraine.
Similar content being viewed by others
References and Recommended Reading
Lipton RB, Bigal ME, Diamond M, et al.: Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007, 68:343–349.
Limmroth V, Michel MC: The prevention of migraine: a critical review with special emphasis on beta-adrenoceptor blockers. Br J Clin Pharmacol 2001, 52:237–243.
Holroyd KA, Penzien DB, Cordingley GE: Propranolol in the management of recurrent migraine: a meta-analytic review. Headache 1991, 31:333–340.
Solomon GD, Steel JG, Spaccavento LJ: Verapamil prophylaxis of migraine: a double-blind, placebo-controlled study. JAMA 1983, 250:2500–2502.
Brandes J, Saper J, Diamond M, et al.: Topiramate for migraine prevention: a randomized controlled trial. JAMA 2004, 291:965–973.
Diener HC, Tfelt-Hansen P, Dahlöf C, et al.: Topiramate in migraine prophylaxis: results from a placebo-controlled trial with propranolol as an active control. J Neurol 2004, 251:943–950.
Silberstein SD, Neto W, Schmitt J, et al.: Topiramate in migraine prevention: results of a large controlled trial. Arch Neurol 2004, 61:490–495.
Limmroth V, Biondi D, Pfeil J, Schwalen S: Topiramate in patients with episodic migraine: reducing the risk for chronic forms of headache. Headache 2007, 47:13–21.
Diener HC, Bussone G, Van Oene J, et al.: Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study. Cephalalgia 2007, 27:814–823.
Silberstein SD, Lipton RB, Dodick DW, et al.: Efficacy and safety of topiramate for the treatment of chronic migraine: a randomized, double-blind, placebo-controlled trial. Headache 2007, 47:170–180.
Silberstein SD, Feliu AL, Rupnow MF, et al.: Topiramate in migraine prophylaxis: long-term impact on resource utilization and cost. Headache 2007, 47:500–510.
Steiner TJ, Findley LJ, Yuen AWC: Lamotrigine versus placebo in the prophylaxis of migraine with and without aura. Cephalalgia 1997, 17:109–112.
Lampl C, Katsarava Z, Diener HC, Limmroth V: Lamotrigine reduces migraine aura and migraine attacks in patients with migraine with aura. J Neurol Neurosurg Psychiatry 2005, 76:1730–1732.
Mathew NT, Rapoport A, Saper J, et al.: Efficacy of gabapentin in migraine prophylaxis. Headache 2001, 41:119–128.
Drake ME Jr, Greathouse NI, Renner JB, Armentbright AD: Open-label zonisamide for refractory migraine. Clin Neuropharmacol 2004, 27:278–280.
Pakalnis A, Kring D: Zonisamide prophylaxis in refractory pediatric headache. Headache 2006, 46:804–807.
Ashkenazi A, Benlifer A, Korenblit J, Silberstein SD: Zonisamide for migraine prophylaxis in refractory patients. Cephalalgia 2006, 26:1199–1202.
Silberstein SD: Methysergide. Cephalalgia 1998, 18:421–435.
Cerbo R, Casacchia M, Formisano R, et al.: Flunarizinepizotifen single-dose double-blind cross-over trial in migraine prophylaxis. Cephalalgia 1986, 6:15–18.
Diener HC, Hartung E, Chrubasik J, et al.: A comparative study of acetylsalicyclic acid and metoprolol for the prophylactic treatment of migraine. A randomised, controlled, double-blind, parallel group phase III study. Cephalalgia 2001, 21:140–144.
Welch KMA: Naproxen sodium in the treatment of migraine. Cephalalgia 1986, 6:85–92.
Couch JR, Hassanein RS: Amitriptyline in migraine prophylaxis. Arch Neurol 1979, 36:695–699.
Ziegler DK, Hurwitz A, Hassanein RS, et al.: Migraine prophylaxis. A comparison of propranolol and amitriptyline. Arch Neurol 1987, 44:486–489.
Ozyalcin SN, Talu GK, Kiziltan E, et al.: The efficacy and safety of venlafaxine in the prophylaxis of migraine. Headache 2005, 45:144–152.
Kuritzky A, Zoldan Y, Melamed E: Selegeline, a MAO B inhibitor, is not effective in the prophylaxis of migraine without aura—an open study. Headache 1992, 32:416.
Moja PL, Cusi C, Sterzi RR, Canepari C: Selective serotonin re-uptake inhibitors (SSRIs) for preventing migraine and tension-type headaches. Cochrane Database Syst Rev 2005:CD002919.
Schrader H, Stovner LJ, Helde G, et al.: Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomised, placebo controlled, crossover study. BMJ 2001, 322:19–22.
Tronvik E, Stovner L, Helde G, et al.: Prophylactic treatment of migraine with an angiotensin II receptor blocker: a randomized controlled trial. JAMA 2003, 289:65–69.
Charles JA, Jotkowitz S, Byrd LH: Prevention of migraine with olmesartan in patients with hypertension/prehypertension. Headache 2006, 46:503–507.
Grossmann M, Schmidramsl H: An extract of Petasites hybridus is effective in the prophylaxis of migraine. Inter J Clin Pharmacol Therapeutics 2000, 38:430–435.
Diener HC, Rahlfs VW, Danesch U: The first placebo-controlled trial of a special butterbur root extract for the prevention of migraine: reanalysis of efficacy criteria. Eur Neurol 2004, 51:89–97.
Lipton RB, Gobel H, Einhaupl KM, et al.: Petasites hybridus root (butterbur) is an effective preventive treatment for migraine. Neurology 2004, 63:2240–2244.
Diener HC, Pfaffenrath V, Schnitker J, et al.: Efficacy and safety of 6.25 mg t.i.d. feverfew CO2-extract (MIG-99) in migraine prevention—a randomized, double-blind, multicentre, placebo-controlled study. Cephalalgia 2005, 25:1031–1041.
Pfaffenrath V, Diener HC, Fischer M, et al.: on behalf of the Investigators. The efficacy and safety of Tanacetum parthenium (feverfew) in migraine prophylaxis—a double-blind, multicentre, randomized placebo-controlled dose-response study. Cephalalgia 2002, 22:523–532.
Palevitch D, Earon G, Carasso R. Feverfew (Tanacetum parthenium) as a prophylactic treatment for migraine—a double-blind placebo-controlled study. Phytother Res 1997, 11:508–511.
Murphy JJ, Heptinstall S, Mitchell JRA: Randomized double-blind placebo-controlled trial of feverfew in migraine prevention. Lancet 1988, 2:189–192.
Johnson ES, Kadam NP, Hylands DM, Hylands PJ: Efficacy of feverfew as a prophylactic treatment of migraine. BMJ 1985, 291:569–573.
Peikert A, Wilimzig C, Köhne-Volland R: Prophylaxis of migraine with oral magnesium: results from a prospective, multi-center, placebo-controlled and double-blind randomized study. Cephalalgia 1996, 16:257–263.
Pfaffenrath V, Wessely P, Mener C, et al.: Magnesium in the prophylaxis of migraine—a double-blind placebo-controlled study. Cephalalgia 1996, 16:436–440.
Schoenen J, Jacquy J, Lenaerts M: Effectiveness of high-dose riboflavin in migraine prophylaxis-a randomized controlled trial. Neurology 1998, 50:466–470.
Sandor PS, Di Clemente L, Coppola G, et al.: Efficacy of coenzyme Q10 in migraine prophylaxis: a randomized controlled trial. Neurology 2005, 64:713–715.
Magis D, Ambrosini A, Sandor P, et al.: A randomized double-blind placebo-controlled trial of thioctic acid in migraine prophylaxis. Headache 2007, 47:52–57.
Aurora SK, Gawel M, Brandes JL, et al.: Botulinum toxin type A prophylactic treatment of episodic migraine: a randomized, double-blind, placebo-controlled exploratory study. Headache 2007, 47:486–499.
Elkind AH, O’Carroll P, Blumenfeld A, et al.: A series of three sequential, randomized, controlled studies of repeated treatments with botulinum toxin type A for migraine prophylaxis. J Pain 2006, 7:688–696.
Evers S, Vollmer-Haase J, Schwaag S, et al.: Botulinum toxin A in the prophylactic treatment of migraine—a randomized, double-blind, placebo-controlled study. Cephalalgia 2004, 24:838–843.
Relja M, Poole AC, Schoenen J, et al.: A multicentre, double-blind, randomized, placebo-controlled, parallel group study of multiple treatments of botulinum toxin type A (BoNTA) for the prophylaxis of episodic migraine headaches. Cephalalgia 2007, 27:492–503.
Silberstein S, Mathew N, Saper J, Jenkins S: Botulinum toxin type A as a migraine preventive treatment. For the BOTOX Migraine Clinical Research Group. Headache 2000, 40:445–450.
Diener HC, Kronfeld K, Boewing G, et al.: Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomised controlled clinical trial. Lancet Neurol 2006, 5:310–316.
Linde K, Streng A, Jurgens S, et al.: Acupuncture for patients with migraine: a randomized controlled trial. JAMA 2005, 293:2118–2125.
Alecrim-Andrade J, Maciel-Junior JA, Cladellas XC, et al.: Acupuncture in migraine prophylaxis: a randomized shamcontrolled trial. Cephalalgia 2006, 26:520–529.
Ernst E: Homeopathic prophylaxis of headaches and migraine? A systematic review. J Pain Symptom Manage 1999, 18:353–357.
Campbell J, Penzien DB, Wall EM: Evidence-based guidelines for migraine headache: behavioral and physical therapy. Available at http://www.aan.com/professionals/practice/pdfs/gl0089.pdf. Accessed July 2007.
Köseoglu E, Akboyraz A, Soyuer A, Ersoy AO: Aerobic exercise and plasma beta endorphin levels in patients with migrainous headache without aura. Cephalalgia 2003, 23:972–976.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schürks, M., Diener, HC. & Goadsby, P. Update on the prophylaxis of migraine. Curr Treat Options Neurol 10, 20–29 (2008). https://doi.org/10.1007/s11940-008-0003-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-008-0003-3