Abstract
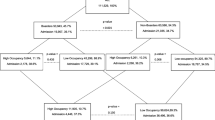
The objective of the study is to determine the association between emergency department (ED) crowding and preventable medical errors (PME). This was a retrospective cohort study of 533 ED patients enrolled in the National ED Safety Study (NEDSS) in four Massachusetts EDs. Individual patients’ average exposure to ED crowding during their ED visit was compared with the occurrence of a PME (yes/no) for the three diagnostic categories in NEDSS: acute myocardial infarction, asthma exacerbation, and dislocation requiring procedural sedation. To accommodate site-to-site differences in available administrative data, ED crowding was measured using one of three previously validated crowding metrics (ED Work Index, ED Workscore, and ED Occupancy). At each site, the continuous measure was placed into site-specific quartiles, and these quartiles then were combined across sites. We found that 46 (8.6%; 95% confidence interval, 6.4–11.3%) of the 533 patients experienced a PME. For those seen during higher levels of ED crowding (quartile 4 vs. quartile 1), the occurrence of PMEs was more than twofold higher, both on unadjusted analysis and adjusting for two potential confounders (diagnosis, site). The association appeared non-linear, with most PMEs occurring at the highest crowding level. We identified a direct association between high levels of ED crowding and risk of preventable medical errors. Further study is needed to determine the generalizability of these results. Should such research confirm our findings, we would suggest that mitigating ED crowding may reduce the occurrence of preventable medical errors.
Similar content being viewed by others
References
Bernstein SL, Aronsky D, Duseja R et al (2009) The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 16:1–10
Sills MR, Fairclough D, Ranade D et al (2011) Emergency department crowding is associated with decreased quality of care for children with acute asthma. Ann Emerg Med 57:191–200
Pitts SR, Niska RW, Xu J et al (2008) National Hospital Ambulatory Medical Care Survey: 2006 Emergency Department Summary. National Center for Health Statistics, Hyattsville, MD
Pines JM, Hollander JE (2008) Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med 51:1–5
Hwang U, Richardson L, Livote E et al (2008) Emergency department crowding and decreased quality of pain care. Acad Emerg Med 15:1248–1255
Fee C, Weber EJ, Maak CA et al (2007) Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med 50:501–509, 509.e1
Pines JM, Localio AR, Hollander JE (2007) The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med 50:510–516
Pines JM, Prabhu A, Hilton JA et al (2010) The effect of emergency department crowding on length of stay and medication treatment times in discharged patients with acute asthma. Acad Emerg Med 17:834–839
Kulstad EB, Hart KM, Waghchoure S (2010) Occupancy rates and emergency department work index scores correlate with leaving without being seen. West J Emerg Med 11:324–328
Chalfin DB, Trzeciak S, Likourezos A et al (2007) Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med 35:1477–1483
Sprivulis PC, Da Silva J, Jacobs IG et al (2006) The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust 184:208–212
Richardson DB (2006) Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust 184:213–216
Pines JM, Pollack CV, Diercks DB et al (2009) The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Acad Emerg Med 16:617–625
Liu SW, Thomas SH, Gordon JA et al (2009) A pilot study examining undesirable events among emergency department-boarded patients awaiting inpatient beds. Ann Emerg Med 54:381–385
Vincent C, Simon R, Sutcliffe K et al (2000) Errors conference: executive summary. Acad Emerg Med 7:1180–1182
White AA, Wright SW, Blanco R et al (2004) Cause-and-effect analysis of risk management files to assess patient care in the emergency department. Acad Emerg Med 11:1035–1041
Friedman SM, Provan D, Moore S et al (2008) Errors, near misses and adverse events in the emergency department: what can patients tell us? CJEM 10:421–427
Sullivan AF, Camargo CA Jr, Cleary PD et al (2007) The National Emergency Department Safety Study: study rationale and design. Acad Emerg Med 14:1182–1189
Ryan TJ, Antman EM, Brooks NH et al (1999) 1999 update: ACC/AHA guidelines for the management of patients with acute myocardial infarction: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation 100:1016–1030
National Heart Lung and Blood Institute (1997) National Asthma Education and Prevention Program Expert Panel Report 2: guidelines for the diagnosis and management of asthma. National Heart, Lung, and Blood Institute, Bethesda, MD
American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists (2002) Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology 96:1004–1017
Burstin HR, Conn A, Setnick G et al (1999) Benchmarking and quality improvement: the Harvard Emergency Department Quality Study. Am J Med 107:437–439
Saketkhou BB, Conet FJ, Noris M et al (1997) Emergency department use of aspirin in patients with possible acute myocardial infarction. Ann Intern Med 127:126–129
Magid DJ, Calonge BN, Rumsfeld JS et al (2000) Relation between hospital primary angioplasty volume and mortality for patients with acute MI treated with primary angioplasty vs thrombolytic therapy. JAMA 284:131–138
Pope JH, Aufderheide TP, Ruthazer R et al (2000) Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med 342:1163–1170
Mehta RH, Eagle KA (2000) Missed diagnoses of acute coronary syndromes in the emergency room—continuing challenges. N Engl J Med 342:1207–1210
Gurwitz JH, Gore JM, Goldberg RJ et al (1998) Risk for intracranial hemorrhage after tissue plasminogen activator treatment for acute myocardial infarction. Ann Intern Med 129:597–604
Emond SD, Woodruff PG, Lee EY et al (1999) Effect of an emergency department asthma program on acute asthma care. Ann Emerg Med 34:321–325
Bernstein SL, Verghese V, Leung W et al (2003) Development and validation of a new index to measure emergency department crowding. Acad Emerg Med 10:938–942
Epstein SK, Tian L (2006) Development of an emergency department work score to predict ambulance diversion. Acad Emerg Med 13:421–426
Hoot NR, Zhou C, Jones I et al (2007) Measuring and forecasting emergency department crowding in real time. Ann Emerg Med 49:747–755
McCarthy ML, Aronsky D, Jones ID et al (2008) The emergency department occupancy rate: a simple measure of emergency department crowding? Ann Emerg Med 51:15–24
Hoot NR, Zhou C, Jones I et al (2007) Measuring and forecasting emergency department crowding in real time. Ann Emerg Med 49:747–755
Pines JM, McCarthy ML (2011) The crowding-effectiveness link: it doesn’t matter how fast we deliver care if we don’t deliver it right. Ann Emerg Med 57:201–202
Croskerry P, Sinclair D (2001) Emergency medicine: a practice prone to error? CJEM 3:271–276
Kohn LT, Corrigan J, Donaldson MS, Institute of Medicine (U.S.) Committee on Quality of Health Care in America (2000) To err is human: building a safer health system. National Academy Press, Washington, DC
Rothschild JM, Churchill W, Erickson A et al (2010) Medication errors recovered by emergency department pharmacists. Ann Emerg Med 55:513–521
Croskerry P, Shapiro M, Campbell S et al (2004) Profiles in patient safety: medication errors in the emergency department. Acad Emerg Med 11:289–299
Campbell SG, Croskerry P, Bond WF (2007) Profiles in patient safety: a “perfect storm” in the emergency department. Acad Emerg Med 14:743–749
Acknowledgments
We gratefully acknowledge the contribution of Dr. David Blumenthal to the NEDSS study that made this work possible, and of Dr. Sharolyn Medina, Director of Clinical Informatics, Picis, Inc. for her assistance with data extraction. We gratefully acknowledge the support of the Riggs Family/Emergency Medicine Foundation Health Policy Grant (Dallas, TX). The National ED Safety Study was supported by grant 5 R01 HS013099 from the Agency for Healthcare Research and Quality (Rockville, MD).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Epstein, S.K., Huckins, D.S., Liu, S.W. et al. Emergency department crowding and risk of preventable medical errors. Intern Emerg Med 7, 173–180 (2012). https://doi.org/10.1007/s11739-011-0702-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-011-0702-8